Translate this page into:
Effect of a deacyl gymnemic acid on glucose homeostasis & metabolic parameters in a rat model of metabolic syndrome
Reprint requests: Dr Samir Malhotra, Additional Professor, Department of Pharmacology, Postgraduate Institute of Medical Education & Research, Chandigarh 160 012, India e-mail: samirmalhotra345@yahoo.com
-
Received: ,
This is an open-access article distributed under the terms of the Creative Commons Attribution-Noncommercial-Share Alike 3.0 Unported, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Background & objectives:
Metabolic syndrome (MS) comprises several cardio-metabolic risk factors, which include obesity, hypertension, hyperglycaemia, hypertriglyceridaemia and decreased HDL cholesterol. Leaf extract of Gymnema sylvestre has been shown to possess glucose lowering activity in animal models. This study was carried out to evaluate the efficacy of deacyl gymnemic acid (DAGA), active constituent of G. sylvestre, in a rat model of MS.
Methods:
Six groups consisting of six wistar rats in each, were studied. Group I received the normal diet, while the remaining five groups received high fructose diet (HFD) for 20 days to induce MS. HFD was continued in these five groups for the next 20 days along with group II received vehicle solution, group III received pioglitazone and groups IV- VI received DAGA in variable doses. Systolic blood pressure (SBP) was measured using tail-cuff method. Oral glucose tolerance test (OGTT) was done at baseline and at days 20 and 40. Blood samples were collected for glucose, insulin and lipid profile.
Results:
Administration of HFD for 20 days resulted in weight gain (>10%), increase in SBP, fasting plasma glucose (FPG) and triglycerides fulfilling the criteria for MS. Administration of DAGA (200 mg/kg) reduced SBP and significantly improved the FPG and HOMA-IR (homeostatis model assessment-insulin resistance) with modest improvement in lipid profile without decrease in body weight similar to pioglitazone.
Interpretation & conclusions:
Our findings show that DAGA decreases SBP and improves parameters of glucose-insulin homeostasis in a rat model of MS induced by HFD. Further studies are required to elucidate the mechanism of action.
Keywords
Deacyl gymnemic acid
Gymnema sylvestre
metabolic syndrome
Metabolic syndrome (MS) is a cluster of several cardio-metabolic risk factors, which include abdominal obesity, hypertension, hyperglycaemia and increased triglycerides and decreased HDL cholesterol. All these parameters are surrogate markers of insulin resistance and predict the risk for future development of diabetes and cardiovascular diseases1.
The prevalence of metabolic syndrome is on the rise in both developing as well as in developed countries. Data from the third National Health and Nutrition Examination Survey (NHANES III), show that approximately one fourth of the US adults 20 years or older have metabolic syndrome2. Worldwide, in adult population samples, the prevalence of MS has been shown to vary from 8 to 24 per cent3. Many studies from developing countries including India also show high prevalence of metabolic syndrome varying from 15 to 45 per cent45. Authors have previously reported two third of patients with stable coronary artery disease had metabolic syndrome6.
Lifestyle modification remains the mainstay of treatment of metabolic syndrome. Even 10 per cent decrease in body weight rewards appreciably in reduction of blood pressure, favourable lipid profile and improved glucose-insulin homeostasis. Unfortunately, till date no single pharmacological therapy has been found to address all the components of metabolic syndrome. Drugs like metformin, thiazolidinedione, ACE (angiotensin converting enzyme) inhibitors and statins are directed towards the individual components of the metabolic syndrome and do not address in totality.
Many alternative medications including herbs have been examined for their efficacy in metabolic syndrome7891011. These include plant extracts from Zingiber officinale rhizome9 and Gymnema sylvestre (Asclepiadaceae)11. G. sylvestre is a woody climber that grows in tropical forest of central and southern India78. Leaves of this herb cause a loss of sweet taste. The active ingredients of the plant obtained from leaves are a group of acids termed as gymnemic acids which have been shown to have anti-hyperglycaemic activities in some studies, while other could not show similar results10. Oral feeding of powdered leaves of G. sylvestre (500 mg per rat) for 10 days prevented intravenous beryllium nitrate induced hyperglycaemia in rats and normalized it in four days in comparison to 10 days in untreated rats. However, no significant hypoglycaemia was seen in normal rats who were daily fed with the leaves of G. sylvestre for 25 days12. Single as well as chronic (32-35 days) oral administration of aqueous extract of G. sylvestre leaves (1 g/kg) did not have any significant effect on immuno-reactive insulin levels13. Tominaga et al14 reported no effect of G. sylvestre leaves extract (120 mg/kg/day PO) administered for seven days on insulin resistance in streptozotocin (STZ) induced diabetic rats. G. sylvestre contains several ingredients15, of which most active constituent is deacyl gymnemic acid (DAGA), which has not been examined earlier. The present study was undertaken to evaluate the efficacy of DAGA on various components of metabolic syndrome in a rat model induced by high fructose diet.
Material & Methods
Animals: This study was conducted in the department of Pharmacology, Postgaduate Institute of Medical Education & Research (PGIMER), Chandigarh, India, from January 2008 to June 2009. Approval from the Institute′s animal ethics committee was taken prior to conducting the study. Wistar rats of both sexes weighing between 150-180 g were procured from the central animal house of PGIMER, Chandigarh. They were kept individually in polypropylene cages in an environmentally controlled room of the departmental animal house, and maintained at 25±2° C with a 12-h dark/light cycle and 40-70 per cent humidity. The animals had free access to food and water. Rats were fed with standard rat chow diet or special high fructose diet (HFD) according to the protocol. Experiments were carried out after a week of acclimatization.
Drugs and chemicals: Deacyl gymnemic acid which is 90 per cent pure (batch no. RD/1574) and pioglitazone were gifted by Natural Remedies, Bangalore, India, and Ind-Swift Pharmaceuticals, Chandigarh, India, respectively.
Experimental groups: Six groups consisting of six wistar rats in each, were studied. Group I, as control received normal diet, while the remaining five groups were fed with high fructose diet (HFD) [supplied by Central Drug House (P) Ltd., New Delhi, India] for 20 days ad libitum. The HFD provided 60 per cent of the calories from fructose. Group II continued to receive HFD and vehicle solution, while group III received HFD and pioglitazone 2.7 mg/kg body weight orally for the next 20 days. The remaining three groups (IV to VI) continued to receive HFD and DAGA at a dose of 50, 100 and 200 mg/kg orally for the next 20 days. Since this compound had never been tested before, dose selection was done on the basis of some preliminary work done in our department. All the drugs were administered once daily by gavage in 1 per cent carboxy-methyl cellulose (CMC) suspension.
Blood pressure was measured by tail-cuff method16 at baseline, days 20 and 40 [Ugobasile, Biological research apparatus, comerio-(va)-Italy]. After light ether anaesthesia, the tail of rat was cleaned with xylene. An occluding cuff similar in principle to that used for routine blood pressure measurements in humans was placed over the tail (near the base), with a piezoelectric transducer placed about 0.5-1 cm distal to the cuff. Pressure in the cuff is increased until the tail pulse disappears and then is released slowly. The systolic BP was taken as the average of the values when the tracing disappears on inflation and reappears on deflation.
The oral glucose tolerance test (OGTT) was performed at baseline, at days 20 and at 40 with the administration of equivalent anhydrous glucose at a dose of 200 mg/kg. Samples for plasma glucose and insulin were collected from the tail vein of rats after an overnight fast at ‘0 min’ and samples were estimated for plasma glucose at 15, 30, 60 and 120 min. The blood samples for lipids were collected at baseline, and at days 20 and 40. Lipid profile estimation was carried out in the pooled plasma in each group. The criteria for metabolic syndrome was defined as 10 per cent increase in body weight and serum triglycerides more than 130 mg/dl after HFD17.
The plasma glucose was estimated by glucose oxidase method18 from commercial kits purchased from CDR Diagnostics, Hyderabad, India. Plasma samples for insulin estimation were stored at -20°C and measured by rat insulin ELISA kit purchased from Mercodia AB, Seminariegatan, Uppsala, Sweden. Plasma total cholesterol and triglycerides were measured enzymatically (Randox Laboratories Ltd., UK) on a digital colorimeter (Digichem Economy, UK). HDL cholesterol was measured (AUTOPAK, Bayer Diagnostics India Ltd., India) on digital colorimeter after precipitation of chylomicrons and LDL cholesterol were measured by Friedwald equation19. Insulin resistance (IR) was calculated using homeostasis model assessment (HOMA-IR) and beta cell function (HOMA-β) assessment was done according to formula derived by Mathews et al20.
Statistical analysis: Intra-group comparisons were done by repeated measures ANOVA. Inter-group comparisons were made using one-way ANOVA followed by post-hoc Bonferroni's test. For the calculation of area under curve (A UC) 0 of OGTT, 0 glucose values at 0, 15, 30, 60 and 120 min were calculated according to trapezoidal rule. Increase in AUC of glucose suggests occurrence of insulin resistance.
Results
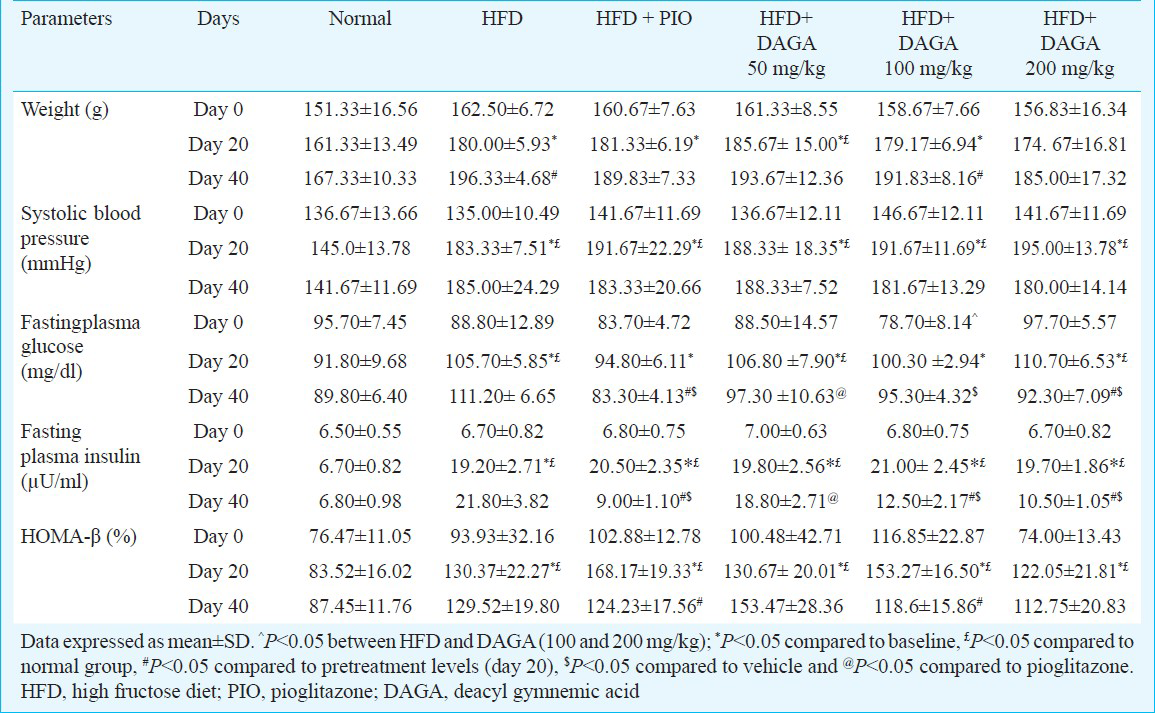
The baseline weight of rats in different groups was not significantly different. Administration of HFD for a period of initial 20 days resulted in an increase in body weight of more than 10 per cent (range 10-15%) in all the groups and reached to significance in all the groups except in group VI (Table). While rats fed on normal diet (control group) gained 6 per cent increase in body weight which was insignificant as compared to HFD administered groups. After intervention with pioglitazone and different doses of DAGA day 20 onwards had no significant change in body weight except DAGA at a dose of 100 mg/kg which was significant. The baseline systolic blood pressure (SBP) in all the groups was similar and administration of HFD for a period of 20 days resulted in about 33 per cent increase SBP in all the groups. Pioglitazone and different doses of DAGA reduced the SBP but could not achieve statistical significance. The baseline fasting plasma glucose (FPG) was similar in all the groups except in group V and administration of HFD for a period of 20 days resulted in significant increase in FPG of about 13-27 per cent in all the groups. Administration of pioglitazone 2.7 mg/kg and DAGA 200 mg/kg caused a significant decrease in FPG level at day 40, however, there was no difference between both the groups. The doses of 50 and 100 mg/kg of DAGA did not influence the FPG profile at day 40. The baseline fasting plasma insulin (FPI) was similar in all the groups and administration of HFD for 20 days significantly increased FPI in all groups as compared to baseline. Pioglitazone 2.7 mg/kg and DAGA in doses of 100 and 200 mg/kg treatment produced a significant decrease in FPI levels at day 40, however, there was no difference between both the groups. The baseline % beta cell function (HOMA-β) was similar in all the groups and administration of HFD for a period of 20 days resulted in significant increase in % beta cell function in all groups. However, the dose of 50 and 100 mg/kg DAGA did not significantly alter % beta cell function (Table).
The baseline HOMA-IR in all the groups was similar and administration of HFD for a period of 20 days resulted in significant increase in all the groups. Pioglitazone and DAGA in doses of 100 and 200 mg/kg treatment led to significant decrease in HOMA-IR at day 40. However, the decrease in HOMA-IR between both the groups was comparable (Fig. 1). The baseline AUC for glucose was similar in all the groups and administration of HFD for a period of 20 days resulted in significant increase of AUC for glucose. Pioglitazone and DAGA (100 and 200 mg/kg) treatment caused a significant lowering in AUC for glucose in both the groups at day 40. However, the difference between both the groups was comparable (Fig. 2).

- HOMA-IR (homeostasis model assessment - insulin resistance) at baseline, days 20 and 40 in different groups. Values mean±SD (n=6 in each group). *P<0.05 compared to baseline, £P<0.05 compared to normal group, #P<0.05 compared to pretreatment levels (day 20), $P<0.05 compared to vechicle and @P<0.05 compared to pioglitazone. HDF, high fructose diet; PIO, pioglitazone; DAGA, deacyl gymnemic acid.
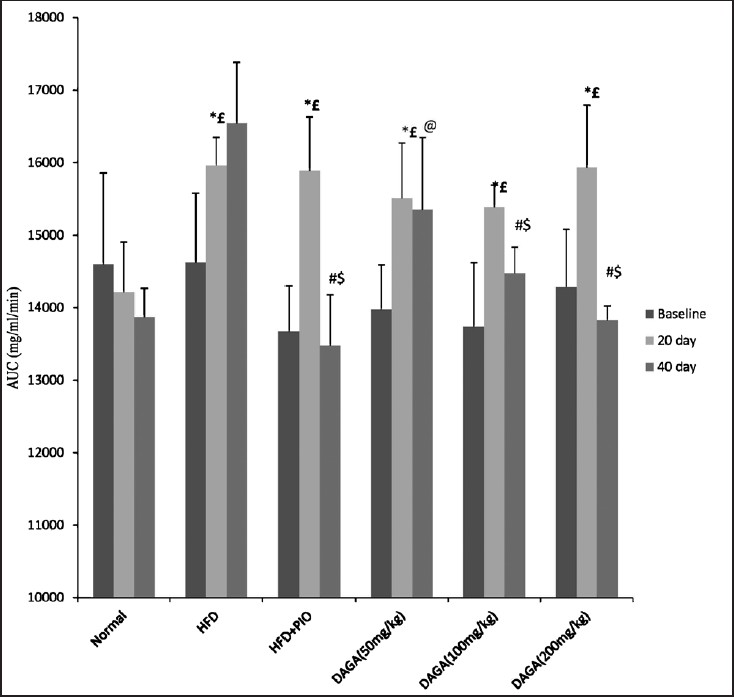
- Area under curve (AUG mg/dl/min) of OGTT at baseline, day 20 and 40 in different groups. Values are mean±SD (n=6 in each group) *P<0.05 compared to baseline, £P<0.05 compared to normal group, #P<0.05 compared to pretreatment levels (day 20), $P<0.05 compared to vehicle and @P<0.05 compared to pioglitazone. HFD, high fructose diet, PIO, pioglitazone, DAGA, deacyl gymnemic acid.
HFD administration led to an increase in triglyceride, total cholesterol and LDL-cholesterol level and decrease in HDL-cholesterol level at day 20. Treatment with DAGA at a dose of 200 mg/kg resulted in slight decrease in triglyceride and total cholesterol level. The extract at any dose level did not result in any alteration in HDL-cholesterol and LDL-cholesterol levels. However, statistical significance could not be assessed as lipid profile analysis was done in pooled samples.
Discussion
This study shows the beneficial effect of DAGA, a herbal ingredient derived from leaves of G. sylvestre, on various parameters of metabolic syndrome in a rat model induced by high fructose diet (HFD). Various rat models of the metabolic syndrome have been developed over the years. The prominent among them are obese Zucker diabetic fatty (ZDF) rat, obese Koletsky rat, obese ZSF1 rat, spontaneously hypertensive rat (SHR) and wistar-Kyoto (WKY) rat21. These are all genetic models of metabolic syndrome and usually associated with severe hyperglycaemia and β cell exhaustion. HFD induced rat model of metabolic syndrome has been widely employed in research studies22 since diet is implicated in the pathogenesis of metabolic abnormalities such as insulin resistance, hypertension and dyslipidaemia23.
Though there are no definite criteria to define metabolic syndrome in rats, some studies have used a serum triglyceride level of >130 mg/dl after HFD as a criterion to define metabolic syndrome22. In this study, we defined metabolic syndrome by 10 per cent increase in body weight and serum triglyceride of >130 mg/dl after HFD. All groups of animals achieved the defined criteria and in addition, there was 35-40 per cent increase in SBP and 20-25 per cent increase in FPG. Therefore, we could achieve almost all the metabolic abnormalities which constitute metabolic syndrome as defined in human beings.
In our study, DAGA in doses of 200 mg/kg decreased the levels of fasting plasma glucose accompanied with decrease in fasting plasma insulin, reduction in systolic blood pressure and modest improvement in lipid profile. This was associated with decrease in HOMA-IR, a surrogate marker of insulin resistance, suggesting that DAGA has beneficial effect on improvement in insulin sensitivity. The improvement in insulin sensitivity was not accompanied with a decrease in body weight thereby suggesting that the drug per se improves insulin sensitivity. The results are further strengthened by inclusion of a positive control group (pioglitazone), which is a well established insulin sensitizer acting through PPAR γ receptors24.
Since insulin resistance is the major contributory factor towards the development of metabolic syndrome25, the ability of DAGA to decrease HOMA-IR appears to be useful and worth pursuing further. This was further corroborated by corresponding decrease in β cell function as evidenced by HOMA-β. The β cell burden increases with HFD which may be attributed to compensatory increase in insulin secretion in response to increasing insulin resistance associated with weight gain. This finding appears to be contrary to the earlier reports in literature that G. sylvestre improves beta cell function in streptozotocin treated rats26. However, several reasons can explain this finding. Firstly, streptozotocin induced diabetes is a model for type 1 diabetes in which the main defect is loss of beta cell function27. The model used by us is a model of insulin resistance where beta cell function is not only preserved but also increased. Secondly, DAGA may have effects that are different from, and/or in addition to gymnemic acid. The mechanism of action of DAGA on glucose- insulin homeostasis is not well elucidated. Some studies have shown preservation of β cell function while others have shown improvement in insulin sensitivity1214.
The strengths of the study include induction of metabolic syndrome by high fructose diet mimicking the aetiopathogenesis of metabolic syndrome and prospective evaluation of efficacy of a herbal drug in a rat model of metabolic syndrome. The limitations of study include lack of comparison with crude extract and short duration of the study.
In conclusion, treatment with DAGA resulted in a significant decrease in insulin resistance accompanied with a decrease in systolic blood pressure and improved glucose and lipid profile without decreasing body weight in a rat model of metabolic syndrome. The molecular mechanisms leading to these effects need to be evaluated.
Acknowledgment
Authors acknowledge the Natural Remedies, Bangalore, India and Ind-Swift Pharmaceuticals, Chandigarh, India for providing drugs for this study.
Conflicts of interest: None.
References
- Prevalence of the metabolic syndrome among US adults: findings from the Third National Health and Nutrition Examination Survey. JAMA. 2002;287:356-9.
- [Google Scholar]
- The metabolic syndrome: prevalence in worldwide populations. Endocrinol Metab Clin North Am. 2004;33:351-5.
- [Google Scholar]
- Prevalence of diabetes, impaired fasting glucose and insulin resistance syndrome in an urban Indian population. Diabetes Res Clin Pract. 2003;61:69-76.
- [Google Scholar]
- Prevalence of metabolic syndrome among patients with stable coronary artery disease. Indian J Cardiol. 2003;6:72-6.
- [Google Scholar]
- Protective effects of ethanolic extract of Zingiber officinale rhizome on the development of metabolic syndrome in high-fat diet-fed rats. Basic Clin Pharmacol Toxicol. 2009;104:366-73.
- [Google Scholar]
- Enzyme changes and glucose utilization in diabetic rabbits: the effect of Gymnema sylvestre, R. Br. J Ethnopharmacol. 1983;7:205-34.
- [Google Scholar]
- Antidiabetic effect of a leaf extracts from Gymnema sylvestre in non-insulin-dependent diabetes mellitus patients. J Ethnopharmacol. 1990;30:295-300.
- [Google Scholar]
- Effect of feeding Gymnema sylvestre leaves on blood glucose in beryllium nitrate treated rats. J Ethnopharmacol. 1986;18:143-6.
- [Google Scholar]
- Effect of Gymnema sylvestre, R. Br. on glucose homeostasis in rats. Diabetes Res Clin Pract. 1990;9:143-8.
- [Google Scholar]
- Effects of seishin-renshi-in and Gymnema sylvestre on insulin resistance in streptozotocin-induced diabetic rats. Diabetes Res Clin Pract. 1995;29:11-7.
- [Google Scholar]
- Drug containing glycosides. In: Kokate CK, Purhoit AP, Gokhale SB, eds. Pharmacognosy. Mumbai, India: Nirali Prakashan; 2002. p. :167-254.
- [Google Scholar]
- Tail cuff blood pressure measurement without external preheating in awake rats. Hypertension. 1982;4:898-903.
- [Google Scholar]
- Effects of three different doses of a fruit extract of Terminalia chebula on metabolic components of metabolic syndrome, in a rat model. Phytother Res. 2010;24:107-12.
- [Google Scholar]
- Estimation of the concentration of low-density lipoprotein cholesterol in plasma, without use of the preparative ultracentrifuge. Clin Chem. 1972;18:499-502.
- [Google Scholar]
- Homeostasis model assessment: insulin resistance and β-cell function from fasting plasma glucose and insulin concentrations in man. Diabetologia. 1985;28:412-9.
- [Google Scholar]
- Rat Models of the Metabolic Syndrome. In: Goligorsky MS, ed. Methods in molecular medicine: Renal disease: Techniques and protocols. Totowa, NJ: Human Press Inc; 2003. p. :29-46.
- [Google Scholar]
- The protective role of Kangen-karyu against fructose-induced metabolic syndrome in a rat model. J Pharm Pharmacol. 2007;59:1271-8.
- [Google Scholar]
- Insulin, oral hypoglycemic agents, and the pharmacology of the endocrine pancreas. In: Brunton LL, ed. The pharmacological basis of therapeutics. New York: McGraw-Hill; 2006. p. :1613-45.
- [Google Scholar]
- Hepatic insulin resistance, metabolic syndrome and cardiovascular disease. Clin Biochem. 2009;42:1331-46.
- [Google Scholar]
- Possible regeneration of the islets of Langerhans in streptozotocin-diabetic rats given Gymnema sylvestre leaf extracts. J Ethnopharmacol. 1990;30:265-79.
- [Google Scholar]
- Streptozotocin-induced model of type 1 diabetes mellitus. Cesk Fysiol. 2006;55:96-102.
- [Google Scholar]






