Translate this page into:
Elephantiasis nostras verrucosa
*For correspondence: sulepot@mynet.com
-
Received: ,
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
A 41 yr old man was admitted to the Internal Medicine department of the Haseki Training and Research Hospital, Istanbul, Turkey, in January 2016. He complained of pain, bad smell, deformity and bilateral swelling on the lower limbs. He gave history of having these complaints for the last 15 years. Occasionally, he received antibiotic therapy and had no family history of familial lymphoedema. His medical history included type 2 diabetes mellitus with nephropathy, morbid obesity, hypertension and congestive heart failure. On physical examination, his lower extremities showed pitting oedema; lichenification; indurated, cobblestone-like papulonodules and plaques (Fig. 1). The systemic examination of the patient was normal (WBC count 14.5×109/l, neutrophils; 11.8×109/l, haemoglobin; 10.9 mg/dl, platelet; 289.0×109/l, C-reactive protein; 14.03 mg/dl and sedimentation; 117 mm/h). Liver and kidney function tests were normal. Empiric antibiotic, ciprofloxacin and metronidazole were started before culture results. Proteus vulgaris grew in the culture of the foot. According to antibiogram results, ciprofloxacin treatment was continued. Intravenous furosemide and heparin was started to control oedema and deep vein thrombosis. In addition, he was encouraged to increase ambulation, elevate his legs and reduce his body weight. Lymphoscintigraphy of the lower limbs was performed using subcutaneous injection of 99mTc-nanocolloid into the first interdigital space in each foot. Uptake was not seen in lymphatic pathways, pelvic and popliteal lymph nodes. There was complete occlusion of lymphatic channels (Fig. 2). After exclusion of osteomyelitis, the patient was sent to the departments of dermatology and plastic surgery. The surgery was done for resection of the hypertrophied areas. The patient was lost to follow up after surgery.

- A: Pitting oedema; B: lichenification; C: indurated, cobblestone-like papulonodules; and plaques.
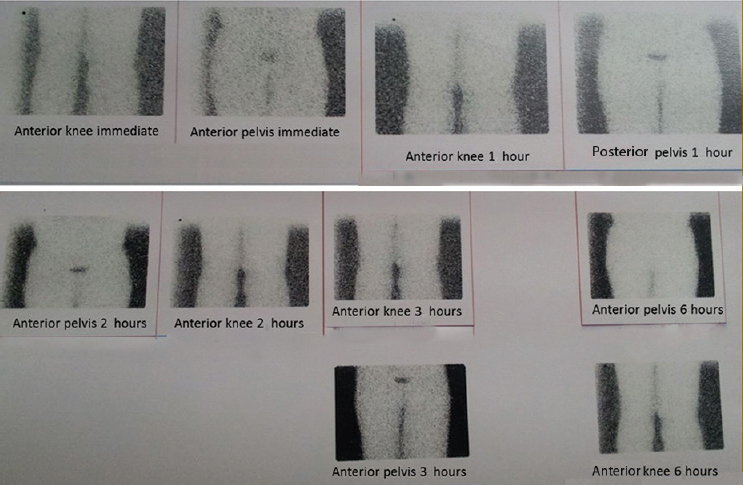
- Lymphoscintigraphy of the lower limbs. Uptake was not seen in lymphatic pathways, pelvic and popliteal lymph nodes. There is complete occlusion of lymphatic channels.
Acknowledgment
We would like to thank the dermatologist Dr Leyli Kadriye Koç, microbiologist Dr Burcu Bayrak and plastic surgeon Dr Sevgi Kurt Yazar.





