Translate this page into:
Does awareness of diagnosis influence health related quality of life in north Indian patients with lung cancer ?
Reprint requests: Dr Ashutosh Nath Aggarwal, Department of Pulmonary Medicine, Postgraduate Institute of Medical Education & Research, Chandigarh 160 012, India e-mail: aggarwal.ashutosh@outlook.com
-
Received: ,
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Background & objectives:
Several patients with cancer in India are not aware of their diagnosis. We evaluated the impact of awareness of cancer diagnosis on health-related quality of life (HRQL) in newly diagnosed patients with lung cancer.
Methods:
A total of 391 treatment-naïve patients with lung cancer, seen at the Lung Cancer Clinic of a tertiary care hospital in north India, were categorized into those aware of their diagnosis (group A) and those not aware (group B). All patients answered Hindi versions of abbreviated World Health Organization Quality of Life questionnaire (WHOQOL-Bref) and European Organization for Research and Treatment of Cancer Quality of Life questionnaire (EORTC QLQ-C30), and its lung cancer module, EORTC QLQ-LC13. Various domain scores were computed and compared between the two groups. Analysis of covariance was used to determine significance of differences after adjustment for potential confounding factors.
Results:
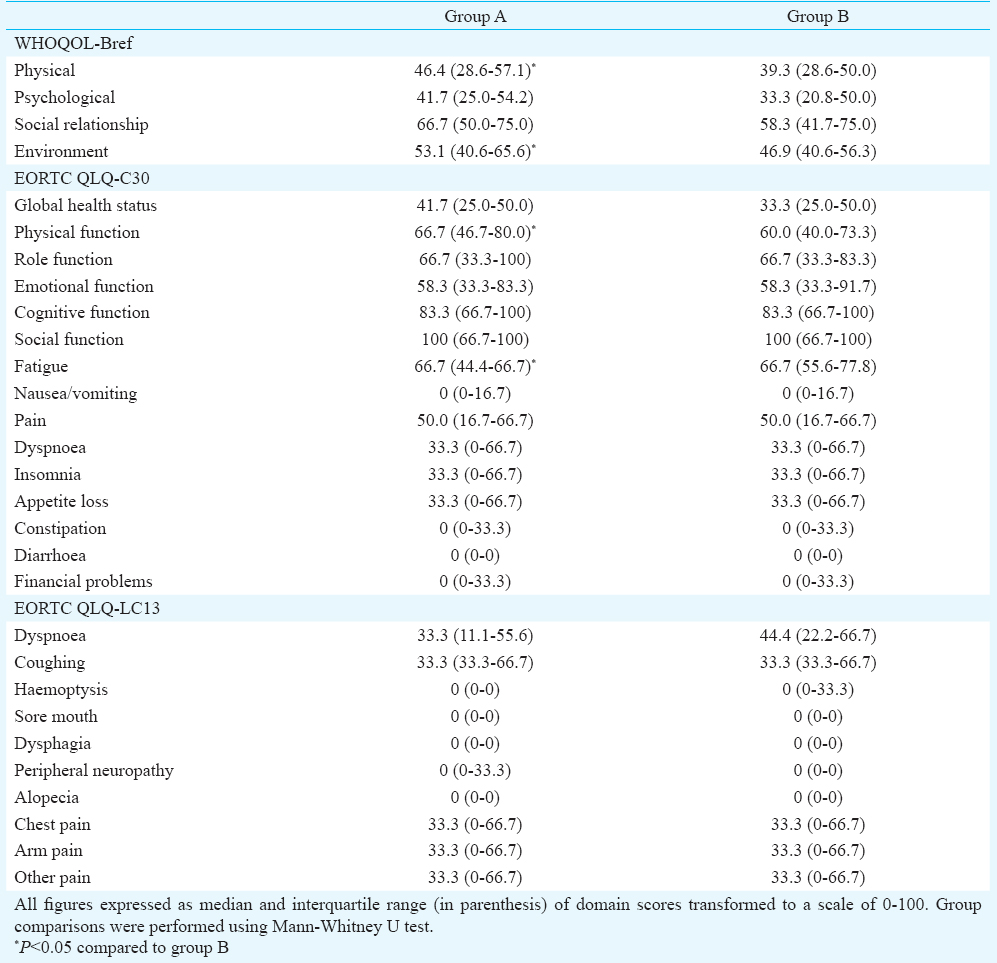
Only 117 (29.9%) patients were aware of their diagnosis. Of all, 302 (77.2%) patients had non-small cell lung cancer, and 301 (77.0%) had advanced disease. All HRQL domain scores were similar between the two groups, except that group B patients had significantly poorer median (interquartile range) Physical [39.3 (28.6-50.0) vs 46.4 (28.6-57.1)] and Environment [46.9 (40.6-56.3) vs 53.1 (0.6-65.6)] domain scores of WHOQOL-Bref, and Physical function [60.0 (40.0-73.3) vs 66.7 (46.7-80.0)] and Fatigue [66.7 (55.6-77.8) vs 66.7 (44.4-66.7)] scores of QLQ-C30. After adjusting for gender, age, education, family income, and tumour extent, these differences were not significant.
Interpretation & conclusions:
Disclosure of cancer diagnosis, or lack of it, had no significant impact on HRQL in patients with lung cancer after adjustment of potential confounders.
Keywords
Communication
India
lung neoplasms
quality of life
questionnaires
truth disclosure
The issue whether cancer patients should be told about their diagnosis has long been debated. Most patients with malignancy want to be told about the nature of their disease and its prognosis1. However, it is common in India not to disclose a diagnosis of malignancy to the patient23. In most instances, family members and close relatives discuss the diagnosis and therapeutic options with the treating physician, and make decisions on the patient's behalf. It is commonly perceived that if an unprepared patient is made aware of the cancer diagnosis, this news may create a huge psychological burden and feeling of despair, and the patient will lose all hope to live4. Similar beliefs are culturally engrained in several societies around the world567. Further, the cost associated with cancer and its treatment in a resource-poor setting is thought to add to patient's psychological distress. However, the relationship between knowledge of diagnosis and psychological adaptation and psychiatric morbidity is variable and complex. In a previous study from south India, though no differences in patterns and prevalence of psychiatric morbidity were noted between patients aware and not aware of a cancer diagnosis; yet more patients unaware of their diagnosis refused treatment for psychological distress8. In contrast, two studies reported higher prevalence of psychiatric disorders, especially depression, in cancer patients aware of their diagnosis910.
If knowledge of cancer diagnosis results in additional psychological or emotional distress, one would expect impairment of health-related quality of life (HRQL) among these patients. As opposed to a physician evaluation, HRQL measures the impact of any health condition as it is perceived by the patient. A study on 100 Turkish cancer patients showed that awareness of diagnosis did not impair any HRQL domain in general or emotional functioning in particular11. Another study on 142 Iranian patients found that patients aware of cancer diagnosis had lower degree of physical, emotional and social functioning12. A study from Korea on 100 patients with advanced malignancy reported significantly higher degree of social, emotional and role functioning, and lower fatigue, anorexia, constipation, anxiety and financial difficulties, among patients aware of their diagnosis compared to those who were not13. Terminally ill cancer patients aware of their disease status had poor survival and HRQL in another study from China14. A recent systematic review has also shown mixed findings regarding the impact of patients’ awareness of metastatic cancer on HRQL15.
Lung cancer is a common malignancy worldwide, especially among men. Its diagnosis is often delayed in India and most patients present with advanced and inoperable disease. Previous studies have shown that disclosure of diagnosis affects HRQL variably, with one study showing impairment, and another showing no effect1617. Similar data are not available for Indian patients. Therefore, this study was planned to evaluate if awareness of cancer diagnosis significantly influenced HRQL in newly diagnosed patients of lung cancer reporting for chemotherapy.
Material & Methods
The study was conducted at the Lung Cancer Clinic at Postgraduate Institute of Medical Education and Research, Chandigarh, India, over a two year period (April 2009 to March 2011). Adult consecutive patients (aged more than 20 yr), with cytologically or histologically proven bronchogenic carcinoma and willing for chemotherapy, were eligible for inclusion in the study. The cancer diagnosis was disclosed to the patients, unless family members specifically requested the clinician not to do so, when they presented with a confirmatory report after diagnostic workup. For patients to whom cancer diagnosis was not disclosed by the clinician, we directly enquired if they knew the nature of their disease. Accordingly, patients were categorized into those aware of their diagnosis (group A) and those not aware (group B). Evaluation for this study was conducted when the patient presented for assessment for chemotherapy to the Lung Cancer Clinic, which was usually around two weeks after diagnosis. Patients who had earlier received treatment with surgery, chemotherapy and/or radiotherapy for the same disease, before evaluation for inclusion into the study, were excluded. Patients with major comorbidity (such as neuropsychiatric illness or severe cardiorespiratory disorder) were also excluded from the study, to minimize potential confounding by other disease processes. The study protocol was approved by the Institutional Review Board, and informed consent was obtained from all participants, for collection of disease-related information and HRQL assessment, prior to their inclusion into the study.
Baseline demographic and clinical data were recorded for all patients. Non-small cell cancer was staged using standard TNM classification based on tumour size and extension (T), lymph nodal involvement (N), and presence of distant metastasis (M) in use during the period of study18. Small cell cancer was staged as either limited (disease restricted to one hemithorax, with or without regional lymph node metastases and/or ipsilateral pleural effusion) or extensive19. Performance status was scored using Eastern Cooperative Oncology Group (ECOG) scale20. All patients completed Hindi versions of a generic and a disease specific HRQL measure themselves. Abbreviated World Health Organization Quality of Life scale (WHQOL-Bref) was used as the generic instrument. This instrument measures HRQL in four domains (physical, psychological, social relationships, and environment) using a seven point Likert scale for 26 items, with a recall period of two weeks21. Higher domain scores reflect better HRQL. The European Organization for Research and Treatment of Cancer Quality of Life Questionnaire (EORTC QLQ-C30) and its lung cancer module (EORTC QLQ-LC13) were used as the disease specific HRQL instrument2223. EORTC QLQ-C30 is a 30-item questionnaire that assesses HRQL using five functional scales (physical, role, social, emotional and cognitive), three symptom scales (fatigue, nausea, and vomiting and pain), a global health status scale and six single items (dyspnoea, insomnia, anorexia, diarrhoea, constipation and financial difficulties) over a one-week time frame. High scores on functional scales and global health status scale reflect better HRQL, while high scores on symptom scales/items reflect poorer HRQL. This core measure is supplemented by a disease specific 13-item EORTC QLQ-LC13. In accordance with guidelines for scoring these questionnaires, all scores were linearly transformed to a scale ranging from 0 to 100 prior to data analysis.
Statistical analysis: Baseline characteristics between the two groups were compared using chi square test (for categorical data) or Mann-Whitney U test (for scalar data). HRQL data were expressed as median and interquartile range (IQR) in view of anticipated non-normal distribution, and compared between groups using Mann-Whitney U test. Analysis of covariance (ANCOVA) was used to determine if differences in HRQL between groups A and B were significant after adjusting for age, gender, years of education, monthly family income, and tumour extent (advanced disease or not).
Results
A total of 391 patients (332 men and 59 women, mean age 58.0 ± 10.6 yr) were enrolled for the study. Most patients were residents of Chandigarh or neighbouring States of Punjab, Himachal Pradesh and Haryana (14.8, 25.1, 22.8 and 19.7%, respectively). Majority of patients had non-small cell lung cancer (302, 77.2%), and had advanced disease (301, 77.0%). Of them, only 117 (29.9%) were aware of their diagnosis (group A). There were no significant differences in gender, age, smoking history, tumour histology, or tumour extent between patients in groups A and B (Table I). Patients in group A were better educated than those in group B [median (interquartile range, IQR) 10 (5-10) vs. 5 (0-10) yr; P<0.001], but had similar monthly family income [median (IQR)  5000 (3000-12000) vs.
5000 (3000-12000) vs.  5000 (3000-9000); P<0.051]. Patients in group A had a better ECOG status as compared to patients in group B [median (IQR) 2 (1-2) vs. 2 (1-3) yr; P<0.001].
5000 (3000-9000); P<0.051]. Patients in group A had a better ECOG status as compared to patients in group B [median (IQR) 2 (1-2) vs. 2 (1-3) yr; P<0.001].
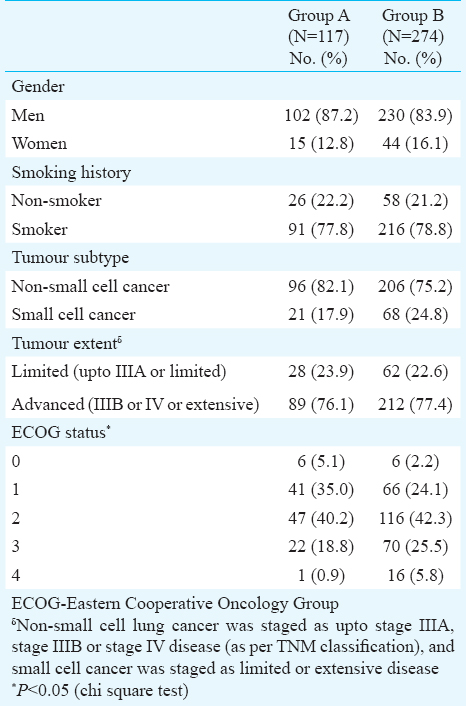
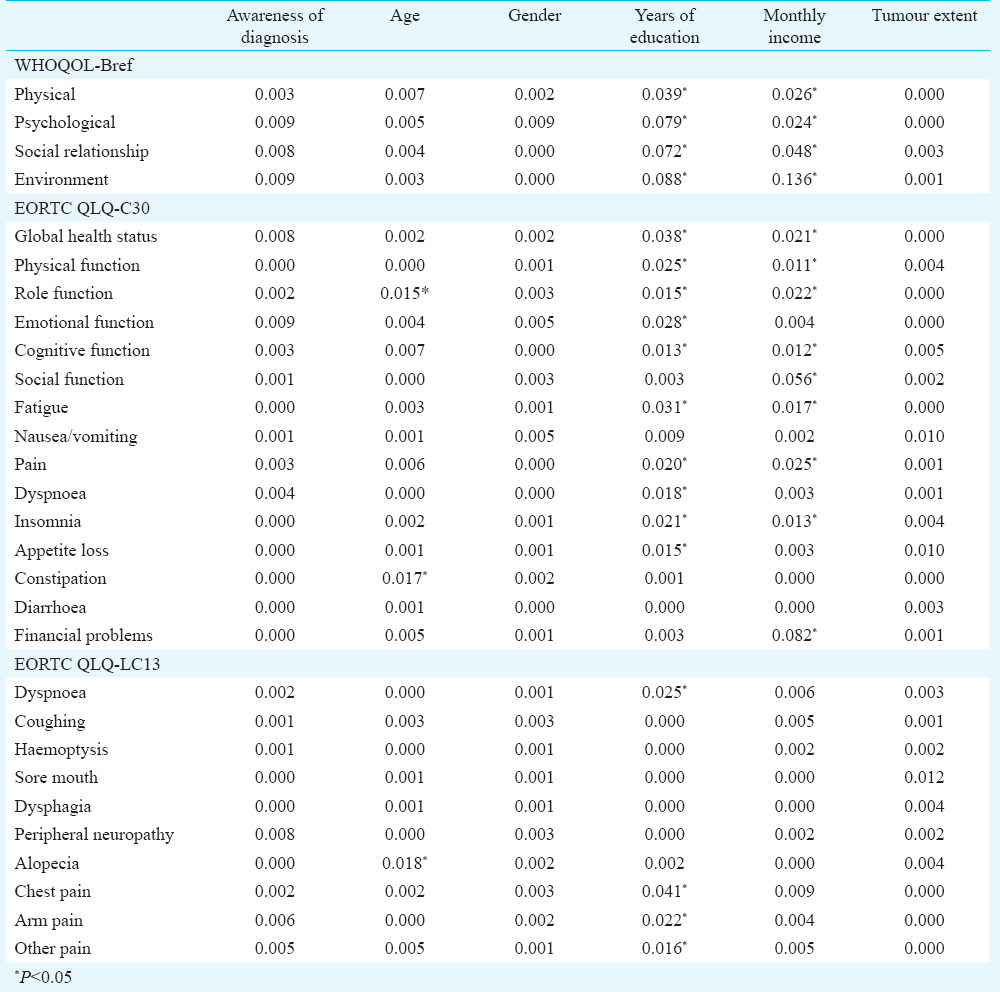
Physical and Environmental domain scores of WHOQOL-Bref were higher in group A patients, while the other two domain scores were similar between the two groups (Table II). All scales/items of EORTC QLQ-C30 and EORTC QLQ-LC13 were similar in the two groups, except for Physical function and Fatigue scales of EORTC QLQ-C30 (Table II). Gender, age, education, family income and tumour extent were significantly correlated with various domain scores of WHOQOL-Bref and functional scale scores of EORTC QLQ-C30. Hence these variables were included as covariates in ANCOVA models to identify if awareness of diagnosis influenced HRQL after adjustment of these potential confounders. After adjustment for gender, age, education, family income and tumour extent, ANCOVA analysis showed all scales/items to be similarly scored between the two groups, indicating no significant differences in HRQL. The effect size of years of education and monthly family income was, however, significant for most domains studied (Table III).
Discussion
We evaluated 391 treatment-naïve patients with lung cancer and studied differences in HRQL based on their awareness of diagnosis, using both generic and disease-specific questionnaires. Similar scores were found for most HRQL domains between patients aware and not aware of their diagnosis. Only Physical and Environmental domain scores of WHOQOL-Bref, and Physical function and Fatigue scores of QLQ-C30, were better among patients aware of their diagnosis. After adjusting for potential confounders, HRQL scores were not significantly different between the two groups.
In this study, nearly 70 per cent of patients reporting for chemotherapy were not aware of their lung cancer diagnosis. While most patients with cancer wish to be told their diagnosis, most caregivers want to know the truth without it being disclosed to the patient3. In several developed countries, clinicians have a legal and ethical responsibility to inform patients about their disease, and its prognosis and management7. In India, socio-cultural conditions and perceptions still impede disclosure of several diseases, and cancer in particular. This also reflects a level of support from family and caregivers, and may be viewed as a positive social resource for the patient.
Clinical characteristics of the two groups in this study were largely similar, except that patients unaware of their diagnosis had an overall worse ECOG performance status. It is possible that the poorer general condition of these patients, coupled with the fact that most patients studied had advanced disease, might have influenced the family's decision to withhold the diagnosis from some of them. In earlier studies from Greece and Turkey, persons accompanying patients with metastatic cancers were more likely to request treating doctors not to disclose the diagnosis to patients2425.
Patients in both groups had similar HRQL scores across nearly all domains. Patients unaware of their diagnosis had poorer scores in ‘physical’ domain of WHOQOL-Bref, and ‘Physical function’ and ‘ Fatigue’ domains of EORTC QLQ-C30. These could be a reflection of the poorer performance status of these patients as compared to those who were aware of their diagnosis. It is important to note that after adjusting for tumour extent and other baseline socio-demographic factors, all HRQL scores were similar between the two groups. This suggests that awareness of diagnosis did not significantly influence HRQL in these patients. Previous studies carried out in patients with lung cancer have shown varied results. In one study, 70 hospitalized patients completed the EORTC QLQ-C30 and EORTC QLQ-LC13 when they were unaware of the diagnosis, and at initiation of treatment after disclosure of diagnosis16. Physical function, role function, social function and emotional function domain scores significantly deteriorated at second evaluation, suggesting impairment of HRQL after disclosure of diagnosis. Another study used the Nottingham Health Profile, EORTC QLQ-C30 and EORTC QLQ-LC13 on 129 Scottish patients of lung cancer, of whom only 30 (23.3%) knew their diagnosis. All domain and symptoms scores were similar between patients aware and not aware of their diagnosis, except that the latter group reported more sleep difficulties on the EORTC QLQ-C3017. Studies on patients with other malignancies have variably shown HRQL to be similar, worse or better in patients aware of a cancer diagnosis111213.
For this study, questionnaires were chosen carefully. For a comprehensive evaluation, a generic instrument was combined with a cancer-specific instrument having an additional lung cancer-specific module. Both questionnaires were available in a standardized Hindi version, and were thus administered in a language easily understood by our patients. Further, none of the items in any of the questionnaires contained any reference to ‘cancer’ that could have influenced responses from a patient unaware of his diagnosis. We focused only on one specific malignancy to avoid heterogeneity in our data. Still, our study had some limitations. Our institute is a tertiary referral centre for diagnosis and management of lung cancer, and our results may not be generalizable to other clinical settings. A ‘referral bias’ could be responsible for the higher proportion of patients with advanced malignancy. As patients in group A were already aware of their diagnosis for some time, it could not be ruled out if this disclosure itself had resulted in any short-term psychological impact (e.g. anxiety, depression, etc.) on these patients. However, a previous study has shown that knowledge of cancer diagnosis does not significantly alter the way patients handle HRQL questionnaires17. This was a cross-sectional evaluation soon after establishing the diagnosis, and it is possible that alterations in HRQL (both overall and in specific domains) might have been naturally delayed in some of these patients. However, HRQL assessment could not be repeated as all these patients were scheduled to receive chemotherapy. Information on baseline HRQL in these patients was not available. Further, there can be cultural and regional differences in the way patients with malignancy perceive their HRQL, and hence our results may not be generalizable to other areas of the country.
In conclusion, most patients of lung cancer evaluated in this study were unaware of their diagnosis. All HRQL domain scores were similar between patients aware and not aware of their diagnosis, except for Physical and Environmental domain scores of WHOQOL-Bref and Physical function and Fatigue scores of QLQ-C30 which were better among patients aware of their diagnosis. However, after adjusting for potential confounders, disclosure of cancer diagnosis, or lack of it, had no significant impact on HRQL in these patients.
Acknowledgment
The study was supported in part by a research grant from the Indian Council of Medical Research, New Delhi, India.
Conflicts of Interest: None.
References
- Attitude of cancer patients toward diagnosis disclosure and their preference for clinical decision-making: a national survey. Arch Iran Med. 2014;17:232-40.
- [Google Scholar]
- Are oncology patients aware of their diagnosis? A survey from Calicut. Indian J Palliat Care. 2004;10:39-40.
- [Google Scholar]
- Ethical dilemmas in palliative care in traditional developing societies, with special reference to the Indian setting. J Med Ethics. 2008;34:611-5.
- [Google Scholar]
- To tell the truth: a cancer diagnosis in other cultures is often a family affair. J Natl Cancer Inst. 1999;91:1918-9.
- [Google Scholar]
- Cancer information disclosure in different cultural contexts. Support Care Cancer. 2004;12:147-54.
- [Google Scholar]
- Disclosing the truth to terminal cancer patients: a discussion of ethical and cultural issues. East Mediterr Health J. 2010;16:442-7.
- [Google Scholar]
- Awareness of diagnosis and psychiatric morbidity among cancer patients - a study from South India. J Psychosom Res. 1998;45:257-61.
- [Google Scholar]
- Prevalence of psychiatric disorder in asymptomatic or minimally symptomatic cancer patients on treatment. J Cancer Res Ther. 2006;2:136-9.
- [Google Scholar]
- Psychiatric morbidity among cancer patients and its relationship with awareness of illness and expectations about treatment outcome. Acta Oncol. 1993;32:623-6.
- [Google Scholar]
- Does awareness of diagnosis make any difference to quality of life? Determinants of emotional functioning in a group of cancer patients in Turkey. Support Care Cancer. 2002;10:51-7.
- [Google Scholar]
- Disclosure of cancer diagnosis and quality of life in cancer patients: should it be the same everywhere? BMC Cancer. 2009;9:39.
- [Google Scholar]
- Awareness of incurable cancer status and health-related quality of life among advanced cancer patients: a prospective cohort study. Palliat Med. 2013;27:144-54.
- [Google Scholar]
- Does awareness of terminal status influence survival and quality of life in terminally ill cancer patients? Psychooncology. 2013;22:2206-13.
- [Google Scholar]
- The impact of patients’ awareness of disease status on treatment preferences and quality of life among patients with metastatic cancer: A systematic review from 1997-2014. J Palliat Med. 2015;18:176-86.
- [Google Scholar]
- Quality of life in lung cancer: does disclosure of the diagnosis have an impact? Lung Cancer. 2004;43:175-82.
- [Google Scholar]
- Does knowledge of cancer diagnosis affect quality of life? A methodological challenge. BMC Cancer. 2004;4:21.
- [Google Scholar]
- Sobin LH, Wittekind C, eds. TNM classification of malignant tumours (6th ed). Hoboken: New Jersey; John Wiley & Sons; 2002.
- Staging and prognostic factors in small cell lung cancer: a consensus report. Lung Cancer. 1989;5:119-26.
- [Google Scholar]
- Toxicity and response criteria of the Eastern Cooperative Oncology Group. Am J Clin Oncol. 1982;5:649-55.
- [Google Scholar]
- WHOQOL-Hindi: a questionnaire for assessing quality of life in health care settings in India. World Health Organization Quality of Life. Natl Med J India. 1998;11:160-5.
- [Google Scholar]
- The European Organization for Research and Treatment of Cancer QLQ-C30: a quality-of-life instrument for use in international clinical trials in oncology. J Natl Cancer Inst. 1993;85:365-76.
- [Google Scholar]
- The EORTC QLQ-LC13: a modular supplement to the EORTC Core Quality of Life Questionnaire (QLQ-C30) for use in lung cancer clinical trials. EORTC Study Group on Quality of Life. Eur J Cancer. 1994;30A:635-42.
- [Google Scholar]
- The families evaluation on management, care and disclosure for terminal stage cancer patients. BMC Palliat Care. 2002;1:3.
- [Google Scholar]
- “Do not tell”: what factors affect relatives’ attitudes to honest disclosure of diagnosis to cancer patients? Support Care Cancer. 2004;12:497-502.
- [Google Scholar]






