Translate this page into:
Epidemiological investigation of an outbreak of typhoid fever in Jorhat town of Assam, India
Reprint requests: Dr Lahari Saikia, Department of Microbiology, Assam Medical College & Hospital, Dibrugarh 786 002, Assam, India e-mail: lahari.saikia@yahoo.com
-
Received: ,
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Background & objectives:
Typhoid fever is a global health problem and is also endemic in India. An outbreak of fever occurred in January 2014 in Jorhat Town in Assam, India. Here we report the results of an investigation done to find out the aetiology and source of the outbreak.
Methods:
The affected areas were visited on January 23, 2014 by a team of Jorhat district Integrated Disease Surveillance Project personnel. A total of 13 blood samples from patients with fever as first symptom and six water samples were collected from the affected areas. The blood samples were cultured and isolates were identified using standard biochemical tests. Isolates were also tested for antimicrobial sensitivity. Widal test was performed on 10 of the 13 blood samples collected. Sanitary survey was carried out to find any leakage in the water supply and also the sewage system of the Jorhat town.
Results:
Blood culture yielded Salmonella enterica serovar Typhi in six (46.15%) patients whereas Widal test was positive in 10 (76.9%) of 13 patients. Water culture showed presumptive coliform count of >180/100 ml in two out of the six samples tested. Salmonella Typhi was also isolated from water culture of these two samples. Sanitary survey carried out in the affected places showed that the water supply pipes of urban water supply were in close proximity to the sewage drainage system and there were few leakages.
Interpretation & conclusions:
The outbreak occurred due to S. Typhi contaminating the water supply. Sanitation and immunization are the two most important components to be stressed to prevent such outbreaks.
Keywords
Blood culture
outbreak
typhoid fever
water culture
Widal test
Typhoid fever is a global health problem. An estimate of annual typhoid incidence rate of 493.5 cases per 100,000 person-years has been reported from India1. The highest incidence occurs in the regions where water supply serving large populations is contaminated with faeces2. Typhoid fever is endemic in India and is under regular surveillance by the Integrated Disease Surveillance Project (IDSP)34. Since 1990, the epidemics of Salmonella enterica serovar Typhi have been reported from different parts of India including Kolkata567. The results of an investigation on an outbreak of fever which was confirmed to be typhoid at Jorhat Town in Assam, India are reported here.
Material & Methods
This study was conducted by the department of Microbiology, Assam Medical College and Hospital, Dibrugarh, Assam, India in 2014. The institutional ethics committee approved the study. The outbreak occurred in January, 2014 at Jorhat urban with areas – Ward No.1 (Gojpuria, New Colony), Ward No.4 (Subash Colony, Netaji Colony, Rajamaidam Road and Kabarshtan) and Ward No.5 (Kalisthan). Seventy nine patients presented to Jorhat Medical College & Hopital and various private nursing homes at Jorhat, India with fever from a total population of 4050 in the affected areas.
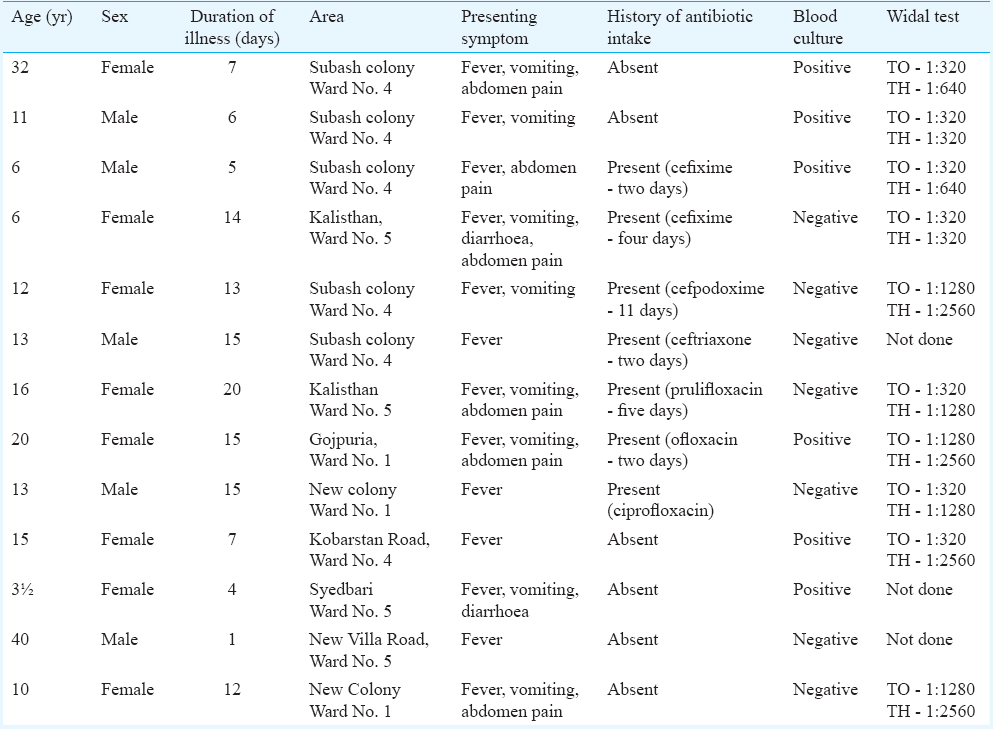
Detailed proforma for outbreak investigation was prepared. The samples were collected by visiting the affected areas on January 23, 2014 with a team of Jorhat district IDSP. The cases were followed up subsequently for a period of three weeks by Jorhat district IDSP and were found to recover without any complication. Case histories of all patients, who had fever, were recorded. Blood samples (10 ml) from 13 patients were collected in sterile containers. The blood was allowed to clot and the serum separated out. It was transferred to another sterile tube and used to perform the Widal test, both by tube and slide method ELISA for IgM antibodies against hepatitis A virus (HAV), hepatitis E virus (HEV) and Leptospira were also tested on the same samples. The clot was broken and transferred to Bile Broth and cultured for Salmonella8. Thick and thin smears were made at the bedside for detection of malarial parasites. Six water samples were collected from the affected areas. Water samples mainly stored for cooking and drinking were collected. Rectal swabs were collected from two patients with diarrhoea and transported in Cary-Blair Medium to the department of Microbiology, Assam Medical College and Hospital. Rapid screening Widal test by slide method was performed with ‘Tydal’ (Tulip Diagnostics, India) in all the outbreak cases (n=79) at Jorhat Medical College, Jorhat.
Blood cultures were carried out by both conventional and automated (VersaTREK, Thermo Fisher Scientific, USA) methods. For conventional culture, subculture was done at 24, 48 h and up to seven days (in case of negative culture) under aerobic incubation at 37°C. For VersaTREK automated system, subcultures were done when the machine indicated positive growth. Subculture was done in MacConkey agar (HiMedia, Mumbai, India) and Xylose-Lysine Deoxycholate (XLD) agar (HiMedia). Rectal swabs collected were enriched in Selenite F Broth (HiMedia) overnight and then subcultured in MacConkey agar and XLD agar. Non-lactose fermenting isolates were identified as Salmonella Typhi by standard biochemical tests9. Identification was confirmed by VITEK 2 Compact system (bioMerieux, France). Serotyping of the isolates done with specific antisera (Denka - Seiken, Japan).
The isolates were tested for antimicrobial sensitivity by Kirby–Bauer disc diffusion method as per Clinical and Laboratory Standards Institute (CLSI) guidelines10. The antibiotic discs used were ampicillin (10 µg), ciprofloxacin (5 µg), cotrimoxazole (25 µg), ceftriaxone (30 µg), chloramphenicol (30 µg) and azithromycin (15 µg). All antimicrobials were procured from HiMedia Laboratories Ltd., Mumbai, India.
Escherichia coli ATCC25922 was used for quality control. Water culture was done by multiple tube test, and the presumptive coliform count per 100 ml water was calculated from the most probable number chart11. Water samples were also plated in MacConkey agar and XLD agar and incubated at 37°C. Colonies suspected to be of S. Typhi were further processed by standard biochemical tests9.
Widal test was done by tube method (Tydal, Tulip Diagnostics, India) in 10 of the 13 blood samples collected. Three samples were haemolyzed. Widal tests with ‘O’ and ‘H’ titre of 1:160 or more were considered as positive12. Blood examination for malarial parasite (peripheral blood smear)13, ELISA for IgM HAV, HEV and Leptospira (DSIS.r.I, Saronno, Italy) were carried out as per manufacturer instructions in all the samples collected.
Sanitary survey was carried out to find any leakage in the water supply and also the sewage system of the Jorhat town.
Results
Among the 79 patients, 43 (54.4%) were males with a male:female ratio of 1.2:1. Sixty two (78.5%) were children and young adults (<20 yr of age). Fever was present in all cases followed by pain abdomen in 36 (46%), vomiting in 30 (38%) and diarrhoea in 10 (12.65%) patients. Characteristics of the cases (n=13) investigated are shown in the Table. The onset of cases from January 9 to February 6, 2014 is shown in the Figure. Maximum numbers of patients were reported on January 20 (n=14) and 17 (n=10).
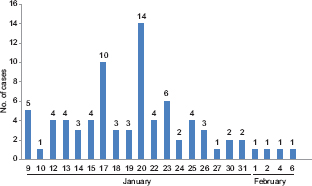
- Onset of cases (n=79) during the outbreak (January 9- February 6, 2014).
Blood culture done by conventional and automated methods in 13 patients showed positivity in six (46.15%). All culture-positive isolates were identified as S. Typhi. Rectal swabs for culture also yielded S. Typhi.
Widal test by slide method done in all the patients (n=79) was found to be 100 per cent positive, whereas the Widal test by tube method done in 10 patients also showed 100 per cent positivity.
Antibiotic susceptibility testing revealed that all isolates were susceptible to all the antibiotics tested. Serological tests for malarial parasite and HAV and HEV performed were negative in all cases. Water culture showed presumptive coliform count of >180/100 ml in two of the six samples. S. Typhi was also isolated from water culture of these two samples.
Sanitary survey carried out in the affected places showed that the water supply pipes of urban water supply were in close proximity to the sewage drainage system and there were leakages.
Discussion
The attack rate of the disease in this outbreak was 19.5 cases per 1000 population. During outbreaks of typhoid, paediatric population usually bears the burden of disease14. In the present study, 78.5 per cent patients were children and young adults. In another study, children aged 5 to 17 yr were found to be mostly affected15. The symptoms of typhoid are diverse with fever being the most common symptom. In this study all patients had fever as also reported earlier16.
Blood culture though a less sensitive method than bone marrow culture, is considered the first test of choice for both diagnosis and epidemiologic evaluation of typhoid fever17. In our study, blood culture was found to be positive in six of 13 cases and the stool culture in two cases for S. enterica serovar Typhi. Widal test by tube method was positive in all 10 patients tested. The Widal test by slide method (screening test) was positive in all patients tested.
Less blood culture positivity as compared to Widal test may be due to prior intake of antibiotics. Four patients who were blood culture negative but Widal test positive had a history of prior intake of antibiotics. Banerjee et al18 found blood culture to be positive in 63.16 per cent cases. In another study, the rate of positivity of blood culture was found to be 5.4 per cent15. According to the WHO classification of typhoid fever2, in the present outbreak, the confirmed cases of typhoid were 46.16 per cent (n=6) whereas probable cases were 38.46 per cent (n=5).
As ciprofloxacin is the first-line drug of choice for typhoid fever in most developing countries, there has been an upsurge in the occurrence of Salmonella strains resistant to ciprofloxacin. Azithromycin treatment has been shown to be useful for the management of uncomplicated typhoid fever19. Although multidrug-resistant strains of S. Typhi have been reported in India162021, we found none of the isolates to be exhibiting any resistance against the six antibiotics (ampicillin, ceftriaxone, ciprofloxacin, co-trimoxazole, azithromycin and chloramphenicol) tested. The cases were followed up regularly, and they recovered without any complication.
The outbreak occurred due to contaminated water supply with S. Typhi. Poor water quality and faecal contamination of drinking water resulting in outbreaks of typhoid fever have been reported previously15161821. The water supply for this outbreak was the urban water supply provided by the municipality. The presumptive coliform count in two of the six water samples tested was found to be very high. S. Typhi was also isolated from water culture of these two samples.
Health camps were regularly held in the affected areas and patients treated with ciprofloxacin. As the source of the outbreak could be traced and appropriate measures taken, the outbreak could be rapidly curtailed.
Acknowledgment
The authors acknowledge Dr A. K. Adhikari, Principal-cum-Chief Superintendent, Assam Medical College and Hospital, Dibrugarh, Assam, for allowing the study to be done at the Department of Microbiology, Assam Medical College and Hospital, Dibrugarh, Assam and Dr Tarun C. Das, District Surveillance Officer, Integrated Disease Surveillance Project, Jorhat district, for the assistance during data collection. The authors thank Shri Bibhas Sarma, Epidemiologist, Jorhat district, Dr Saurav Jyoti Patgiri, Smt Sunjan Gogoi and Shri Charitra Saikia, for technical assistance.
Conflicts of Interest: None.
References
- A study of typhoid fever in five Asian countries: disease burden and implications for controls. Bull World Health Organ. 2008;86:260-8.
- [Google Scholar]
- World Health Organization. Background document: The diagnosis, treatment and prevention of typhoid fever. Communicable disease surveillance & response. In: Department of Vaccines and Biologicals. Geneva: WHO; 2003. p. :4-13.
- [Google Scholar]
- Park K, ed. Epidemiology of communicable diseases. Park's textbook of preventive medicine (18th ed). Jabalpur: Ms Banarasidas Bhanot; 2005. p. :121-284.
- National Centre for Disease Control. Integrated disease surveillance Project (IDSP). Project implementation plan. Ministry of Health & Family Welfare, New Delhi. Government of India. Available from: http://www.ncdc.gov.in/writereaddata/linkimages/222.pdf
- A note on incidence of typhoid fever in diverse age groups in Kolkata, India. Jpn J Infect Dis. 2003;56:121-2.
- [Google Scholar]
- Comparison of whole blood culture and blood clot culture for the diagnosis of enteric fever. JKIMSU. 2013;2:145-6.
- [Google Scholar]
- Tests for the identification of bacteria. In: Collee JG, Fraser AG, Marmion BP, Simmons A, eds. Mackie & McCartney practical medical microbiology (14th ed). London: Churchill Livingstone; 1996. p. :131-49.
- [Google Scholar]
- Clinical and Laboratory Standards Institute. Performance standards for antimicrobial susceptibility testing; twenty third informational supplement, CLSI document M100-S23. Wayne, PA: CLSI; 2013.
- Examination of water, milk, food and air. In: Collee JG, Fraser AG, Marmion BP, Simmons A, eds. Mackie & McCartney practical medical microbiology (14th ed). London: Churchill Livingstone; 1996. p. :883-921.
- [Google Scholar]
- Value of single Widal test in the diagnosis of typhoid fever. Indian Pediatr. 1994;31:1373-7.
- [Google Scholar]
- Examination of blood for parasites. In: Parasitology protozoology & helminthology (13th ed). India: CBS Publishers & Distributors; 2009. p. :266-70.
- [Google Scholar]
- Use of vaccines for the prevention of typhoid fever. Indian Pediatr. 2003;40:1029-34.
- [Google Scholar]
- Epidemiological investigation of a typhoid outbreak. Med J Armed Forces India. 2008;64:241-2.
- [Google Scholar]
- Outbreak of multi-drug resistant Salmonella Typhi enteric fever in Mumbai Garrison. Med J Armed Forces India. 2005;61:148-50.
- [Google Scholar]
- Epidemiological investigation of an outbreak of enteric fever. Med J Armed Forces India. 2007;63:322-4.
- [Google Scholar]
- Antimicrobial resistance in typhoidal salmonellae. Indian J Med Microbiol. 2011;29:223-9.
- [Google Scholar]
- An outbreak of multidrug resistant typhoid fever in Bangalore. Indian J Pediatr. 1995;62:445-8.
- [Google Scholar]
- Occurrence of multi-drug resistant Salmonella Typhi in Calcutta. Indian J Med Res. 1992;95:179-80.
- [Google Scholar]






