Translate this page into:
Essential programme on immunization in WHO South-East Asia: A five-decade journey of saving millions of lives & ending diseases
For correspondence: Dr Rahul Srivastava, World Health Organization, South-East Asia Region, New Delhi 110 002, India email: srivastavar@who.int
-
Received: ,
Accepted: ,
Abstract
Vaccination is one of the most successful and cost-effective interventions designed by science which has helped in preventing millions of deaths, especially in children. The Expanded Programme on Immunization (EPI) was established by World Health Organization (WHO) in 1974 to develop immunization programmes throughout the world with polio, measles, diphtheria, tetanus, tuberculosis and whooping cough. The WHO South-East Asia Region (SEAR) has a disproportionately high burden of infectious diseases and has greatly benefitted from the EPI as compared to other regions with more than 90 per cent of the population having access to vaccines. The story of vaccines in South-East Asia is a testament to scientific progress, global collaboration, and unwavering commitment to public health. This article aims to discuss the journey of EPI in the WHO SEAR.
Keywords
Diseases
EPI
essential programme on immunization
expanded programme on immunization
immunization
South-East Asia
vaccination
vaccines
Vaccination is among the most cost-effective interventions which has been successful in saving millions of lives, especially in children1. Return on investment in context to immunization is an estimated US$ 54 for every dollar spent2. Since the implementation of the intensified smallpox eradication programme in 1967, the scope of immunization has grown significantly. It now impacts 14 out of 17 Sustainable Development Goals (SDGs), both directly and indirectly, and extends beyond the prevention of infectious diseases to include global health security, antimicrobial resistance (AMR), pandemic preparedness, and cancer prevention3.
The Expanded Programme on Immunization (EPI, now the Essential Programme on Immunization)4 was launched by the World Health Organization (WHO) with an aim to expand the immunization programmes throughout the world. The first few diseases targeted by the EPI were polio, measles, diphtheria, tetanus, whooping cough and tuberculosis. Before the launch of EPI, vaccination coverage for these diseases in children was estimated to be less than five per cent globally5. EPI, initially launched with the target to prevent six childhood diseases, has since evolved and now covers vaccination across the life course. It now covers 13 universally recommended vaccines among all age groups and 17 additional vaccines6. Every country across the world today has a national immunization programme.
The first major milestone after the launch of EPI was marked by the eradication of smallpox in 1980. Though the EPI cannot be credited for the eradication of smallpox, this has been followed by several other major achievements which includes the entire world becoming free from wild poliovirus except two countries – Afghanistan and Pakistan7. Globally, all countries except 10, have achieved maternal and neonatal tetanus elimination which includes three out of six regions8. Measles has been eliminated from 83 countries as of end of 20229. Apart from these, there are several other vaccine preventable diseases which have been controlled through the vaccination efforts. In 2024, as we mark 50 years of EPI, it is estimated that 3.5 to 5 million deaths are averted every year due to vaccination with a total of 154 million deaths have been averted till now globally10. Furthermore, over the last 50 years, EPI has made the most significant contribution to improving infant survival with 40 per cent recorded decline in the global infant mortality and thus ensuring a child under <10 yr age is 40 per cent more likely to survive up to their next birthday compared to a no vaccination scenario11.
The WHO South-East Asia Region (SEAR) is home to a quarter of the world’s population comprising of 11 countries (viz. Bhutan, Bangladesh, DPR Korea, Myanmar, Maldives, Indonesia, Nepal, India, Sri Lanka, Timor-Leste and Thailand) bears a disproportionately high burden of infectious disease at 28 per cent12, has equally benefitted from the EPI as compared to other regions with more than 90 per cent of the population having access to vaccines13. With this background, the article aims to reflect on the journey of EPI in the WHO SEAR.
EPI progress in the WHO SEAR since 1974
The region has a population of approximately 2.1 billion, a birth cohort of 36 million, and manages 41 million pregnant women each year. When EPI began in the 1970s, the birth cohort totaled to about 30 million due to the region’s high birth rates despite its low population14.
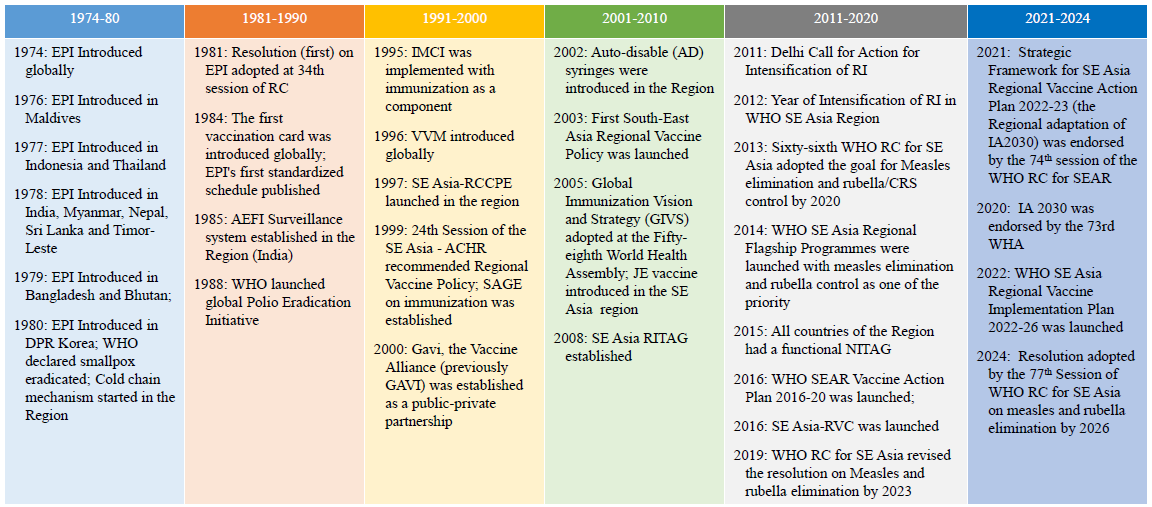
EPI was launched in the countries of WHO SEAR from 1976-80 (Fig. 1). It started with six vaccines and gradually various vaccines were added to the programme including measles containing vaccine (MCV) (1984-85), Hep B (1993-2003), MCV 2 (2007-09), pentavalent and JE vaccine (2009–15), rotavirus (2010-15) and IPV and PCV (2015-17) (Table I). In 1981, the first resolution on EPI was adopted in this during the 34th session of the WHO SEAR Committee meeting15.
- Enablers for strengthening immunization programme in the WHO SEAR. Source: Adapted based on the information available on WHO SEARO website.
| Pathogen | Total deaths averted 1974-2024 | Total YFH gained 1974-2024 | ||
|---|---|---|---|---|
| All ages | Under 5s | All ages | Under 5s | |
| Diphtheria |
81,000 [78,000 - 85,000] |
73,000 [71,000 - 77,000] |
5,430,000 [5,295,000 - 5,552,000] |
4,900,000 [4,777,000 - 5,010,000] |
| Haemophilus influenzae type B |
601,000 [592,000 - 603,000] |
601,000 [592,000 - 603,000] |
43,365,000 [42,495,000 - 43,593,000] |
43,365,000 [42,495,000 - 43,593,000] |
| Hepatitis B |
73,000 [70,000 - 75,000] |
57,000 [55,000 - 58,000] |
10,486,000 [10,184,000 - 10,721,000] |
8,158,000 [7,923,000 - 8,341,000] |
| Japanese encephalitis |
20,000 [19,000 - 20,000] |
14,000 [13,000 - 14,000] |
2,151,000 [2,110,000 - 2,188,000] |
1,481,000 [1,453,000 - 1,506,000] |
| Measles |
20,517,000 [19,996,000 - 21,083,000] |
20,194,000 [19,682,000 - 20,752,000] |
1,264,122,000 [1,228,062,000 - 1,299,750,000] |
1,244,255,000 [1,208,762,000 - 1,279,324,000] |
| Pertussis |
4,428,000 [4,307,000 - 4,527,000] |
3,910,000 [3,814,000 - 3,991,000] |
366,568,000 [353,197,000 - 376,230,000] |
323,138,000 [311,714,000 - 331,301,000] |
| Poliomyelitis |
347,000 [347,000 - 347,000] |
196,000 [196,000 - 196,000] |
168,577,000 [168,577,000 - 168,577,000] |
95,333,000 [95,333,000 - 95,333,000] |
| Rotavirus |
62,000 [61,000 - 64,000] |
62,000 [61,000 - 64,000] |
4,150,000 [4,093,000 - 4,200,000] |
4,150,000 [4,093,000 - 4,200,000] |
| Rubella |
112,000 [105,000 - 117,000] |
0 [0 - 0] |
8,410,000 [7,891,000 - 8,955,000] |
0 [0 - 0] |
| Streptococcus pneumoniae |
137,000 [134,000 - 138,000] |
137,000 [134,000 - 138,000] |
10,091,000 [9,865,000 - 10,167,000] |
10,091,000 [9,865,000 - 10,167,000] |
| Tetanus |
9,237,000 [8,939,000 - 9,485,000] |
8,883,000 [8,595,000 - 9,121,000] |
503,183,000 [482,237,000 - 518,767,000] |
477,844,000 [458,221,000 - 492,382,000] |
| Tuberculosis |
2,416,000 [2,397,000 - 2,434,000] |
1,704,000 [1,690,000 - 1,716,000] |
189,866,000 [188,034,000 - 191,495,000] |
133,886,000 [132,594,000 - 135,035,000] |
| Total |
38,030,000 [37,047,000 - 38,979,000] |
35,830,000 [34,904,000 - 36,730,000] |
2,576,398,000 [2,502,041,000 - 2,640,195,000] |
2,346,599,000 [2,277,231,000 - 2,406,191,000] |
Source: Reproduced with permission from Ref 11 (supplementary appendix Table S1 in Ref 11)
The initial focus of EPI was more on childhood vaccination and emphasis was given to this cause. Between 1990 and 2015, the childhood mortality rate in this region decreased by 64 per cent with a decline in infant mortality rate (118/1000 live births and 43/1000 live births in 1990 and 2015, respectively). With time a life course approach has been adopted in the vaccination process including children and adults of all ages16.
The first Regional Vaccine Policy was launched in 2003 with the purpose to provide a framework on research, availability, production, and distribution of vaccines in this region17. This was followed by Regional Vaccine Action Plan 2016-202018 and Strategic Framework for the South-East Asia Regional Vaccine Action Plan 2022−203019 as strategic guidance documents. The most recent Regional Vaccine Implementation plan (2022-2026), based on three impact goals and seven strategic priorities, focuses on increasing equitable access to routine immunization, and reducing vaccine preventable diseases (VPDs) related mortality and morbidity across life cycle20.
In 2008, the Regional Immunization Technical Advisory Group was established, and the first meeting was conducted in New Delhi. By 2015, all countries of the WHO SEAR had a functional National Immunization Technical Advisory Group to provide evidence-based advice to policy makers and programme managers on policy issues related to vaccines and immunization.
Vaccine introduction in the region
By 1980, all the countries in the region had started EPI, which means four EPI vaccines targeting six VPDs were introduced in the WHO SEAR. However, Bangladesh (OPV in 1953), India (BCG-1948 and OPV in 1972) and Sri Lanka (BCG in 1959, DPT in 1961, and OPV in 1962) had already introduced EPI vaccines before the launch of EPI in their respective countries (Table II). With time various other vaccines were added to the EPI as per the requirement as and when these were validated.
| OPV | BCG | DPT | Measles | Hep B | Penta | MCV2 | Rubella | IPV | Rota VV | JEV | COVID-19 | PCV | TCV | HPV | Hepatitis B BD | IPV2 | DTP booster | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Bangladesh | 1979 | 1979 | 1979 | 1982 | 2003 | 2009 | 2000 | 2012 | 2015 | 2021 | 2015 | 2023* | 2017 | |||||
| Bhutan | 1979 | 1979 | 1979 | 1980 | 1997 | 2009 | 2010 | 2008 | 2015 | 2021 | 2019 | 2011 | 2012 | 2022 | 2013 | |||
| DPR Korea | 1980 | 1980 | 1980 | 1980 | 2003 | 2012 | 2008 | 2019 | 2015 | 2004 | ||||||||
| India | 1972 | 1948 | 1978 | 1985 | 2023 | 2011 | 2010 | 2017 | 2015 | 2016 | 2007 | 2021 | 2017 | 2016* | 2007 | 2015 | 1995 | |
| Indonesia | 1977 | 1977 | 1977 | 1977 | 1997 | 2013 | 2004 | 2017 | 2016 | 2022 | 2018 | 2021 | 2017 | 2016* | 2008 | 2022 | 2013 | |
| Maldives | 1988 | 1971 | 1985 | 1983 | 1993 | 2013 | 2007 | 2017 | 2015 | 2021 | 1993 | 2018 | ||||||
| Myanmar | 1987 | 1978 | 1978 | 1987 | 2003 | 2012 | 2008 | 2015 | 2015 | 2020 | 2017 | 2021 | 2016 | 2020 | 2016 | 2023 | ||
| Nepal | 1978 | 1978 | 1978 | 1979 | 2005 | 2009 | 2015 | 2013 | 2014 | 2020 | 2007 | 2021 | 2015 | 2022 | 2018 | |||
| Sri Lanka | 1962 | 1959 | 1961 | 1984 | 2003 | 2008 | 2003 | 1996 | 2015 | 1988 | 2021 | 2017 | 2016 | |||||
| Thailand | 1982 | 1977 | 1977 | 1984 | 2008 | 2019 | 2000 | 1986 | 2015 | 2020 | 1990 | 2021 | 2021* | 2017 | 1992 | 1995 | ||
| Timor-Leste | 1978 | 1978 | 1978 | 1978 | 2007 | 2012 | 2015 | 2016 | 2016 | 2019 | - | 2021 | 2023 | 2024 | 2016 | 2017 |
Source: Ref 26 (reproduced with permission from WHO Regional office for SEAR)
Six new priority vaccines are scheduled to be introduced in one or more countries of the Region, and this includes pneumococcal conjugate vaccine (PCV), human papillomavirus vaccine (HPV), rotavirus vaccine (RVV), typhoid conjugate vaccine (TCV), Japanese encephalitis vaccine (JEV), and COVID-19 vaccines. Other important existing vaccines are inactivated polio second dose (IPV2), DTP booster and hepatitis birth dose.
Vaccination coverage of EPI vaccines in the WHO SEAR
The graph below shows the trend of different vaccines in the region from 1980 to 2022. The coverage of all the vaccines has been increasing with time but most of the vaccines are still below 90 per cent coverage in this region (Fig. 2).
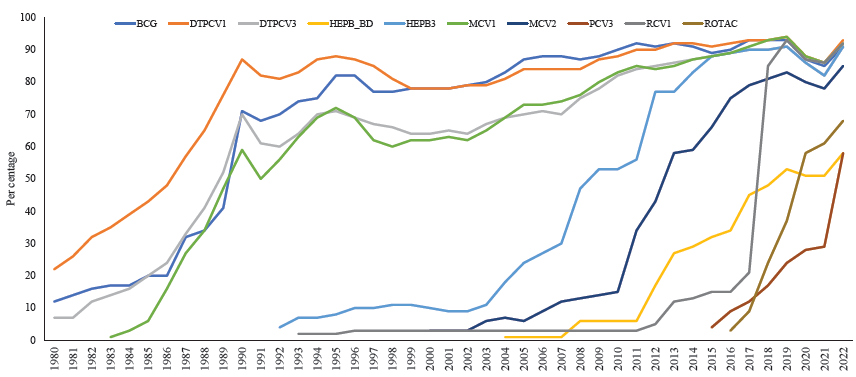
- Trend of routine immunization coverage in WHO South-East Asia region (1980-2022). Source: Reproduced with permission from WHO Regional office for SEAR (https://immunizationdata.who.int/).
The coverage of DPT3 was only seven per cent in this region in 1980 but increased to 64 per cent in 2000 and crossed 90 per cent in 2017. Maldives (1989), Thailand (1990) and Sri Lanka (1993) were the first countries to touch the DTP3 coverage of 90 per cent for the first time and this was followed by Myanmar (1997), Bangladesh (2004), DPR Korea (2007), Nepal (2011) and India in 201821.
The MCV2 vaccine was introduced in the region since 2000, and the estimated coverage was only three per cent which increased to 85 per cent in 2022. Similarly, the IPV vaccine was started in WHO SEAR in 2015 with eight per cent coverage and the coverage increased to 88 per cent in 2022. Hepatitis B vaccine - birth dose, introduced in 2004, however, the coverage is still only 58 per cent21.
Impact (mortality and morbidity) of EPI
Since 1974, significant advances in childhood survival have been added in all geographical regions. As per the latest estimates, over the last 50 yr, EPI has made the most significant contribution to improving infant survival10.
In WHO SEAR, over the last 50 yr (June 1974, and May 2024) vaccination programmes under EPI targeting 14 modeled pathogens are recorded to have averted around 38 million deaths (global 154 million deaths averted), including 36 million (global 145 million under 5 deaths averted) in children <5 yr11. This means 2.6 billion yr of full health (i.e., disability-adjusted life-year averted) was gained during this period in the WHO SEAR (Table I). The greatest contribution to the deaths averted is due to measles vaccination which saved 20·5 million lives (54 per cent of the 38 million total lives saved) over this 50-yr period. This was followed by 9.2 million lives saved due to tetanus vaccination11.
Since 1974, global and regional infant mortality has declined substantially and vaccines reportedly contributed for 40 per cent of this decline, while in the WHO SEAR, 22 per cent of the decline in infant mortality was attributed to vaccination11.
Strengthened immunization system in the region
Cold chain management in immunization
As the EPI progressed in this region, there was a need to strengthen this cold chain system for storage and transportation of vaccine. Iced-Line Refrigerator (ILR) was included in the cold chain and worked well in places with at least 8h of electricity supply ‘end-to-end’ with a temperature monitoring system. For transportation purposes, high-performance vaccine cold boxes as well as carriers were developed in 197922. In the early 1980s, cold chain monitor card was developed, and vaccine vial monitors (VVM) was developed in 1996, which ensured the quality of vaccines delivered. Now real time monitoring of the temperature is available which provides continuous temperature update. Also, emphasis is being given to alternate sources of energy and 50 per cent of all the vaccine fridges installed by UNICEF around the world since 2017 are solar-powered23.
In 1980, cold chain equipment produced locally in the countries of the WHO SEARO were tested for their ‘cold life’. In India and Maldives, solar powered refrigerators were tested for storing vaccines15. Regional cold stores were installed for vaccines15. Gradually the region became equipped to produce cold chain equipment and now cold chain infrastructure and management capacities in this region have improved significantly. India alone has more than 29,000 cold chain points24.
The progress in EPI in building systems like cold chain and workforce enabled COVID-19 vaccines to be rapidly rolled out globally and showed its capacity to respond to emerging health crises25. More than three billion doses of COVID-19 vaccines were deployed in the WHO SEAR. Existing manpower was rapidly trained, and vaccination sessions were conducted in the normal routine immunization clinic. During the COVID pandemic, subnational and national cold chain capacities in the region were increased rapidly. Ultracold chain equipment were set up in the region to accommodate COVID-19 vaccines in 2021 and Bangladesh and Indonesia have 26 and 17 ultracold chain equipment, respectively.
Vaccine preventable disease surveillance
Strong VPD surveillance system is central to the immunization success story. VPD surveillance for polio was conducted via the acute flaccid paralysis surveillance (AFP). Between 2006 and 2016, more than half a million children aged 15 yr were investigated for polio, and approximately one million stool samples were tested in the laboratory26. Polio eradication was possible due to rigorous monitoring to detect and examine all cases of polio-like acute flaccid paralysis (AFP). Now, the surveillance is done for the vaccine associated polio diseases in the region. Also, polio transition plan integrates critical functions and infrastructure established by the polio eradication programme into the national health system.
A similar surveillance approach was adopted for measles and rubella. All eleven member countries in this region have also adopted the ‘Acute fever and maculopapular rash’ surveillance. The sensitivity of this surveillance has improved (non-measles non-rubella (NMNR) discard rate -2.86 per 100,000 population as of 2022), after suffering slight decrease during the pandemic. NMNR discard rate of ≥2 per 1000 population has been achieved by more than 50 per cent of the districts in the WHO SEARO countries25. Surveillance is done for many other vaccine preventable diseases like haemophilus influenza, rabies, Japanese encephalitis, typhoid, cholera, etc.
Strategic guidance and partnership for successful implementation of EPI
WHO has initiated many policies to enable successful implementation of EPI. The Global Vaccine Action Plan (GVAP) was started in May 2012 and aimed to prevent millions of deaths by 2020 by ensuring equitable access to existing vaccines. The WHO SEAR adopted the Immunization Agenda 2030 strategy according to the regional context in the form of the Regional Vaccine Implementation Plan (RVIP) 2022-26 which provides details regarding the implementation of the regional strategic framework in the countries. The plan focuses on the implementation in countries on the basis of national health level policies, immunization strategies, and multi yr plans. Annual workplans would be developed with specific activities with fixed timelines and a continuous quality improvement cycles will be followed.
The WHO SEAR has shown a strong commitment and has resolved to further the agenda on EPI through various resolutions. Some major accountability and commitment mechanisms included formation of National Immunization Technical Advisory Groups (NITAGs), Regional Technical Advisory Groups on Immunization (RITGS), Regional Certification Commission for Polio Eradication (RCCPE), National Certification Commission for Polio Eradication (NCCPE) and, Regional Verification Commissions (RCV) and National Verification Commission (NVC) for measles and rubella elimination (Fig. 1). All countries have increased national expenditure on vaccines and most of the countries in WHO SEAR are dependent more on self-funding inter-agency coordination committees (ICCs) have been formed in the Gavi, the Vaccine Alliance, eligible countries, which ensure the involvement of all stakeholders in planning, implementation and monitoring of national immunization programmes20.
Vaccine manufacturing and regulatory aspects
South-East Asia produces about 46 per cent of global vaccine supply with about 3.8 billion doses being manufactured in India, one billion in Indonesia, 100 million in Thailand and 144 million in Bangladesh27. There are two major vaccine producers in the region, Serum Institute of India and Biofarma in Indonesia28,29. Thailand and Bangladesh are also producing significant number of vaccines lately.
WHO has published standards/guidelines on the quality, safety and efficacy of vaccines and medicine, and regulatory assessment of approved products, which help in regulation of the vaccines. Except Timor-Leste, all the National Regulatory Authorities (NRAs) in WHO SEAR have conducted formal assessments of their vaccine regulatory systems using the standardized WHO assessment tools. NRAs in India, Thailand and Indonesia have been functional since 2008. Other countries, such as Sri Lanka and Nepal, imported vaccines through government procurement agencies, or through UNICEF procurement agencies, due to the NRA’s limited capacity to regulate vaccines.
AEFI surveillance
One major challenge in EPI is to ensure immunization monitoring and safety of adverse events following immunization (AEFI). Since 2008, training workshops have been organized in several countries of WHO SEAR, resulting in increase in detection and reporting of AEFIs.
Although published guidelines for monitoring AEFIs are available their enforcement varies widely from one country to another. For instance, Bangladesh, Indonesia and India have established several subnational AEFI committees to support national committees. However, the sensitivity of AEFI surveillance specific to EPI vaccines needs to be escalated. About 93 per cent of the serious AEFI cases in this region were investigated and causality assessment for only 15 per cent of those was completed in 202225. India, Sri Lanka, and Thailand are primarily lagging in assessing causality for significant AEFIs. There has been a decline in the AEFI reports from 2019 to 2022 in this region, excepting Sri Lanka25. Timely completion of causality assessment is still difficult in India, Sri Lanka and Thailand. Only four (Bangladesh, India, Indonesia and Thailand) out of 11 countries submit data regularly with Uppsala Monitoring Centre (UMC) through the ViGiBase. Maldives and Nepal have shown interest in sharing data with UMC25.Vaccine safety surveillance has improved, but there is still a long way to go.
Major achievements of EPI
Smallpox was eliminated from this region in 1975 and was declared eradicated from the world in 1980. In 1979, the WHO advised that all vaccinations be discontinued in all countries, with the exception of those working with smallpox viruses. Vaccination in this region continued till 198230. WHO preserved a stock of 200 million doses in 1980, out of 99 per cent was destroyed in the late 1980s when smallpox did not reemerge. Two sites in the USA and Russia, respectively, hold seeds of variola virus for future use31.
Elimination of polio
The WHO SEAR has been polio free since 2014 (Fig. 3). However, the international spread of poliovirus remains a public health emergency since wild polio is still endemic in two countries (Pakistan and Afghanistan)32. Additionally, the cases of vaccine-derived polioviruses (cVDPVs) have also been recorded in several countries32.
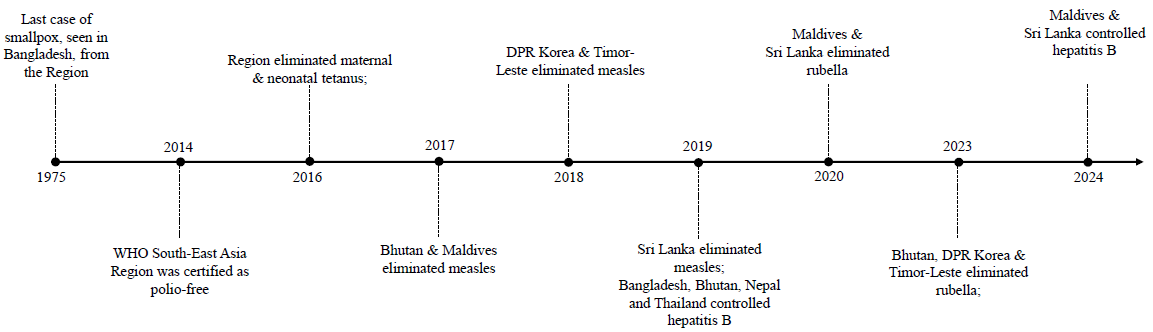
- Major achievements of 50 years of EPI in WHO South-East Asia. Source: Adapted from information available on WHO SEARO website.
Maldives became the first country in WHO SEAR to eliminate Polio in 1983 followed by Bhutan in 1989. The last case of wild poliovirus in this region was reported in January 2011 in India. India was certified as polio free on March 27, 2014. This was made possible by high-quality vaccination campaigns which reached a total of 7.5 billion children >17 yr. Between 1995 and 2012, 189 nationwide campaigns were conducted across the WHO SEAR and >13 billion doses of oral polio vaccine were administered33. Many factors including the AFP surveillance, regional polio laboratory network, and various other risk mitigation activities are responsible for eradication.
Outbreaks were reported due to circulating cVDPV2 in Indonesia in November 2022 and February 2023, respectively. The national programme in Indonesia conducted rapid response vaccination campaigns for > 6 million children. Additional steps were taken to strengthen surveillance and routine immunization34. No additional cVDPVs have been detected in other countries of WHO SEAR so far.
Elimination of maternal & neonatal tetanus
Maternal and neonatal tetanus (MNT) was a major cause of newborn mortality in the WHO SEAR before EPI started. In the 1980s, neonatal tetanus had a case fatality rate of about 87 per cent and about 350,000 neonates died due to neonatal tetanus in this region35. However, the rate of MNT in this region has remained less than one per 1000 live births since 2016 and annual post-validation desk review has confirmed that the MNTE status has been sustained. MNTE has been sustained in the region through optimal implementation of the strategies outlined in the ‘guide to sustaining maternal and neonatal tetanus elimination (MNTE) and broadening tetanus protection for all populations’ which includes routine vaccination of all children/adolescents and strengthening immunization of pregnant women, antenatal screening of pregnant women access to skilled health personnel at the time of birth and hygienic birth/cord care practices; and strong tetanus and neonatal tetanus surveillance and regular data review to identify at risk districts for re-emergence of MNT and needing corrective action36.
Measles and rubella elimination
In 2013, WHO SEAR adopted the regional goal of ‘measles elimination and rubella and congenital rubella syndrome control by 2020’21 and this was designated as one of the priority programmes for this region. This mandated maintenance of more than 95 per cent coverage with two doses of vaccine containing measles and rubella in every district through routine or supplementary immunization activities.
As of July 2023, five countries including (DPR Korea, Bhutan, Maldives, Timor-Leste and Sri Lanka) have achieved the measles and rubella elimination goal. Despite the challenges posed by COVID-19 pandemic, measles containing vaccine (MCV) 1 coverage increased from 85 per cent in 2013 to 91 per cent in 2023 and MCV2 increased from 59 per cent in 2013 to 85 per cent in 202337.
Hepatitis B control
The SEAR houses roughly 60 million people reportedly living with chronic hepatitis B and > 200,000 that die of hepatitis B every year. Only about three per cent are diagnosed <1 per cent are on treatment38. In 2016, WHO SEAR endorsed a goal of hepatitis B control with a target of reduction in hepatitis B prevalence to < 1 per cent among children aged > 5 yr. This pentavalent is now included in the national immunization schedules of all countries. Three doses of the vaccine are provided within the first year of life and a birth dose is provided in eight countries in WHO SEAR. The coverage of third dose of pentavalent vaccine (containing Hep B) was 91 per cent in 2022. In 2019 Bangladesh, Nepal, Bhutan, and Thailand achieved the regional target of hepatitis B control and Maldives and Sri Lanka achieved hepatitis B control in 202439.
The birth dose of hepatitis B is still low in this region (54% in 2019, 51% in 2020 and 2021, 57% in 2023) and this is one of the main challenges in achieving control. Also, due to the COVID-19 pandemic, planned sero-surveillance was postponed in three countries (Maldives, DPR Korea and Sri Lanka)25.
Member States of the WHO South-East Asia has adopted several resolutions to strenghen immunization in the Region and this includes the most recent one (in October 2024) on measles and rubella elimination by 2026 (https://www.who.int/southeastasia/news/detail/10-10-2024-who-south-east-asia-region-sets-new-target-for-measles-and-rubella-elimination). The resolutions have been mentioned in detail in figure 1.
COVID-19 – immunization infrastructure
The progress in EPI facilitated the possibility of a rapid global rollout of COVID-19 vaccines. This also demonstrated its capacity to respond to emerging health crises. This was only made possible due to the system in place including the cold chain management and trained manpower. It was possible to train the existing manpower rapidly and vaccination sessions could be held in the routine immunization clinic. All Governments also made efforts to secure the required vaccine doses through various means like donations, increased manufacturing, and various deals, to ensure successful roll-out. Most of the countries have also initiated efforts to integrate COVID-19 vaccination and routine immunization. Many countries utilized the routine immunization sites for the COVID-19 vaccination as well. Private sector also has a major role in implementation of routine immunization by improving access to vaccines and the same contributed to COVID vaccination as well.
Challenges in implementation of EPI
The Expanded Programme on Immunization (EPI) is encountering a range of emerging challenges which demand responsive strategies and adaptive.
Though supply of vaccines is not a major challenge in the WHO SEAR, delivery and other logistics pertaining to the vaccination sites which are often in the rural areas is a challenge. There should be an adequate monitoring of the vaccine and logistics delivery system. This is important to monitor stockouts at any level. Political conflicts, war like situations, climate change impacts, ecological problems, economic crises, etc in the country poses a major challenge to health programmes in the country and maternal and child health is the first to suffer in such case. Similarly, migration also poses a major challenge in vaccine coverage due to limited access to various health services including routine immunization in the refugee camps and other similar settlements.
Allocation of adequate funds and the financial sustenance of vaccine procurement and other logistics is a challenge in some countries. This limitation is more pronounced in the middle income countries and GAVI graduated countries, due to a decline in resources and external fundings. National budgets now finance a significant percentage of all spending on routine immunization, from 42 per cent in India, and 100 per cent in Maldives and Thailand is caused from the country’s national budget. Expenditure on routine immunization is now covered largely from the national budgets in countries. For example, 29 per cent immunization budget in Bangladesh.
One of the biggest challenges is ensuring the optimal implementation of strategies and ensuring multisector coordination. There is a need to enhance accountability at various levels to ensure optimal programme implementation at national as well as subnational levels. There is also a need to look at digital health technologies. Most of the data platforms use electronic system to record vaccine stock and supply management, VPD surveillance, adverse event reporting, etc. But the success of using electronic systems depends primarily on regular updates and user support. Furthermore, hard to reach and rural areas may have some electricity and network issues, which can affect the data quality. In such cases, virtual training may also not be as effective as compared to a hands-on training where better interaction can be ensured.
Vaccine hesitancy due to social or religious issues remains high in certain areas. This can alter the community perception and make it difficult to vaccinate children. Advocacy at local levels and high political commitment is required to deal with community perception. Area specific communication plans should also be devised with help of community leaders.
All the countries should prioritize screening vaccination of underserved children. The main focus should be on availability of sufficient manpower, vaccine supply and other logistics at the vaccination sites alongside, allocation of adequate funds and financial sustainability for procurement.
Zero dose children refer to those who have never received any routine vaccination and are measured as those who have not received the first dose of DPT vaccine40. As per the latest global data, in 2023 ⁓3.4 million children in the WHO SEAR did not receive all vaccines. Of these 2.7 million did not receive any vaccine, making them vulnerable to life threatening but vaccine preventable diseases. While overall immunization coverage is high, there remain variability in the subnational level coverage in countries, particularly in those with large populations. The inequities in immunization coverage leading to accumulation of pockets of unvaccinated children poses the risk of measles outbreaks, diphtheria, and other vaccine-preventable diseases. While countries in the WHO SEAR have been making notable efforts, with seven countries consistently reaching over 90 per cent children with three doses of diphtheria, pertussis, and tetanus (DTP3) vaccines, the high numbers of missed and under vaccinated children calls for urgent action. One needs to identity where and why these children were missed and prioritize reaching them with tailored approaches to vaccinated them at the earliest41.
While the COVID-19 pandemic brought many challenges including lockdown and restricted movements, high burden on the healthcare system, reluctance of women to attend ANC clinics, lower facility deliveries due to fear of COVID-19, etc., it also caused setbacks in the implementation of EPI worldwide42. It caused unprecedented fallback in immunization with more than 25 million children who remained un-or under-vaccinated in 2021. About 18.2 million of these were zero-dose children which is 6 million more than in 2019. In SEAR, the coverage of pentavalent vaccine (Penta 3) (3 doses) decreased from 91 per cent in 2019 to 86 per cent in 2020 and to 82 per cent in 2021. The number of children who failed to receive the first dose of this vaccine increased from two million in 2019 to 4.6 million in 202126. Although most of the countries have recovered the pandemic gap, Timor-Leste and Nepal still need more efforts to reach the required coverage levels while DPR Korea and Myanmar still require significant recovery. Plans should be made to reach all the zero dose children and vaccinate them so that no one is left behind.
Way forward
Since its inception, EPI has accomplished numerous milestones and established itself as one of the world’s most prominent programmes. Committed to its objective of providing universal access to all relevant vaccines for those at risk, EPI continues to collaborate with other public health programmes to reduce infectious illnesses and improve health for all people worldwide.
In the near future, the primary goal is to ensure optimal implementation of the RVIP 2022-2026 and progress towards achieving the IA 2030 targets. WHO SEAR will require targeted efforts to reach unvaccinated and under-vaccinated children and communities. This will require adoption of advanced vaccine technologies, building on innovations such as mRNA vaccines, and integrate emerging delivery methods to improve immunization reach and efficiency.
Strengthening surveillance systems and embracing digital technologies will be essential. Advanced tools like artificial intelligence, machine learning, and data analytics offer transformative opportunities to improve vaccine equity and optimize programme effectiveness. The future of EPI also lies in its integration with primary health care systems, enhancing service delivery and building vaccine confidence among communities. Equitable access to all vaccines for every individual remains the ultimate goal, underscoring the need for sustained prioritization and investment in immunization. Immunization progress can easily backslide if complacency sets in. Hence, strengthening immunization programmes will be essential not only to prevent outbreaks of vaccine-preventable diseases but also to mitigate the spread of AMR by reducing the need for antibiotic treatments. By addressing climate change impacts and closing coverage gaps, targeted immunization efforts can build more resilient health systems, ensuring equitable vaccine access for vulnerable populations and creating a sustainable impact on public health.
The next 50 yr hold immense potential, but this will require collective, sustained determination to drive EPI forward. Political will, resources and commitment from national to community level will be key to achieving this goal. In the long term, the ultimate goal is to ensure that everyone has equitable access to all vaccines.
Financial support & sponsorship
None.
Conflicts of Interest
None.
Use of Artificial Intelligence (AI)-Assisted Technology for manuscript preparation
The authors confirm that there was no use of AI-assisted technology for assisting in the writing of the manuscript and no images were manipulated using AI.
References
- Chapter 1 - A short history of vaccination. In: Orenstein W, Offit P, Edwards KM, Plotkin S, eds. Plotkin’s Vaccines (8th ed). Philadelphia: Elsevier; 2023. p. :1-16.e9.
- [Google Scholar]
- Global Health Equity Network - Gavi, the Vaccine alliance. Available from: https://initiatives.weforum.org/global-health-equity-network/case-study-details/gavi,-the-vaccine-alliance/aJYTG00000003M54AI, accessed on July 19, 2024.
- Sustainable Development Goals. The 17 Goals. Available from: https://sdgs.un.org/goals, accessed on November 7, 2024.
- Essential programme on immunization. Available from: https://www.who.int/teams/immunization-vaccines-and-biologicals/essential-programme-on-immunization, accessed on October 16, 2024.
- The State of the World’s Children 1989. Available from: https://www.unicef.org/reports/state-worlds-children-1989, accessed on November 7, 2024.
- Celebrating 50 years of immunization progress: honouring achievements, embracing innovation, and envisioning the future. Available from: https://www.who.int/news-room/events/detail/2024/05/28/default-calendar/celebrating-50-years-of-immunization-progress-honouring-achievements-embracing-innovation-and-envisioning-the-future, accessed on July 17, 2024.
- Poliomyelitis. Available from: https://www.who.int/health-topics/poliomyelitis, accessed on October 14, 2024.
- Maternal and neonatal tetanus elimination. . Progress towards global MNT elimination. Available from: https://www.who.int/initiatives/maternal-and-neonatal-tetanus-elimination-(mnte)/progress-towards-global-mnt-elimination, accessed on October 14, 2024.
- Progress toward measles elimination — Worldwide, 2000–2022. MMWR Morb Mortal Wkly Rep. 2023;72:10.
- [Google Scholar]
- Two centuries of vaccination: Historical and conceptual approach and future perspectives. Front Public Health. 2024;11:1326154.
- [Google Scholar]
- Contribution of vaccination to improved survival and health: Modelling 50 years of the expanded programme on immunization. Lancet. 2024;403:2307-16.
- [Google Scholar]
- Communicable diseases in the South-East Asia Region of the World Health Organization: towards a more effective response. Bull World Health Organ. 2010;88:199.
- [Google Scholar]
- South-East Asia. Vaccines and immunization. Available from: https://www.who.int/southeastasia/health-topics/immunization, accessed on July 19, 2024.
- World Birth Rate 1950-2024. Available from: https://www.macrotrends.net/global-metrics/countries/wld/world/birth-rate, accessed on November 7, 2024.
- SEA/RC34/23 - Report of the thirty-fourth session of the WHO Regional Committee for South-East Asia. Available from: https://iris.who.int/ handle/10665/129746, accessed on July 17, 2024.
- South-East Asia. Make focused, accelerated efforts to prevent, reduce newborn deaths: WHO. Available from: https://www.who.int/southeastasia/news/detail/14-12-2015-make-focused-accelerated-efforts-to-prevent-reduce-newborn-deaths-who, accessed on November 7, 2024.
- South-East Asia regional vaccine policy. Available from: https://iris.who.int/bitstream/10665/127129/1/SEA-ACHR-28-09.pdf, accessed on October 10, 2024.
- South-East Asia regional vaccine action plan 2016-2020. Available from: https://iris.who.int/handle/10665/272397, accessed on October 21, 2024.
- Strategic framework for the South-East Asia Regional vaccine action plan 2022−2030 as aligned with the global Immunization Agenda 2030. Available from: https://iris.who.int/handle/10665/343756, accessed on October 21, 2024.
- Immunization Data portal - South-East Asia Region. Available from: https://immunizationdata.who.int/dashboard/regions/south-east-asia-region, accessed on November 7, 2024.
- Regional Vaccine Implementation Plan 2022–2026, WHO South-East Asia Region. Available from: https://www.who.int/publications/i/item/9789290210542, accessed on October 11, 2024.
- The origins of the vaccine cold chain and a glimpse of the future. Vaccine. 2017;35:2115-20.
- [Google Scholar]
- The vaccine cold chain: A history. Available from: https://www.gavi.org/vaccineswork/vaccine-cold-chain-history, accessed on October 31, 2024.
- World’s largest vaccination drive in India: Challenges and recommendations. Health Sci Rep. 2021;4:e355.
- [Google Scholar]
- Asia WHORO for SE. Immunization achievements in South-East Asia: the platform for measles elimination. Available from: https://iris.who.int/handle/10665/258759, accessed on October 14, 2024.
- Fourteenth meeting of the WHO South-East Asia Regional Immunization Technical Advisory Group, 29 August–1 September 2023, New Delhi, India. . Licence: CC BY-NC-SA 3.0 IGO. Available from: https://iris.who.int/handle/10665/258759, accessed on October 14, 2024.
- Global vaccine market report 2023 Update. Available from: https://cdn.who.int/media/docs/default-source/immunization/mi4a/who_gat_008_global_vaccine_market_report_march_12.pdf?sfvrsn=a61f4733_1&download=true, accessed on August 24, 2024.
- About us. Serum-Protection from birth onwards. Available from: https://www.seruminstitute.com/about_us.php, accessed on October 1, 2024.
- The Leading Vaccine Manufacturer in Indonesia. Available from: https://www.biofarma.co.id/, accessed on October 1, 2024.
- Smallpox and its post-eradication surveillance. Available from: https://iris.who.int/handle/10665/264479, accessed on July 17, 2024.
- Smallpox. Available from: https://www.cdc.gov/smallpox/research/index.html, accessed on July 17, 2024
- South East Asia. Polio-free certification: WHO South-East Asia. Available from: https://www.who.int/southeastasia/activities/maintaining-polio-free-status/polio-free-certification-who-south-east-asia, accessed on October 17, 2024.
- South-East Asia Region declared polio-free. Available from: https://polioeradication.org/news-post/who-south-east-asia-region-declared-polio-free/, accessed on July 19, 2024.
- Circulating vaccine-derived poliovirus type 2 - Indonesia. Available from: https://www.who.int/emergencies/disease-outbreak-news/item/2024-DON500, accessed on July 17, 2024.
- Sustaining maternal and neonatal tetanus elimination. Available from: https://www.who.int/southeastasia/activities/sustaining-maternal-and-neonatal-tetanus-elimination, accessed on July 17, 2024.
- Protecting all against tetanus: guide to sustaining maternal and neonatal tetanus elimination (MNTE) and broadening tetanus protection for all populations. Available from: https://iris.who.int/handle/10665/329882, accessed on October 21, 2024.
- Striving to eliminate measles and rubella in the WHO South-East Asia Region. Available from: https://www.who.int/southeastasia/news/feature-stories/detail/striving-to-eliminate-measles-and-rubella-in-the-who-south-east-asia-region, accessed on July 17, 2024.
- Global hepatitis report 2024: action for access in low- and middle-income countries. Available from: https://www.who.int/publications/i/item/9789240091672, accessed on November 7, 2024.
- South-East Asia. . Maldives, Sri Lanka achieve Hepatitis B control. Available from: https://www.who.int/southeastasia/news/detail/17-01-2024-maldives-sri-lanka-achieve-hepatitis-b-control, accessed on July 17, 2024.
- Zero-dose children and missed communities. Available from: https://www.gavi.org/our-alliance/strategy/phase-5-2021-2025/equity-goal/zero-dose-children-missed-communities, accessed on November 7, 2024.
- WHO South-East Asia Region lauds countries for routine immunization coverage scale-up, says accelerated efforts must continue. Available from: https://www.who.int/southeastasia/news/detail/18-07-2023-who-south-east-asia-region-lauds-countries-for-routine-immunization-coverage-scale-up--says-accelerated-efforts-must-continue, accessed on July17, 2024.
- Impact of the COVID-19 pandemic on immunization and surveillance of vaccine-preventable diseases in the WHO South-East Asia Region. WHO South-East Asia J Public Health. 2022;10:1-3.
- [Google Scholar]






