Translate this page into:
Development of a screening instrument for autism spectrum disorder: Chandigarh Autism Screening Instrument
For correspondence: Dr. Priti Arun, Department of Psychiatry, Government Medical College & Hospital, Sector 32, Chandigarh 160 030, India e-mail: drpritiarun@gmail.com
-
Received: ,
This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Background & objectives:
There is a paucity of trained professionals for the diagnosis of autism spectrum disorder (ASD), and a large number of cases go undetected and are diagnosed only during adolescence. There is no screening instrument specifically developed for screening of Indian population for ASD. This study was undertaken to develop a screening instrument to screen ASD in north Indian Hindi speaking population by multipurpose health workers.
Methods:
A 37-item instrument in Hindi with dichotomous yes/no responses [Chandigarh Autism Screening Instrument (CASI)] was developed to be applied on children aged 1.5-10 yr. The instrument was pilot tested and then reliability and validity of this instrument were tested. The sample included children with intellectual disability (n=75), ASD (n=83), other developmental disorders (n=87) and typically developing children (n=160).
Results:
Reliability, construct and content validity testing of the instrument were performed, and a score of 10 as cut-off had sensitivity of 89.16 per cent, specificity of 89.13 per cent, positive predictive value of 67.89 per cent and negative predictive value of 96.96 per cent. A shorter four-item version (CASI Bref) has also been developed with good sensitivity (73.49%) and specificity (90.68%) at a cut-off score of 2.
Interpretation & conclusions:
CASI was found to be a valid instrument for screening general Hindi speaking population of north India with adequate sensitivity and specificity.
Keywords
Autism
autism screening
CASI
community survey
screening questionnaire
sensitivity
validity
Autism is a neuro-developmental disorder with a prevalence of 14.7/1000 in the USA1. Prognosis is better if detection and intervention start in early childhood. In India most studies are based on the clinic-based data. A community survey could not be carried out due to lack of a good screening instrument. Indian Scale for Assessment of Autism (ISAA) was the first tool developed in India by National Institute for Mentally Handicapped for the National Trust2. Earlier, it was used for making a diagnosis and assessment of disability in children with autism. In 2016, Government of India issued a notification, wherein the ISAA was notified for the assessment of disability, and another instrument INCLEN-autism spectrum disorder (ASD) was notified for making diagnosis3. There has not been any instrument developed in India for the purpose of community survey for ASD.
There are two published studies reporting the prevalence from community sample. In a study from Kerala, a prevalence of 23.3/10,000 population was reported4. In this study, a survey of chronic diseases including developmental disabilities was carried out using a non-standardized questionnaire on the whole population. In another study, Hindi version of ISAA was used to survey children and a prevalence of 0.9/1000 was reported5.
Many parents who have autistic children are unaware about the existence of the disorder till mid-10 years. Often, autism is misunderstood with hearing difficulties, mental retardation (MR) and attention-deficit hyperactivity disorder (ADHD). Clinical evidence suggests that early identification and intervention lead to better outcome of cognitive and behavioural problems of the autistic children67.
For any prevalence study, it is important to have an adequate sample size and an appropriate and valid screening instrument. Western scales apart from question of appropriateness in Indian conditions are prohibitively expensive and hence make it difficult to carry out proper research work. For India with its large population, locally developed instruments must be available to conduct the prevalence studies. Questionnaires developed in other languages and then translated become difficult to use. Questionnaire requires to be retested if it is used for another purpose. Hence, the present study was aimed to construct a screening instrument for screening ASD in north Indian Hindi speaking population and to test the reliability and validity of a brief four-item screening instrument for the diagnosis of ASD.
Material & Methods
The study was conducted over a period of six months from August 2014 to February 2015 at the department of Psychiatry, Government Medical College and Hospital (GMCH), Chandigarh, India. The study was approved by the institutional research and ethics committee. The term ASD has been used for conceptual clarity. However, for making the diagnosis of individuals included in the present study, the Diagnostic and Statistical Manual IV Edition Text Revised (DSM IV TR)8 was used. The following steps were taken for the study:
-
Literature review: For the purpose of construction of screening instrument [Chandigarh Autism Screening Instrument (CASI)], a comprehensive literature review of ASD was done to find out necessity of a new screening instrument and to systematically accumulate initial item pool. Primarily, the literature searched was DSM IV TR, standard textbooks of psychiatry9 and child psychiatry1011 and existing screening scales available in English language212. In addition, parents coming to child guidance clinic (CGC) were interviewed to understand what symptoms they had first noticed.
-
Conceptualization: For the purpose of constructing the screening instrument, DSM-IV TR was used as it is closer to International Classification of Diseases (ICD-10), Classification of Mental and Behavioural Disorders13 in terms of its construct. Autism is a well-defined construct having three apparent facets/domains (i.e. socialization, language/communication and repetitive/ritualistic behaviour).
-
Item generation: Focussed group discussions (FGDs) were conducted by three psychiatrists and two psychologists. Initial discussions were centered on early symptoms and how to enquire about them. For making the initial item pool, all aspects of the ASD were included. In many items, the words of the parents were incorporated. Level of understanding of health workers expected to use the instrument was kept in mind.
The item pool of 100-items was prepared in English. The FGDs were carried out on each item to choose appropriate and specific items for the proposed scale. At this stage of discussion, spoken Hindi was kept as the language for scale construction. Of the 100 items, 37 items were retained. On the basis of diagnostic value, the remaining items were discarded because of item ambiguity, repetition and linguistic complexity. Some items were rephrased and a few double-barrelled items were divided further as those were focusing on separate areas. Examples were added to 10 items to make them comprehensible to the respondents. Examples were added to the items such as ‘does your child look at what you are pointing at, e.g. moon, bird, flower’ (Item no. 1) and ‘does your child play imaginary games like talking on phone, playing with dolls or setting up a toy shop’ (Item no. 12). In addition, the dichotomous response format of ‘Yes’ and ‘No’ was finalized for the questionnaire. The age range of 1½-10 yr was selected for the study as it was observed that 1½ yr was the earliest time when parents became aware of behavioural issues of the child. Upper age was kept at 10 yr as many cases were brought to clinical services till 10 yr of age and beyond. Moreover, the constructed items would not be applicable beyond this age.
Pilot testing: After the finalization of the initial item pool, a pilot study was conducted. For this purpose, the 37-item version (CASI) was administered on 10 mental health professionals comprising five psychologists, three psychiatrists, one psychiatric social worker and one psychiatric nurse. The respondents’ feedback revealed a few shortcomings of the screening instrument. Consequently, four items were rephrased, two were removed, one was added and another one item was divided into two items. The revised screening instrument finally retained 37 items (Table), with a response format of ‘Yes’ and ‘No’.
To have a brief and short version, four core items pertaining to the essential features of ASD were selected for the construction of a brief screening instrument. The brief screening instrument (CASI Bref) included core items with a response format of ‘Yes’ and ‘No’. These items were pertaining to eye contact, ability to communicate needs through verbal or non-verbal means, peer interaction and odd, repetitive behaviour.
Reliability and validity
Sample: For testing the reliability and validity of the instrument, item to response ratio of 1:10 was decided. Since initial tool had 37 items, a sample size of 405 children was taken. The sample included children with intellectual disability (n=75), ASD (n=83), other developmental disorders (n=87) and typically developing children (n=160). All the parents had conversational knowledge of Hindi. Of the total sample, there were 266 boys (65.7%), girls to boys ratio was 1:1.92, mean age was 6.24±2.18 yr, 239 children (59%) were attending regular school and 36 (8.9%) were receiving special education. Information was collected from mothers only for 217 children (53.6%), from both parents in 54 (13.3%) and from fathers only for 134 (33.1%) children. Children were excluded if they had any serious medical or neurological illness, if parents were not able to converse in Hindi or if parents were not able to provide information regarding their ward due to any reason such as not staying with the child.
The sample was drawn as the following:
-
Pervasive developmental disorder (PDD) and MR: Children who were diagnosed with autistic disorder, Asperger syndrome or pervasive developmental disorder not otherwise specified as per the DSM IV TR either coming for follow up or recently diagnosed were included in the ASD group. This sample was taken from the department of Psychiatry, GMCH, the Government Rehabilitation Institute for Intellectual Disabilities (GRIID), Rehabilitation Centre for Handicapped Children-PRAYAAS and the Society for Rehabilitation of Mentally Challenged, Chandigarh. Children with intelligence quotient (IQ) <70 without PDD were included in the intellectual disability category. MR was diagnosed by IQ testing. IQ tests were administered by qualified psychologists. From a battery of intelligence tests, at least two tests were administered as part of standard practice in the GRIID.
-
Children with other developmental disorders were drawn from CGC of department of Psychiatry, GMCH. These children were diagnosed with behavioural disorders such as ADHD, somatization disorder and specific developmental disorder of scholastic skills. Children having intellectual disability or ASD were excluded.
-
For inclusion of typically developing children, permission was sought from the authorities of regular schools in the vicinity of GMCH. The consent of parents was obtained through the school principals. Teachers were asked about any problem behaviour of the children. Parents who did not have concern about child's behaviour were included.
Instruments: For external validation, autism behaviour checklist (ABC)14 and MCHAT12 were used. The issue of language difficulty in the ABC questionnaire was resolved before the final administration. Examples were generated for 22 items of the ABC questionnaire exclusively with the purpose of making the items comprehensible to the respondents. ABC was administered for children above two years of age. For children younger than two years, modified checklist for autism for toddlers (MCHAT) was used (n=6). MCHAT and ABC both were administered on children who were 2-3 yr of age (n=12).
Permission for data collection was sought from the designated authorities. The parents of children aged 1½-10 yr were approached. Parents were provided the details of the study and those willing to participate were included. Screening instrument and MCHAT and/or ABC were administered to parents. The caregivers who were comfortable in completing the study questionnaires were allowed to complete the screening instrument themselves, and the rest of the parents were administered screening instrument by the research workers.
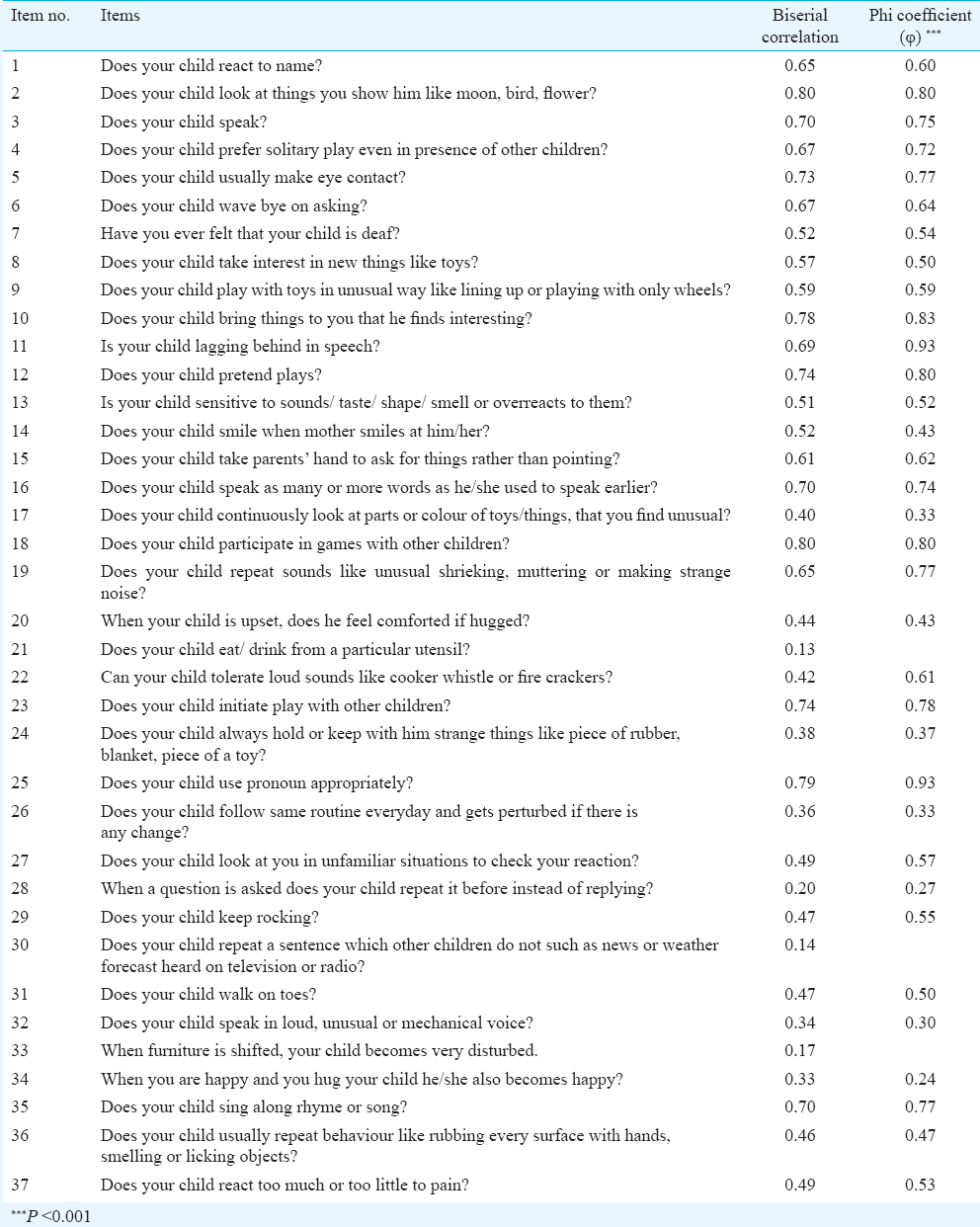
Statistical analysis: After collection of data on preliminary version of screening instrument, item analysis was done. For analysis, first, a biserial correlation was done on each item taking total score versus score on each item. Phi coefficient was calculated taking those who scored 27 per cent on both extremes. Item-wise Chi-square was applied on the four groups, i.e. autism, MR, other developmental disorders and typically developing children. For external validation, each item was validated using ABC and MCHAT in autism and non-autism group and on whole sample. Discrimination index and split half coefficient were calculated. Analysis was done using SPSS version 16 (SPSS Inc., USA).
Results
The items of screening instrument had adequate validity against MCHAT and ABC. Item-wise Chi-square was applied on four groups, and the value was non-significant on item number 21 (0.402), whereas on rest of the items, it was significant. On biserial correlation, four items (21, 28, 30, and 33) had coefficient value <0.3 (Table). Thus, item numbers 21, 30, and 33 were deleted from the final analysis as these items had discrimination index <10. Item number 28 was retained as it was very specific to autism, had discrimination index of 13.93. Furthermore, there was significant difference on this item between ASD group and MR group (P <0.001). Thus, final instrument had 34 items.
Cut-off score of ≥10 had a sensitivity of 89.16 per cent and specificity of 89.13 per cent. Positive predictive value was 67.89 per cent and negative predictive value was 96.96 per cent. Split half coefficient was 0.858 showing adequate reliability. The Figure shows receiver operating characteristic curve of the screening instrument. The area under the curve was found to be 0.947, suggesting that a score of 10 was a good cut-off score.
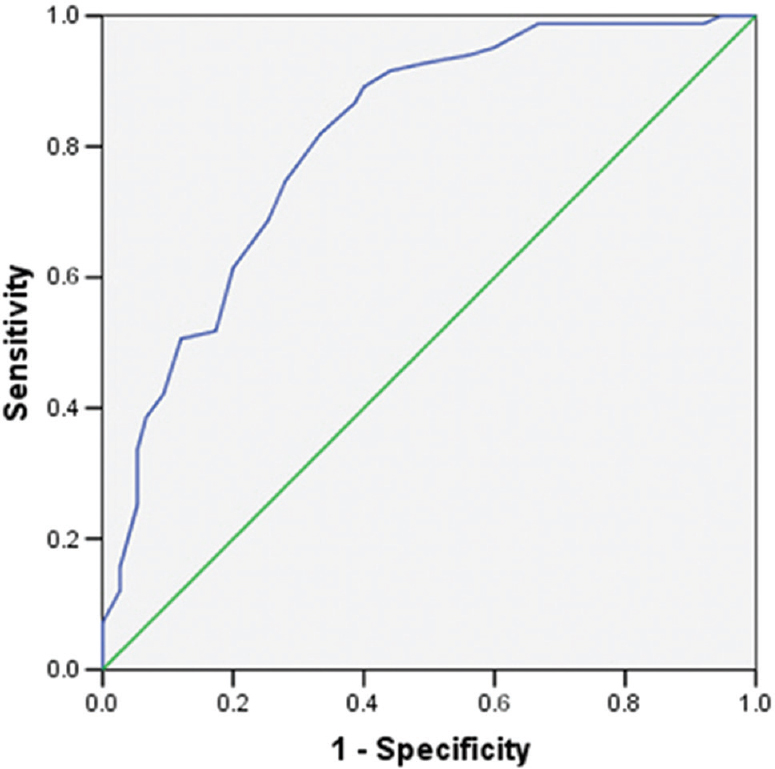
- Receiver operating characteristic (ROC) curve of screening instrument. Diagonal segments are produced by ties.
A short screening instrument of four items was also administered to all the children. This short screening instrument of ‘core items’ was able to distinguish between children with ASD and others at cut-off 2 with sensitivity 73.49 per cent and specificity 90.68 per cent. It had a positive predictive value of 67.03 and negative predictive value of 92.99 per cent. Short screening instrument had a good agreement with screening instrument having kappa value of 0.775.
Discussion
Most research in autism has been done in developed countries. This is due to high cost of tools and training in use of these tools15. CASI instrument developed in the present study was found to have a sensitivity of 89.16 per cent and specificity of 89.13 per cent at a cut-off score of 10. MCHAT which was developed for use in well baby clinic had a sensitivity of 87 per cent and specificity 99 per cent12. The sensitivity of ABC was found to be 54 per cent in a study from Italy16. ABC was developed to identify autistic behaviours in intellectually disabled and severely disabled children. ABC is easy to use and can be applied by parents, but cut-off needs to be set17. Various authors have suggested a different cut-off score. High false negative (46%) score was seen with a lower cut-off score of 5316. In the absence of any screening instrument designed specifically for Indian population, Indian studies have used ISAA and other non-standardized scale for the purpose of screening45.
Since labelling a child with ASD will have lifelong consequences, the instrument should be reliable and with adequate psychometric properties. Instrument reliability depends on various factors. The language in which instrument was developed is of prime importance. Many scales are available in English language for screening of children that can be used by professionals such as MCHAT, ABC and others. Some questionnaires are to be filled by parents, e.g. Social Responsiveness Scale (SRS)18. Translation of an instrument in English into Hindi before administration will be inconsistent without uniformity conveying different message and thus eliciting inconsistent information. Further, some of the expressions are difficult to translate into Hindi. Sometimes, many expressions when translated lose the exact meaning and require some explanation to convey the meaning. Thus, brief and reliable screening instrument for ASD in Hindi was required for north India.
To find out the percentage of persons with ASD who have access to mental healthcare services, a study from the USA reported that only one-fourth of children were reaching mental health care services19. Situation in India is expected to be far worse due to limited number of health professionals who are trained to diagnose ASD. There is evidence that early diagnosis and early intervention in ASD improve outcome, whether the intervention is mediated by parents20, given as intensive long-term care21 or short-term intervention22. Among the barriers to care for persons with ASD, delayed and low level of detection is a major factor23. For neuro-developmental disorders, screening instruments can be applied at first level by teachers and primary healthcare staff and diagnostic assessment can be done in the second stage. This would lead to an improvement in mental health care for children with ASD23.
Increased prevalence rate has been correlated with improved recognition and detection. In the UK, prevalence of 157/10,000 has been reported by screening for autism spectrum conditions in regular schools and schools for children with special needs24. In a study from Korea, a higher than expected prevalence rate (1.89%) was reported when screening in regular schools was done25. These children had not required additional support or services and were not diagnosed previously. Authors opined that it could be due to scales developed for North American population25. This shows that country-specific scales are required for ASD.
The strength of the present work was that screening instrument was developed in Hindi language. The screening instrument had questions that needed to be read out and not explained; hence, training was not required. Development of scale was done using recognized procedure. Further, it was easy to administer, and took about 15-20 min for administration. The brief screening instrument of four items was also found to have adequate psychometric properties. Sensitivity of four-item screening instrument was 73.49 per cent. It was lesser than 34-item screening instrument (sensitivity 89.16%). A good screening instrument should have higher sensitivity. Hence, 34-item version was considered better while carrying out a proper survey. However, when time is a limitation, CASI Bref (4-item version) can be used (e.g. in camp setting).
One of the major limitations was that only convergent validity was assessed and discriminant validity was not assessed. For making a diagnosis of autism criterion-based approach was used, diagnosis was made as per the DSM IV TR. A diagnostic tool was not used. Another limitation was that the tool was applied on selective cohort of those children whose diagnosis was already known and it was likely to give rise to bias. Ideal approach would be to apply the scale on large number of normal children and then carry out analysis. Finally, usefulness of this scale needs to be evaluated in a large community study.
Financial support & sponsorship: This study was funded by the Department of Health Research/Indian Council of Medical Research, New Delhi, India
Conflicts of Interest: None.
References
- Prevalence and characteristics of autism spectrum disorder among children aged 8 years – Autism and developmental disabilities monitoring network, 11 sites, United States, 2012. MMWR Surveill Summ. 2016;65:1-23.
- [Google Scholar]
- National Institute for the Mentally Handicapped. Indian Scale for Assessment of Autism (ISAA): Test Manual. New Delhi: The National Trust. Ministry of Social Justice & Empowerment, Department of Empowerment of persons with Disabilities. Government of India; Available from: http://arppassociation.org/Downloads/ISAA_Tool.pdf
- [Google Scholar]
- Ministry of Social Justice & Empowerment, Department of Empowerment of persons with Disabilities, Notification. Available from: http://www.disabilityaffairs.gov.in/upload/uploadfiles/files/Autism%20Guidelines-%20Notification_compressed.pdf
- Prevalence of autism spectrum disorders in a semiurban community in South India. Ann Epidemiol. 2016;26:663-5.e8.
- [Google Scholar]
- Prevalence of autism spectrum disorders among children (1-10 years of age) – Findings of a mid-term report from Northwest India. J Postgrad Med. 2015;61:243-6.
- [Google Scholar]
- A meta-analytic study on the effectiveness of comprehensive ABA-based early intervention programs for children with autism spectrum disorders. Res Autism Spectr Disord. 2011;5:60-9.
- [Google Scholar]
- American Psychological Association. Diagnostic and statistical manual of mental disorders (4th ed). Washington DC: American Psychological Association; 2000.
- Sadock BJ, Sadock VA, eds. Kaplan & Sadock's comprehensive textbook of psychiatry. Philadelphia: Lippincott Williams & Wilkins; 2000.
- Thapar A, Pine DS, leckman JF, Scott S, Snowling MJ, Taylor EA, eds. Rutter's child and adolescent psychiatry. Chichester: Wiley Blackwell; 2015.
- Martin A, Volkmar FR, eds. Lewis's child and adolescent psychiatry: A comprehensive textbook. Columbia: Lippincott Williams & Wilkins; 2007.
- The modified checklist for autism in toddlers: An initial study investigating the early detection of autism and pervasive developmental disorders. J Autism Dev Disord. 2001;31:131-44.
- [Google Scholar]
- World Health Organization. The ICD-10 Classification of Mental and Behavioural Disorders: Clinical Descriptions and Diagnostic Guidelines. Geneva: WHO; 1992.
- [Google Scholar]
- Autism screening instrument for educational planning (3rd ed). Austin, Texas: Pro-ed; 2008.
- Autism screening and diagnosis in low resource settings: Challenges and opportunities to enhance research and services worldwide. Autism Res. 2015;8:473-6.
- [Google Scholar]
- Childhood autism rating scale (CARS) and autism behavior checklist (ABC) correspondence and conflicts with DSM-IV criteria in diagnosis of autism. J Autism Dev Disord. 2004;34:703-8.
- [Google Scholar]
- Autistic Behavior Checklist (ABC) and its applications. In: Patel VB, Preedy VR, Martin CR, eds. Comprehensive guide to autism. New York: Springer Science & Business Media; 2014. p. :2787-97.
- [Google Scholar]
- Validation of a brief quantitative measure of autistic traits: Comparison of the social responsiveness scale with the autism diagnostic interview-revised. J Autism Dev Disord. 2003;33:427-33.
- [Google Scholar]
- Overlooked and underserved: “Action signs” for identifying children with unmet mental health needs. Pediatrics. 2011;128:970-9.
- [Google Scholar]
- Parent implemented early intervention for young children with autism spectrum disorder: A systematic review. J Eval Clin Pract. 2007;13:120-9.
- [Google Scholar]
- Long-term outcomes of early intervention in 6-year-old children with autism spectrum disorder. J Am Acad Child Adolesc Psychiatry. 2015;54:580-7.
- [Google Scholar]
- Long-term outcomes of toddlers with autism spectrum disorders exposed to short-term intervention. Pediatrics. 2012;130(Suppl 2):S186-90.
- [Google Scholar]
- Improving access to care for children with mental disorders: A global perspective. Arch Dis Child. 2013;98:323-7.
- [Google Scholar]
- Prevalence of autism-spectrum conditions: UK school-based population study. Br J Psychiatry. 2009;194:500-9.
- [Google Scholar]
- Prevalence of autism spectrum disorders in a total population sample. Am J Psychiatry. 2011;168:904-12.
- [Google Scholar]






