Translate this page into:
Effect of hypertension at presentation on prognosis in patients with dilated cardiomyopathy presenting with normal renal angiogram
Reprint requests: Dr Goru Bhawani, Department of Pharmacology, Narayana Medical College, Nellore 524 003, Andhra Pradesh, India e-mail: bhawanigk22@yahoo.co.in
-
Received: ,
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Background & objectives:
Dilated cardiomyopathy (DCM) is a progressive disease of heart with systolic and diastolic dysfunction carrying a poor long-term prognosis. The prognostic index and predictors of mortality are considered to be useful in guiding the treatment. This study was undertaken to evaluate the effects of hypertension at presentation on prognosis in patients with DCM presenting with normal renal and coronary angiogram.
Methods:
An observational, analytical, non-interventional and a combination of retrospective and prospective study was conducted in patients between 15 and 75 yr of age with DCM having on and off symptoms while receiving treatment in a cardiology outpatient department for more than a year. Sixty patients who fulfilled the inclusion criteria were enrolled in the study. Left ventricular systolic and diastolic functions were assessed by echocardiography along with New York Heart Association (NYHA) functional class prospectively and at baseline retrospectively. Patients were grouped into two categories: DCM with hypertension at presentation (HTNAP, Category 1) and DCM without hypertension at presentation (NHTNAP, Category 2). The primary end-points were the number and dose of parenteral drugs at hospitalization, duration of hospital stay and change in the left ventricular (LV) systolic function expressed as LV ejection fraction, and the secondary end-points included overall mortality, change in LV and right ventricular systolic and diastolic functions and change in the NYHA functional class between baseline and three month follow up in patients.
Results:
Thirty five and 25 patients presented with HTNAP and NHTNAP, respectively (total 60). The overall mortality was 10 per cent (6/60). The number of hospitalizations was less in HTNAP category and of days of hospital stay was 6.3 in HTNAP and 9.8 in NHTNAP, the difference being significant (P < 0.001). The HTNAP category required less parenteral diuretics and inotropes compared with the NHTNAP category. The echocardiographic parameters showed better improvements in the HTNAP group as compared to the NHTNAP group. Overall, the patients in the <35 yr of age showed the best prognosis (P < 0.001).
Interpretation & conclusions:
Normal or high blood pressure response at acute presentation of DCM leads to better prognosis which may be due to an intact renovascular and an active sympathetic system and can depict the stage of DCM.
Keywords
Active sympathetic system
dilated cardiomyopathy
hypertension
prognostic factors
Dilated cardiomyopathy (DCM) is a progressive disease of heart muscle that is characterized by ventricular chamber enlargement and systolic dysfunction with normal left ventricular (LV) wall thickness1. DCM is the third most common cause of heart failure, with a prevalence of 36.5 per 100,000 in a population-based study2. Historically, the prognosis of patients with DCM has been very poor, with a median survival of two years after diagnosis3; although there have been advances in the medical and surgical therapy of DCM in the last two decades, the condition still carries a poor long-term prognosis. Right ventricular (RV) dysfunction may be present in DCM and is an important adverse prognostic marker, associated with significantly worse functional class and outcome4.
Although ischaemic cardiomyopathy and other forms of DCM can cause the symptoms of heart failure, each type requires a specific treatment strategy, surgical intervention and lifestyle choices to effectively control the disease. In patients with suspected heart failure or LV dysfunction, echocardiography is the most important investigation in establishing the diagnosis of DCM, by defining the presence and severity of LV dilatation and dysfunction. Using conventional echocardiography and Doppler ultrasound as also the recent technologies such as tissue-Doppler imaging, strain analysis and real-time three-dimensional echocardiography, it is possible to provide important pathophysiological information that can be used to guide the optimal clinical management of patients with DCM5.
The prognosis of DCM presenting with fluctuations of blood pressure is not known, particularly in the absence of coronary disease and diabetes6. Very little data are available regarding the characteristics and prognosis of symptomatic patients with idiopathic DCM presenting with varied clinical conditions. Invasive and non-invasive parameters of diastolic function reveal comparable information for the estimation of prognosis of patients with DCM to initiate early therapy. A relatively large percentage of patients with an idiopathic DCM will have a marked improvement in the LV systolic function. This is more likely to happen in the presence of a short duration of symptoms and better LV functions7. The prognostic index is therefore, useful for evaluating patients and guiding treatment. This study was aimed at investigating the outcome and the predictors of mortality in DCM patients with LV systolic dysfunction presenting with or without hypertension at acute decompensated state.
Material & Methods
The study was conducted in the department of Cardiology, GSL Medical College and Hospital, Rajahmundry India, over a period of four months (April-July, 2013) after taking prior approval from the Institutional Ethics Committee. The study was observational, analytical, non-interventional, and a combination of both retrospective and prospective observations. Patients between 15 and 75 yr of age with DCM and with on and off symptoms while receiving treatment attending GSL Cardiology outpatient department for more than a year were evaluated. Sixty patients who fulfilled the inclusion criteria were enrolled. Diagnosis was based on guidelines for DCM [ejection fraction (EF) <30% with left ventricular internal diameter in diastole (LVIDD) >5.3 cm in females and >5.8 cm in males]8 and heart failure. LV systolic and RV diastolic functions in the patients were assessed by echocardiography along with the New York Heart Association (NYHA) functional class8 prospectively and at baseline retrospectively.
Inclusion criteria: Heart failure with DCM presenting in NYHA IV with pulmonary oedema and orthopnoea, raised pulmonary artery pressure (PAP) defined echocardiographically [pulmonary artery systolic pressure >35 mmHg by tricuspid regurgitation (TR) gradient method], hypertension (defined as systolic pressure >140 mmHg and diastolic >90 mmHg), normotensive or hypotensive (systolic pressure <90 mmHg and diastolic <60 mmHg) at presentation and non-significant renal and coronary angiogram.
Exclusion criteria: Patients with primarily valvular heart disease with DCM, acute coronary syndrome, congenital heart disease, any rhythm abnormality, history of any malignancy, secondary hypertension and electrocardiogram showing previous myocardial infarction were excluded from the study.
Parameters in relation to DCM with heart failure involving LV systolic dysfunction are LV end diameter in diastole (LVEDD), LV end diameter in systole (LVEDS) and LV ejection fraction (LVEF). LV diastolic parameters included E/A ratio, pulmonary capillary wedge pressure (PCWP), TR gradient, RV systolic pressure, left atrial diameter (LA) and mean PAP through echocardiography. Moderate concentric hypertrophy with wall motion abnormalities was also noted. Cystent Philips HD 11XE with Ultrasound system with colour Doppler and S4-2 sector array probe (Trisonics. Inc, Netherlands) was used for recording the echocardiographic parameters. Intraobserver variability was <15 per cent.
Study design: Enrolled patients were grouped into two categories: category 1: DCM with hypertension at presentation (HTNAP) or high normal range of blood pressure; and category 2: DCM with hypotension at presentation (NHTNAP).
Each group was further divided, according to the age, into minimum three groups to avoid as much bias as possible. The two study groups maintained similar baseline characteristics. The primary end-points of the study were the number and dose of parenteral drugs used or required during episodes of exacerbation, duration of hospital stay, change in the LV systolic function expressed as LVEF between baseline and at the end of study period in patients of both the categories. The secondary end-points included overall mortality, change in LV and RV systolic and diastolic functions and change in the NYHA functional class between baseline and three month follow up in patients of all groups. The other prognostic factors such as pulmonary hypertension (PH), raised triglyceride/high-density lipoprotein (analysed by Thyrocare Labs) ratio and body mass index were assessed for the strength of their association with prognosis.
Intravenous (i.v.) drugs included dobutamine 2-5 µg/kg/min, levosimendan 6 µg/kg loading dose for 10 min followed by 0.1 µg/kg/min for 24 h on day 2, two ampoules furosemide stat followed by i.v. furosemide drip 20-40 mg/h, i.v. morphine 3 mg six hourly. Oral drugs included metolazone 5 mg, ramipril 1.25 mg twice daily, carvedilol 3.125 mg twice daily, digoxin 0.25 mg one tablet stat followed by half tablet once daily and spironolactone 25-50 mg once daily.
Statistical analysis: Continuous variables are expressed as mean ± SD. For each parameter, the analysis of result was done by using unpaired Student's t-test or Wilcoxon rank sum test as appropriate based on the differences between the groups. Paired t test was performed for data within the groups. Categorical variables are presented as per cent values and compared by Chi-square test. Analyses were performed using SPSS version 16 (IBM, Chicago, USA).
Results
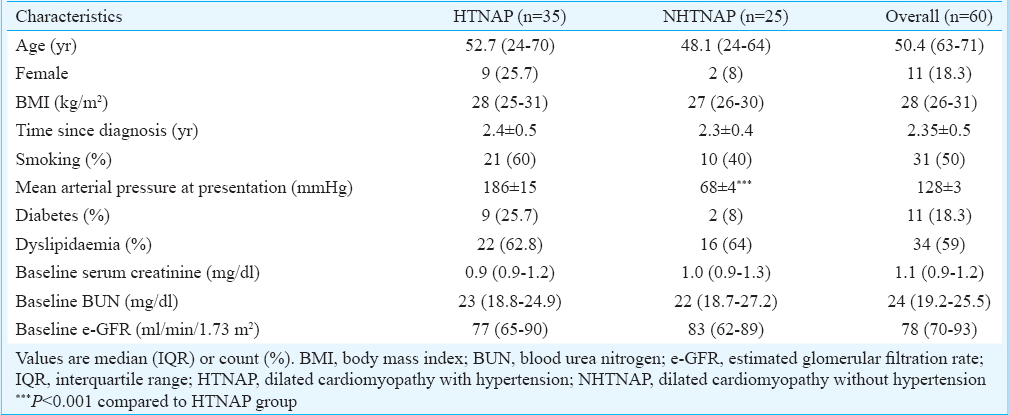
The baseline demographic and clinical characteristics of the patients enrolled in the study are shown in Table I. Almost all characteristics between the two categories (HTNAP & NHTNAP) were comparable except mean arterial pressure which was significantly lower (P<0.001) in NHTNAP category patients. Of the 60 patients enrolled, 35 patients presented with HTNAP and 25 patients presented with NHTNAP. All patients were kept on standard treatment of diuretics, inotropes, angiotensin-converting enzyme (ACE) inhibitors and beta-blockers.
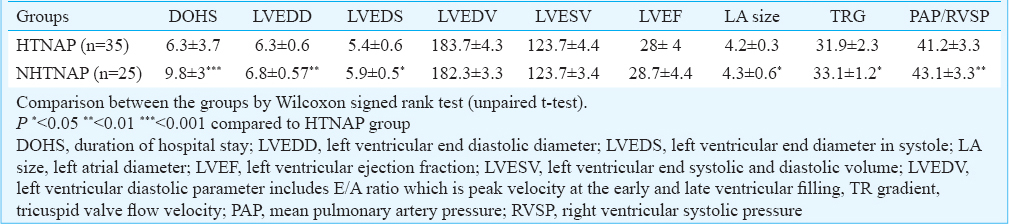
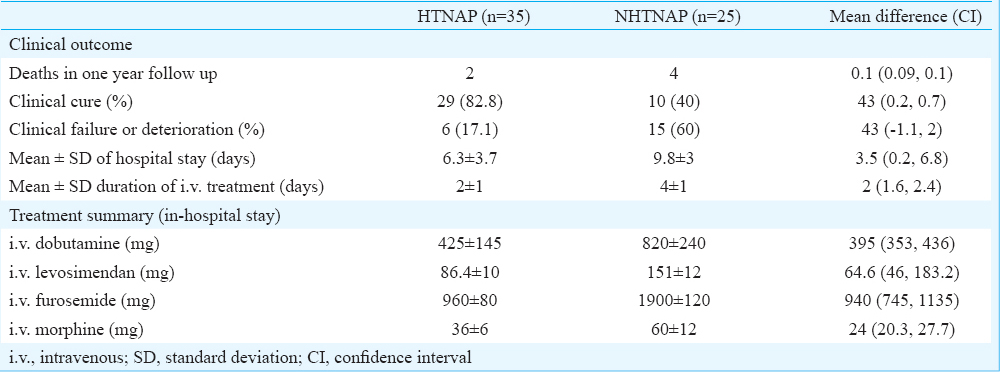
Short-term prognosis: The overall in-hospital mortality was 10 per cent (6/60) with four patients succumbing to death in NHTNAP and two patients in HTNAP group. The duration of hospital stay in the HTNAP category was 6.3 days whereas in NHTNAP was 9.8 days P < 0.001 (Table II). The clinical cure (defined as the absence of symptoms with which they presented at the time of hospitalization) was 84.8 per cent in HTNAP as compared to 40 per cent in NHTNAP group. Moreover, patients in the HTNAP category required less parenteral drugs with mean values of (425 mg of dobutamine, 86.4 mg of levosimendan 960 mg of furosemide and 36 mg of morphine) when compared with the NHTNAP (Table III).
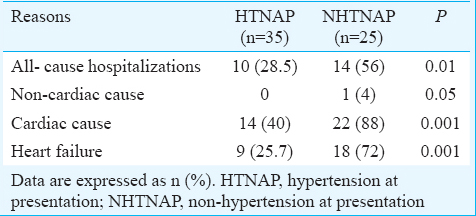
Long-term prognosis: Most of the patients were on follow up for a period of 24 months including the three month study period, and long-term prognosis was estimated by the change in the echocardiographic parameters and the number of hospitalizations during this period. Within the category HTNAP, the patients on the 15-50 yr age group showed the best prognosis (P < 0.001, 0.01) when compared to other age group. All the echocardiographic parameters showed improvements in both the age groups (Table IV). The percentages of all-cause, non-cardiac, cardiac and heart failure hospitalization were 28.5, 0, 40 and 25.7 per cent, respectively, and 70 per cent of them were with age >35 yr (Table V). There was a prompt shift from NYHA functional class IV to II as indicated by the less in-hospital stay as compared to the NHTNAP group.
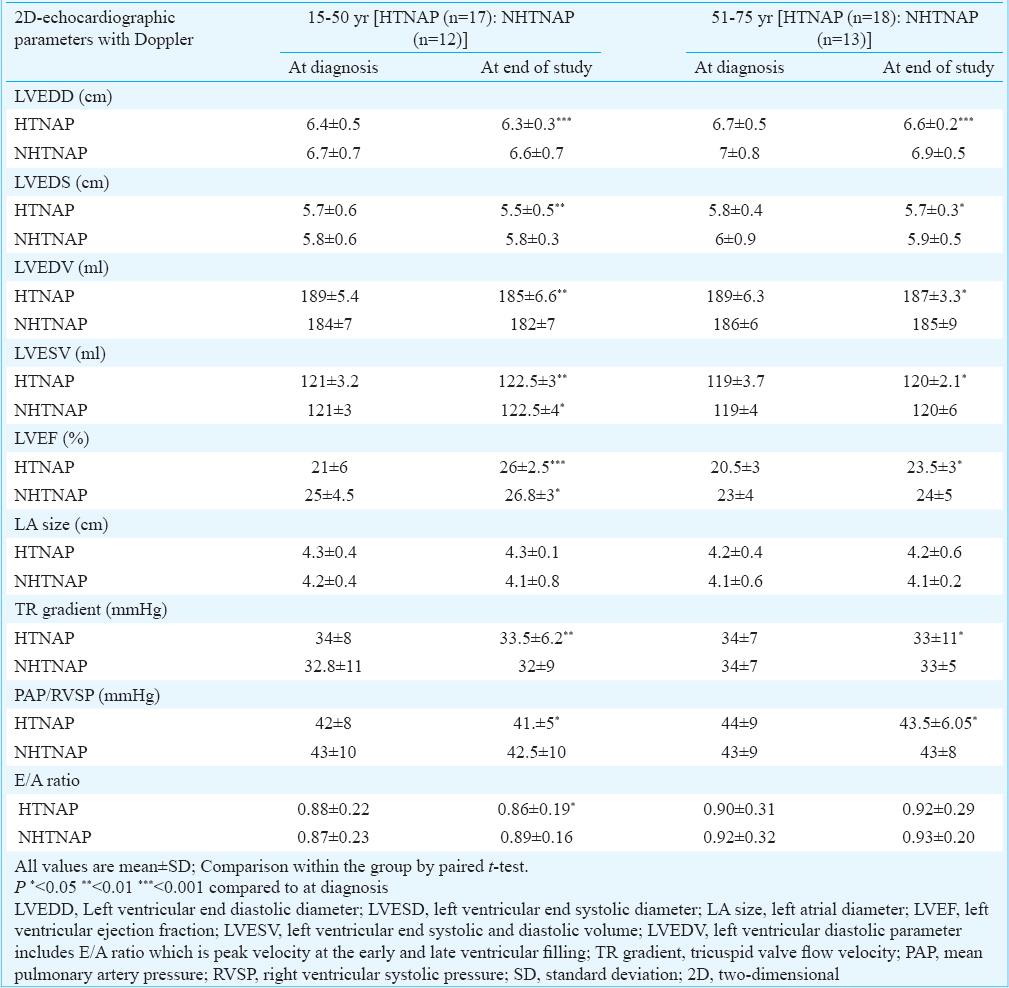
The NHTNAP category patients in the 15-50 yr age group showed some improvement in the echocardiographic parameters when compared to the other age group (Table IV). The percentage of all-cause, non-cardiac, cardiac and heart failure hospitalisation was 56, 4, 88 and 72 per cent, respectively (Table V).
Between the categories (HTNAP & NHTNAP): Most of the echocardiographic parameters showed better improvements in the HTNAP group as compared to the NHTNAP group (Table II). There were significantly (P<0.01) less hospitalizations due to various causes in the HTNAP group (Table V).
Discussion
This study showed that patients with DCM with either HTNAP or towards the high normal blood pressure at presentation had shorter duration of hospitalization and required less diuretics and inotropes than those presenting with NHTNAP. The overall mortality over the course of two years follow up was more in the NHTNAP category than in the HTNAP. There was improvement in all the echocardiographic parameters in the HTNAP when compared with the NHTNAP. A growing body of experimental and clinical evidence suggests that the portfolio of compensatory mechanisms, which include the activation of biologically active molecules, sympathetic nervous system and renin-angiotensin system, is responsible for maintaining the cardiac output and cardiac repair and remodelling9. The disturbances in the autonomic control were initially attributed to loss of the inhibitory input from arterial or cardiopulmonary baroreceptor reflexes, but there is increasing evidence that excitatory reflexes may also participate in the imbalance10. In heart failure, inhibitory input from baroreceptors and mechanoreceptors decreases and excitatory input increases, with the net result of generalized increase in sympathetic nerve traffic and blunted parasympathetic nerve traffic with a resultant loss of heart rate variability and increased peripheral vascular resistance. The AdreView Myocardial Imaging for Risk Evaluation in Heart Failure (ADMIRE-HF) study examined the prognostic usefulness of myocardial sympathetic innervation11. The results showed that temporarily heightened activity of sympathetic system elicited modest positive inotropic effect and maintained vascular resistance for organ perfusion. Apart from this, the renin-angiotensin system is critical for maintaining short-term circulatory homeostasis. In a detailed analysis of systolic blood pressure in patients from the OPTIMIZE-HF study12, there was a relatively monotonic relationship between blood pressure and mortality, with no evidence of increased risk even at very high levels of systolic blood pressure (>180 mmHg). Interestingly, the LVEF had a little bearing on the conduct of the in-hospital stay of patients with respect to the duration, number and dose of drugs being used.
Normally, the pulmonary vasculature is characterized by low pressure, low resistance and high distensibility. When this compensatory capacity is exceeded, PAP rises at first on exertion and then at rest. The right ventricle is sensitive to changes in afterload. Excessive stimulation of sympathetic and renin-angiotensin system, as well as accumulation of endothelin, contributes to the compensatory capacity131415. In patients with heart failure, PH is a predictor of poor outcome. The E-wave deceleration rate, E/A ratio and degree of mitral regurgitation are the strongest predictors. Pulmonary arterial pressure correlates with the LV end diastolic pressure and diastolic dysfunction1617, and it is associated with increased short- and long-term mortality in patients with both reduced and preserved LVEF. Patients with a higher velocity of tricuspid regurgitation (>2.5 m/s) had a 40 per cent higher mortality rate and a 50 per cent higher rate of HF admissions than those with normal pulmonary pressures and also impacts the exercise capacity in HF patients1819.
In conclusion, an intact renovascular and an active sympathetic system, which leads to a hypertensive or normotensive response of patients at the time of hospitalization due to acute heart failure with pulmonary oedema and LV systolic dysfunction is a marker of intact autoregulation of vital organs during acute conditions; hence, treatment with ACE inhibitors and beta-blockers gives better response and prognosis in this group of patients than in those presenting with hypotension having an exhausted renovascular and sympathetic system. Our results suggested that irrespective of blood pressure variation at presentation, the clinical and demographic features were the same but prognosis was better if the blood pressure was normal or high.
Acknowledgment
Authors acknowledge the Indian Council of Medical Research for financial support under STS Programme 2012.
Conflicts of Interest: None.
References
- Dilated cardiomyopathies of the adult (first of two parts) N Engl J Med. 1982;307:1051-8.
- [Google Scholar]
- Clinical utility gene card for: dilated cardiomyopathy (CMD) Eur J Hum Genet 2013:21.
- [Google Scholar]
- Clinical and pathologic study of familial dilated cardiomyopathy. Am J Cardiol. 1990;65:1449-53.
- [Google Scholar]
- Discordance in degree of right and left ventricular dilatation in patients with dilated cardiomyopathy: Recognition and clinical implications. J Am Coll Cardiol. 1993;21:649-54.
- [Google Scholar]
- The role of echocardiography in guiding management in dilated cardiomyopathy. Eur J Echocardiogr. 2009;10:iii15-21.
- [Google Scholar]
- Behaviour of blood pressure in dilated cardiomyopathy patients suspected significantly hypertensive at echocardiography. Acta Cardiol. 1995;50:203-7.
- [Google Scholar]
- The etiology, course and prognosis of dilated cardiomyopathy. Z Kardiol. 1982;71:497-508.
- [Google Scholar]
- American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. 2013 ACCF/AHA Guideline for the Management of Heart Failure. A Report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. Circulation. 2013;128:1495-1502.
- [Google Scholar]
- Novel mechanisms of sympathetic regulation in chronic heart failure. Hypertension. 2006;48:1005-11.
- [Google Scholar]
- Sympathetic activation in human heart failure: Diverse mechanisms, therapeutic opportunities. Acta Physiol Scand. 2003;177:391-8.
- [Google Scholar]
- Myocardial iodine-123 meta-iodobenzylguanidine imaging and cardiac events in heart failure. Results of the prospective ADMIRE-HF (AdreView Myocardial Imaging for Risk Evaluation in Heart Failure) study. J Am Coll Cardiol. 2010;55:2212-21.
- [Google Scholar]
- Systolic blood pressure at admission, clinical characteristics, and outcomes in patients hospitalized with acute heart failure. JAMA. 2006;296:2217-26.
- [Google Scholar]
- Neurohormonal activation and the chronic heart failure syndrome in adults with congenital heart disease. Circulation. 2002;106:92-9.
- [Google Scholar]
- Alterations in cardiac beta-adrenoceptor responsiveness and adenylate cyclase system by congestive heart failure in dogs. Eur J Pharmacol. 1987;140:123-32.
- [Google Scholar]
- Angiotensin II receptor blockade and effects on pulmonary hemodynamics and hypoxic pulmonary vasoconstriction in humans. Chest. 1996;110:698-703.
- [Google Scholar]
- Determinants of pulmonary hypertension in left ventricular dysfunction. J Am Coll Cardiol. 1997;29:153-9.
- [Google Scholar]
- Doppler-derived mitral and pulmonary venous flow variables are predictors of pulmonary hypertension in dilated cardiomyopathy. Echocardiography. 2002;19:457-65.
- [Google Scholar]
- Pulmonary hypertension predicts mortality and morbidity in patients with dilated cardiomyopathy. Ann Intern Med. 1992;116:888-95.
- [Google Scholar]
- Pulmonary hypertension and risk of death in cardiomyopathy: Patients with myocarditis are at higher risk. Circulation. 2002;105:1663-8.
- [Google Scholar]






