Translate this page into:
Development & evaluation of a training programme to address complex post-COVID psychological needs
For correspondence: Dr Himani Kashyap, Department of Clinical Psychology, National Institute of Mental Health and Neurosciences, Bengaluru 560 029, India e-mail: himani@nimhans.ac.in
-
Received: ,
Accepted: ,
Abstract
Background & objectives
In India, mental health treatment gaps are significant, and related to shortage of trained personnel. Published literature has identified gaps in existing training programmes including - delivering psychological interventions for complex concerns such as intensified post-COVID grief, trauma, suicidality; ongoing mentoring; and culture-sensitive interventions. Despite government initiatives, gaps in treatment and training have been compounded by a surge in psychological distress following COVID-19. This study aimed to develop, implement and evaluate a training programme for psychologists to identify, assess, and treat complex post-COVID psychological concerns.
Methods
The study employed a sequential mixed exploratory research design with tailored programme development (Phase I) and programme delivery with pre-post evaluations of participation, satisfaction, learning and competence using Moore’s framework (Phase II). Psychologists with postgraduate qualifications, engaged in direct client contact were invited through flyers to participate in the free online training programme.
Results
The final programme included ten modules; with knowledge, skills, and application components; comprising synchronous and asynchronous elements. Fifty-three participants enrolled in the programme and 70 per cent completed the course. Pre-post evaluations indicated high satisfaction (93.54% rated as met/exceeded expectations); improvements in competence (pre training mode = 3; post-training mode = 4); and average to above average learning scores (mean scores ≥3 on 7 out of 9 module quizzes). Participant feedback revealed that the focus on complex concerns, practical learning through interactive sessions and role play recordings, and case-based supervision were helpful.
Interpretation & conclusions
The programme focused on training gaps identified through a needs assessment survey. It was received well in terms of participation, satisfaction, content, accessibility and learning. The indigenous and skill-focused training has implications to contribute to future mental health preparedness and scope for large-scale deployment.
Keywords
COVID
mental health
digitised training programme
disaster preparedness
grief and trauma
human resource development
psychologist training
Mental disorders represent 13 per cent of the global burden of disease1 and in India, affect over 197 million individuals2. Treatment gaps of up to 84.5 per cent persist3, despite the Indian Government’s implementation of mental health programmes, including grassroots training of personnel4. With the advent of COVID-19, mental health concerns peaked by 20 per cent in India5. Across the world, lockdowns, disrupted routines, quarantine mandates, travel restrictions and insufficient information affected psychological well-being, and contributed to symptoms like post-traumatic stress, depression, anger, anxiety, sleep difficulties, suicidality, and anticipatory grief6,7.
Despite a research spotlight on COVID-19, relatively limited inquiry has been directed towards the post-pandemic period. Experts predicted a ‘tsunami of psychiatric illnesses’ in the aftermath of COVID-19, especially for vulnerable populations8,9 and complex concerns such as suicidality9, complicated grief and suggestion of a ‘collective trauma’10. Confirming these predictions, significant increases in a range of psychiatric symptoms have been reported in the post-pandemic phase11 particularly related to trauma, suicidality, and complicated grief10. These have been attributed to the large-scale losses, reduced social support and long periods of isolation, and absence of mourning rituals12. The persistence of physical symptoms in long COVID has been linked to grief regarding loss of physical health13. The nature of the pandemic is distinct because healthcare professionals faced considerable challenges themselves during the pandemic, while addressing concerns of clients. Upto 60 per cent of them were affected by symptoms of anxiety, depression, and insomnia during the pandemic, with persistence of symptoms predicted for several years to come9. If the mental health of mental health professionals themselves is not adequately addressed, they may struggle to deliver effective services in the post-pandemic period7.
In India, the increased burden on tertiary mental health systems during the pandemic is indicated by roughly doubled demand for psychotherapy sessions14. Government initiatives show commensurate step-up during COVID, e.g., Ministry of Health and Family Welfare psychosocial toll-free helpline, release of audio-visual awareness resources and guidelines15 and Tele - MANAS, the digital arm of the District Mental Health Programme16. However, mental health services were quickly overwhelmed during COVID-1917. Some programmes attempted to meet the increased demand for trained personnel during COVID-19, such as training for telephone-based psychological support18, for strengthening knowledge and skills of community health workers19 and for specific concerns such as depression, dementia, anxiety and substance abuse20. These were in addition to previously existing programmes such as training for Accredited Social Health Activists (ASHAs)21, non-specialist health workers and lay counsellors22. However, while mental health concerns persisted in the post-pandemic period, many helplines and training programmes could not be sustained beyond the acute phase.
A systematic review of training programmes for community-level workers in India revealed significant gaps in specialised training for handling severe concerns and supervision, and underscored involvement of various stakeholders to attend to the design, delivery, supervision, evaluation, and considerations for sustainability and scalability23. Previous training programmes in the COVID context reported training needs regarding identification of high distress concerns such as anxiety, suicidality, depression and behavioural addiction; and referral processes18. Educating non-licensed personnel like counsellors, community mental health workers, and youth development professionals to administer low-intensity interventions has proven effective to broaden mental health services, increase accessibility and initiate prevention strategies24. However, a critical gap in existing programmes is the need for training and ongoing supervision in advanced psychotherapeutic interventions for complex concerns which are not covered in basic training23, and have intensified in the post-COVID period. Further, it is likely that the above concerns do not exist in isolation among individuals, necessitating interventions at the intersection of these concerns. There is also a requirement of culture-sensitive therapeutic strategies, as direct transfer of Western philosophies may not be applicable25. Addressing the above gaps will help mental health systems to adopt a ‘pandemic lens’ for the future. The current study attempts to bridge this gap through developing, implementing and evaluating a training and supervision programme for psychologists, with a special focus on the complex nature of post-COVID issues in India.
Materials & Methods
This study was conducted by the departments of Clinical Psychology and Mental Health Education, National Institute of Mental Health and Neurosciences (NIMHANS), Bengaluru between June 2023 and February 2024. This study was carried out in accordance with the guidelines of the Institute Ethics Committee (Behaviour Sciences Division). The participants were not required to pay for the training. Participants, who requested further training/supervision beyond the programme, were offered appropriate options and resources. All participants were provided contact resources in the event of personal psychological distress. The study employed a sequential exploratory mixed research design: Phase I included identification of training needs and programme development based on the Steps for Quality Intervention Development (6SQuID)26-defining and understanding training needs, clarifying how training will be delivered, testing the programme, and rigorous evaluation. Phase II comprised programme delivery and evaluation of participation, satisfaction, learning and competence27.
Phase I: Programme development:
Defining and understanding training needs
Training needs were identified through three gateways: literature review of existing training programmes and identification of training gaps in India; consultation with subject experts and content designers; and needs-assessment survey of psychologists.
The needs assessment survey sent via online forms to 121 psychologists meeting criteria (described in Phase II and Fig. 1) sought information on knowledge about COVID, previous training, client practice and personal experiences in the post-COVID period. The responses of the survey have been mentioned in the results section.
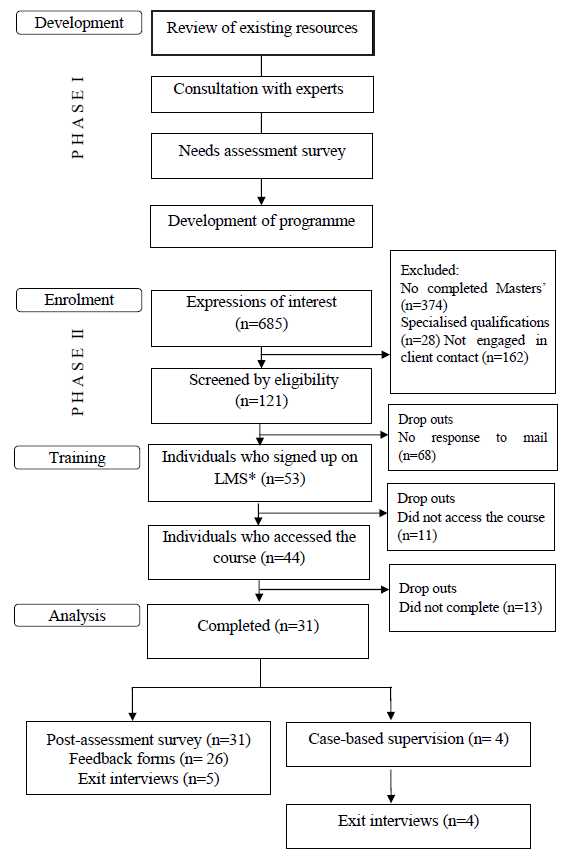
- Prisma flow chart explaining steps of allocation of participants to the training programme. *LMS, learning management system.
Phase II: Programme delivery
Sample
The sample included individuals with a postgraduate degree in psychology, engaged in direct client contact. Individuals without a postgraduate qualification, unemployed or employed in research /academic positions were excluded. A purposive sampling technique was utilised, and participants were invited through flyers circulated online to attend the free training conducted by a tertiary institute.
Study design
A single-group mixed design with quantitative pre-post assessment and qualitative feedback was used.
Tools
Besides the needs-assessment survey described in the methods section, the study developed five-point ratings of participants’ confidence (in handling post-COVID concerns) and competence (on a list of skills such as grief counselling, crisis intervention, psychoeducation, suicide risk assessment), administered pre and post-training assessment.
A semi-structured exit interview schedule was developed containing the following sections: helpful and unhelpful elements of the programme content; access and use of materials on LMS (Learning Management System); general feedback on application of learnt skills in clinical practice, online live sessions, practice quizzes; suggestions for further modifications and case-based discussions (Supplementary Table).
A feedback form was developed seeking five-point ratings on the helpfulness of the components of the programme namely, knowledge, skills training and practice/application.
As shown in figure 1, 685 expressions of interest were received via online flyers, with 121 meeting the inclusion criteria who were then invited to participate. Of these, 53 participants enrolled on LMS, completed the pre-assessment survey and received login credentials. 31 participants completed the modules and post-assessment survey; five volunteered for an exit interview, and the remaining 26 completed the feedback form. Among the completers, 14 expressed interests in the weekly case-based supervision; and four completed all supervision sessions and online exit interviews with the first two authors. Certificates were issued to all course completers.
Data analysis
Quantitative analysis comprised descriptive statistics such as mean, mode, standard deviation, frequency and percentages to examine sample characteristics. The effectiveness of the training programme was assessed on Moore’s evaluation framework for continuing medical education27, employing the first four levels from the framework, as follows:
-
(i)
Level 1: Participation refers to the number of professionals engaged in the training program.
-
(ii)
Level 2: Satisfaction reflects how well the training programme met participants’ expectations regarding its setting and delivery.
-
(iii)
Level 3: Learning is assessed by participants’ ability to demonstrate their understanding of the knowledge intended by the training programme
-
(iv)
Level 4: Competence is evaluated based on participants’ ability to perform tasks in an educational context as intended by the training programme, including aspects of perceived self-efficacy and self-confidence.
Qualitative analysis was carried out for exit interviews through the steps defined by Braun et al28: familiarising oneself with the data, generating initial codes, seeking themes, defining and naming themes, and reporting.
Results
As evidenced from table I, participants were between 22 to 51 yr age (mean=28.2; SD=6.2). A majority were female, more than half specialised in clinical psychology, and were employed in private organisations. Most participants provided offline sessions, and a majority had client contact up to two years.
| Sociodemographic characteristics | Mean/ n | S.D.^/% | |
|---|---|---|---|
| Age | 28.2 | 6.2 | |
| Gender |
Female Male |
38 15 |
71.6 28.3 |
| Specialization degree |
Clinical psychology Psychology Applied psychology Counselling psychology Rehabilitation psychology Industrial psychology |
28 12 7 4 1 1 |
52.8 22.6 13.2 7.5 1.8 1.8 |
| Nature of organisation |
Private Government NGOs |
37 10 6 |
69.8 18.8 11.3 |
| Mode of work |
Offline Online Hybrid |
37 8 8 |
69.8 15 15 |
| Work setting |
Clinical Educational Corporate |
39 18 11 |
73.5 33.9 20.7 |
| Job experience |
Fresher-2 yr 3-6 yr 10+ yr |
37 14 2 |
69.8 26.4 3.7 |
| Nature of involvement in client care |
Paid employment Volunteering Internship |
48 3 2 |
90.5 5.6 3.7 |
| Number of client consultations per wk |
Less than 10 h 10-24 h 24-48 h More than 48 h |
24 13 12 4 |
45.2 24.5 22.6 7.5 |
| Number of clients seen with COVID concerns in the last 6 months |
Less than 10 11-30 31-60 More than 60 Not applicable |
20 17 1 3 12 |
37.7 32 1.8 5.6 22.6 |
n, frequency; S.D. ^ , standard deviation; %, percentage
On the needs assessment survey, of the 48 responses received, 26 individuals (54.16%) rated their knowledge on post-COVID mental health issues as average or below average (indicated by a score ≤ 3 out of 5). Participants reported that stressors most frequently encountered with clients in the post-COVID era include loneliness and death of a loved one (n=46; 95.8%), financial loss (n=41; 85.4%), employment loss (n=40; 83.3%) and post-COVID health complications (n=35; 72.91%) with concerns like anxiety (n=48; 100%), depression (n=47; 97.9%) and loneliness (n=41; 85.4%) intensified in the post-COVID period. Addiction to technology (n=25; 52.1%), family conflicts (n=25; 52.1%), grief (n=24; 50%), depression (n=19; 39.6%) and loneliness (n=19; 39.6%) were reported as the most challenging to address. Participants rated their training as average or below average (indicated by a score ≤ 3) in the area of problematic technology use (n=41; 85.4%), trauma and grief (n=40;83.33%) and suicidality (n=36; 75%). Additionally, a majority (n=37; 77.1%) reported lack of access to sufficient resources to help clients and aid their practice. All participants reported themselves experiencing one or more stressors during the pandemic, namely, challenges while handling clients (n=27, 56.3%), risk of becoming infected (n=24, 50%), finances (n=21, 43.8%), switching to online consultation (n=19, 37.6%), risk of passing the infection on to others (n=17, 35.4%), increased workload (n=13, 27.1%), loss of a loved one (n=11, 22.9%), employment loss (n=5, 10.4%) and reduced self-esteem (n=1, 2.1%). Techniques like self-care (n=40, 83.3%) and peer discussions (n=36, 75%) were reported as helpful to assist their clinical practice. Hence the training program was tailor-made to address the needs identified by participants themselves.
The gaps in literature and the needs identified in the survey were discussed with subject experts, i.e., authors and resource persons who identified the important themes to be addressed in the training, and sub-themes of the same, to be developed into a course curriculum.
Figure 2 shows the key data extracted to understand training needs and clarify training development and delivery.
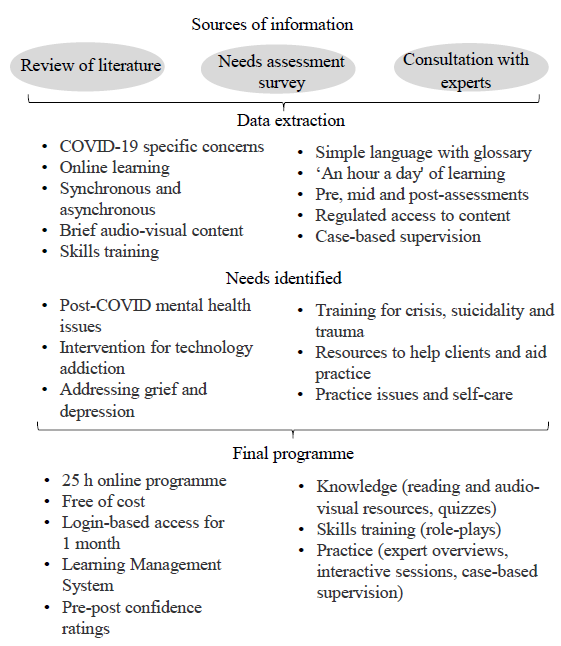
- Process of identification of training needs and development of training programme.
Developing training content and structure
Content of the modules
The programme content (Table II) was curated by the authors, based on the needs identified from the survey, starting with post-COVID mental health issues and stressors (Module 2). The physical health module addressed long COVID, while the mental health module included long-term impacts of psychological stressors (changes in academic, work and social functioning), quarantine, coping with loss, and cognitive issues, particularly for vulnerable populations. This knowledge was crucial for interventions and psychoeducation (Module 5). Modules 4 and 8 covered intake, assessments and negative effects, which although part of basic training, were addressed for COVID concerns. Shortfalls identified in the needs assessment survey in areas such as technology addiction, grief, trauma, suicidality, and were included (Modules 3, 7 and 9), along with practice issues such as ethics, tele psychotherapy and self-care for psychologists (Module 10).
| Module 1: Introduction to the programme | |||||
|---|---|---|---|---|---|
| Overview and context of the programme, introduction to the project team and a guide to use LMS | |||||
| Module 2: Impact of COVID-19 | |||||
| EO | PT | RP | RM | OLS | |
| Long-term physical health implications | ü | ü | |||
| Mental health and socio-occupational implications | ü | ü | |||
| Concerns in vulnerable populations in India | ü | ||||
| Psychiatric and psychological conditions in the pandemic and post-pandemic period | ü | ü | |||
| Cognitive concerns associated with Long COVID-19 | ü | ü | |||
| Module 3: COVID-19 and technology | |||||
| EO | PT | RP | RM | OLS | |
| Technology use related to COVID-19 | ü | ü | |||
| Internet, gaming, and social networking sites: addiction and overuse | ü | ü | |||
| Infodemic during the pandemic | ü | ||||
| Module 4: Initial interview | |||||
| EO | PT | RP | RM | OLS | |
| Case history taking | ü | ||||
| Micro skills | ü | ||||
| Brief assessments | ü | ||||
| Module 5: Psychoeducation | |||||
| EO | PT | RP | RM | OLS | |
| Psychoeducation for COVID-related mental health concerns | ü | ü | |||
| Module 6: Supportive intervention | |||||
| EO | PT | RP | RM | OLS | |
| Purpose, strategies, and techniques | ü | ü | |||
| Module 7: Loss and grief | |||||
| EO | PT | RP | RM | OLS | |
| Understanding loss and grief | ü | ||||
| Addressing grief during the pandemic | ü | ||||
| Grief and loss: An overview | ü | ||||
| Coping with grief | ü | ü | |||
| Module 8: Negative affect | |||||
| EO | PT | RP | RM | OLS | |
| Negative affect: An overview | ü | ||||
| Brief interventions for depression and related concerns | ü | ü | |||
| Brief interventions anxiety and related concerns | ü | ü | |||
| Module 9: Crisis and trauma intervention | |||||
| EO | PT | RP | RM | OLS | |
| Crisis and trauma intervention | ü | ü | |||
| Crisis intervention and suicidality | ü | ü | ü | ||
| Trauma informed care | ü | ü | |||
| Module 10: Practice issues in psychological care | |||||
| EO | PT | RP | RM | OLS | |
| Tele psychotherapy | ü | ü | |||
| Ethics in psychotherapy | ü | ü | ü | ||
| Challenges and self-care for psychologists | ü | ü | |||
Note: The table represents the modules and sub-modules of the training programme along with the mode of delivery. EO, expert overview; PT, presentations; RP, role play; RM, reading material; OLS, online live session
Structure and format
The training material comprised knowledge, skills training and practice/application in each of the ten modules. Knowledge component included 10–15 min video presentations, reading materials (comprising of research articles and information sheets, categorised as recommended and additional resources), and quizzes (Table II). Skills training involved role-play recordings of practical skills for interviews and interventions, highlighting key takeaways and post-hoc session discussions. The practice/application section featured expert overviews and weekly interactive sessions with experts (clinical psychologists with over 15 yr of experience).
Subject experts structured the programme to progress from basic skills (interviewing, assessment) to advanced skills (brief interventions), catering to participants with varying clinical experience. Each module included reading materials, expert overviews, presentations, interviews, role plays, and module quizzes for evaluation. Participants could progress to the next module after completing the quiz of the subsequent module.
Ethics, practice issues and supervision
Optional group supervision was offered for four weekly sessions, with participants each presenting one case. Offered by the second author (clinical psychologist with over 15 yr of experience), the supervision aimed at risk assessment, intervention optimization, and identification of referral needs. The objective was to support participants in maintaining ethical and evidence-based practice. Ethical considerations and practice issues were identified by subject experts as needing elaboration in the training content.
Culture-sensitivity
Culture-sensitivity was maintained throughout with a focus on the Indian context (e.g., impact of COVID, ethical considerations, and tele-psychotherapy). Reading materials incorporated Indian research while pre-recorded expert overviews and role plays addressed cultural nuances unique to the Indian context such as large-scale losses without mourning rituals; socio-cultural factors in technology addiction like reduced social support, long periods of isolation and the infodemic; and systemic issues like overwhelmed mental health services and reduced sustainability of services for crises responses.
Digitization of the programme
The course was hosted on the institute’s LMS and offered free of charge for easy access, especially for remote participants. A landing page and user manual guided navigation, while an intro session addressed platform concerns and boosted engagement. Videos and reading materials were embedded on the LMS. The programme spanned one month (25 h total), with approximately one hour of learning per weekday.
Figure 3 shows the effectiveness of the training programme as assessed on the evaluation framework for continuing medical education27.
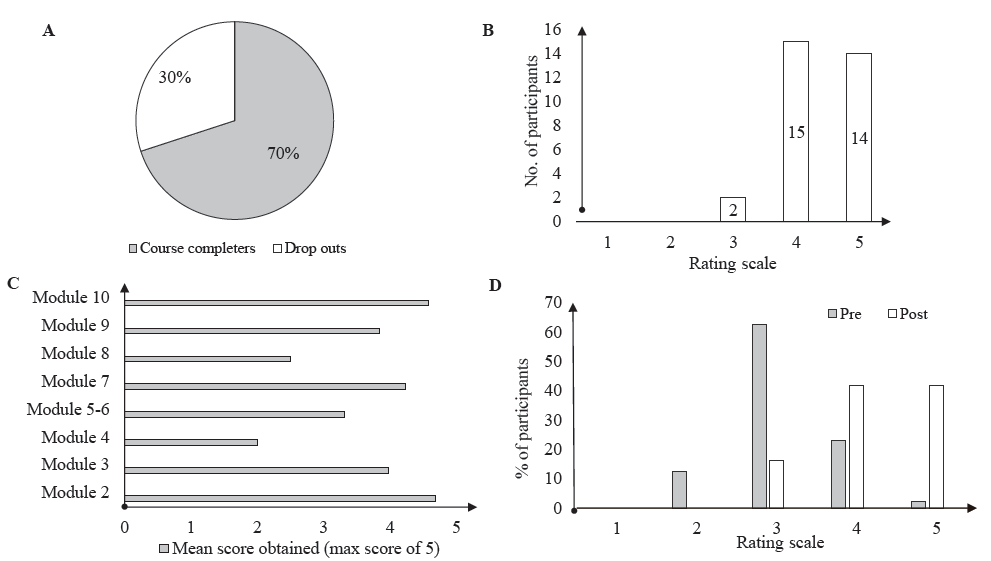
- The figure shows the evaluation of the training programme based on the levels of Moore’s evaluation framework (2015) as follows: (A) Participation, (B) satisfaction (1-very dissatisfied, 2-dissatisfied, 3-neutral, 4-satisfied, 5-very satisfied), (C) learning scores on each module (Module 2-impact of COVID, Module 3 - COVID and technology, Module 4 – initial interview, Module 5 and 6 – psychoeducation and supportive intervention, Module 7 – loss and grief, Module 8 – negative affect, Module 9 – crisis and trauma intervention, Module 10 – practice issues in psychological care), and (D) self-rated competence (1-very poor, 2-poor, 3-fair, 4-good, 5-very good).
Participation
This was measured by the number of participants who enrolled, attendance rates for case-based discussions, and number who completed all of the modules. Fifty-three participants enrolled for the programme, 44 accessed the course and 31 of them (70%) completed the modules (Fig. 3).
Satisfaction
Feedback forms and exit interviews obtained ratings of the degree to which expectations of participants from the course were met. On a 5-point Likert scale (5=very satisfied, 4=satisfied, 3=neutral, 2=dissatisfied, 1=very dissatisfied), 29 out of 31 participants (93.54%) rated the programme as meeting expectations (Fig. 3). In the exit interviews and feedback survey, the broad range of content covered and practical learning were reported helpful; difficulties reported included technical glitches and short duration (course duration was extended to accommodate these). Participants suggested future modifications - need for more intensive and longer specialised training, with more interactive elements. Participants who attended the case-based discussion sessions reported validation from the group, applicability of skills and exposure to a wide range of client presentations and perspectives as helpful.
Learning
Module quizzes assessed participants’ learning and mean scores in seven out of nine of the modules indicated average to above average performance (indicated by a score of ≥3 on 5) (Fig. 3). Quiz questions were curated by subject experts from module resources and administered via Google Forms, with answer keys provided after completion. Each quiz consisted of five items, allowing a maximum score of 5 (1 point per correct response). The average score for all participants was calculated for each module.
Competence
Confidence ratings for problems and interventions covered in the course were obtained and showed modal increase from average to above average (pre training mode = 3; post-training mode = 4) (Fig. 3).
Discussion
The study aimed to develop, implement and evaluate a training and supervision programme for psychologists with a special focus on the complex nature of post-COVID issues in India. Significant gaps have been identified in existing training programmes relating to complexity of psychological concerns, culture-sensitive interventions, and supervision23. The current study attempted to bridge these gaps, by training psychologists to identify and address psychological needs that have intensified post-COVID. This was done by defining and understanding training needs from the literature and various stakeholders, developing engaging and skill-focused training content to be hosted, delivered and evaluated through the online learning management system.
Triangulation of data from literature review, consultation with experts and needs assessment survey formed the phase I results and informed the content of the modules. Training content ranged from basic interviewing, identification of referral needs, and interventions for concerns like trauma, suicidality and grief, in a culture sensitive manner and self-care for professionals which were identified in existing literature7,8,18,23,25 and the needs assessment survey of phase I. The focus of training and difficulty level were also maintained through careful selection of a homogenous group of participants with basic training in psychology, and experience with client contact, managed through login-based access to eligible participants.
In phase II, the programme was well-received as evidenced by participation, satisfaction, competence ratings and learning scores27. Participants provided positive feedback about the relevance and easy applicability of the content, and progressive difficulty levels. Online mode of training has been highlighted in the literature as a convenient and a time-saving method which increases accessibility, availability and affordability among participants18,29. Some challenges were highlighted in online training programmes of the recent past, such as adoption of a completely asynchronous model of teaching, use of complex language, time constraints and lack of video-based interactive sessions29. As highlighted in other studies21 this programme attempted to overcome these challenges by balancing synchronous (interactive live sessions and case-based supervision) and asynchronous (recorded audio-visual content and reading materials in simple language) aspects of learning. This balance ensured that participants could complete the asynchronous content at their own pace and attend scheduled synchronous sessions.Interactive sessions were highlighted by our participants as a space for practical learning and greater connectivity with one another.
Satisfaction was reported on fulfilment of expectations. High satisfaction scores in our study could be attributed to curation of the training programme based on the needs-assessment from participants themselves29. Relatedly, there was an increase from pre-to post training ratings of competence, since the programme targeted areas where training was lacking. On feedback, participants suggested training in more intensive psychotherapeutic interventions. Learning was demonstrated in the form of average to above-average scores in all modules. Over 95 per cent of our participants reported applying skills learnt from the programme into their practice – this reflects the utility of the knowledge-skills-practice components of the programme.
The structure and format of the programme was intended to ensure maximum trainee engagement in several ways: Firstly, the videos were limited to a duration of around ten min. This duration has been recommended to reduce extraneous cognitive load and aid in schema building, contributing to greater student engagement and learning as compared to longer videos30-32. Practice quizzes are known to function as an incentive for active learning and preparatory reading and are recommended to improve student activity and persistence in online training programmes33. This feature of the programme bridges a gap identified in recent studies18,23. Role plays and case-based supervision emphasised practical learning and application, which are integral to training and a quality assurance tool in treatment delivery34.
Participant motivation was managed through regular email contact, availability for troubleshooting, restrictions on content downloading to minimise procrastination, module quizzes, interactive sessions, and certificates for programme completion. Recommendations from a recent systematic review23 indicated a need for specialised training and supportive supervision to help professionals deliver intervention in the context of the pandemic and beyond. In adherence to this, the training programme content spanned across various mental health concerns covering topics like grief, crisis and trauma which had received little attention in existing programmes. This programme also aimed to offer broad basic training in interviewing, micro-skills and low-intensity interventions, unlike the selective focus of some other programmes20. Additionally, the case-based supervision in this programme was reported by participants as helpful, and has been highlighted as an important component23. Only a few existing programmes had peer supervision or mentoring based on trainee needs29.
A key strength of the programme was its wide reach, with participants from across India, enabled by the digitization of content for sustainability. This was among the few programmes developed specifically for the post-pandemic context. Unlike other shorter programmes for training frontline volunteers in providing telephonic support regarding concerns in the acute phase of COVID-1918, this programme was developed for persisting, complex pandemic-related concerns, for longer-term therapies conducted online, offline or hybrid.
Limitations
A significant limitation of the programme was attrition at every stage of the study. The four-month gap between needs-assessment and programme initiation (to facilitate content development), may have contributed to dropout due to participants’ changed circumstances (e.g., some participants provided a workplace email address, but changed jobs in the meantime). While the programme was offered free-of-cost, free programmes have interestingly been associated with lower persistence and motivation, compared to a paid or a refund programme35. Efforts to increase engagement through multiple reminders via email, invitations to interactive sessions, and completion incentives through issue of certificates were made; perhaps communication through modes like telephone or instant messaging may have elicited better response than e-mails29. More flexible supervision options may have increased participation. Due to a lack of data from similar programmes in India and no specific reasons for dropout due to a lack of response, it was difficult to assess whether this rate is typical in the selected study setting.
The study did not assess the long-term application or maintenance of skills in real-world settings, and this could be explored in future research. Pre- and post-test knowledge scores would also help measure learning gains. Moving forward, the programme could be periodically reassessed and adapted based on needs. The preliminary nature of the study and the small sample made it difficult to control for selection biases, study power, and hence limits the generalizability of findings.
Overall, the training programme attempted to bridge treatment gaps in the post-COVID period through training in culture-sensitive, brief, skill-focused interventions for complex psychological concerns, on an easily accessible online platform. The final programme included ten modules (focused on complex concerns such as grief, trauma, suicidality), with knowledge, skills, and application components, comprising synchronous and asynchronous elements. This study is a preliminary step and is suitable for large-scale deployment given its online and self-sustainable nature. Content developed for the programme, along with feedback from completers, can be adapted to other mental health training programmes, and contribute to mental health preparedness to meet large-scale intensive needs (e.g., future pandemics, disasters).
Acknowledgment
Authors acknowledge Dr. Jyothsna Chandur, Ms. Malika Verma, and Ms. Vasundhara Kulkarni for inputs to conceptualization; and Dr(s) Geetha Desai, Harish Thippeswamy, Ms. Akanksha Verma, Ananta Khare, Ashwini Tadpatrikar, Harikrupa Sridhar, Himali Madavi, Hitankshi Trivedi, Jemimah Johnson, Merlyn Sargunaraj, Preeti Kodancha, Shweta Sunil, Soumya Sardana, Srijita Gupta, Tanisha Agarwal, Mr. Rojo George, and Dr. Mahalaxmi for their contribution to the training programme.
Financial support & sponsorship
The study received funding from Indian Council of Medical Research (No. NCD/130/2022-23).
Conflicts of Interest
None.
Use of Artificial Intelligence (AI)-Assisted Technology for manuscript preparation
The authors confirm that there was no use of AI-assisted technology for assisting in the writing of the manuscript and no images were manipulated using AI.
References
- Institutional Repository for Infromation Sharing. The global burden of disease: 2004 update. Available from: https://iris.who.int/handle/10665/43942, accessed on March 21, 2024.
- The burden of mental disorders across the states of India: The global burden of disease study 1990–2017. Lancet Psychiatry. 2020;7:148-61.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- The national mental health survey of India (2016): Prevalence, socio-demographic correlates and treatment gap of mental morbidity. Int J Soc Psychiatry. 2020;66:361-72.
- [CrossRef] [PubMed] [Google Scholar]
- 2020-21 Annual Report. Available from: mohfw.nic.in, accessed on April 20, 2024.
- COVID 19 and its mental health consequences. J Ment Health. 2020;30:1-2.
- [CrossRef] [PubMed] [Google Scholar]
- The psychological impact of quarantine and how to reduce it: Rapid review of the evidence. Lancet. 2020;395:912-20.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Mental health in the post-COVID-19 era: Challenges and the way forward. Gen Psychiatr. 2021;34:e100424.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Mental health implications of COVID-19 pandemic and its response in India. Int J Soc Psychiatry. 2021;67:587-600.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Post COVID-19 pandemic mental health challenges. Asian J Psychiatr. 2020;53:102430.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- The COVID-19 pandemic as a traumatic event and the associated psychological impact on families - A systematic review. J Affect Disord. 2022;319:27-39.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Researching into Chinese university students’ mental health in the post-pandemic era - problems and causes. Front Psychol. 2024;15:1393603.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Addressing grief and bereavement in COVID-19 pandemic. Illness Crisis and Loss. 2024;32:492-503.
- [CrossRef] [Google Scholar]
- A journey through grief: experiences of loss among patients with long COVID. J Patient Exp. 2024;11:23743735241272267.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Institute of National Importance Bengaluru. Annual report 2020-21. Bengaluru, 2021. Available from: https://nimhans.ac.in/wp-content/uploads/2022/09/NIMHANS_AR_2020-21_English.pdf, accessed on April 20, 2024.
- Ministry of Health & Family Welfare [homepage on Internet]. Government of India [update 2025 January 30]. Available from: https://www.mohfw.gov.in/, accessed on February 22, 2024.
- National tele-mental health program in India: A step towards mental health care for all? Indian J Psychiatry. 2022;64:117-9.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Govt. helpline receives 92,000 calls on child abuse and violence in 11 days. The Hindu [Internet]. 2020 Apr 8. Available from: https://www.thehindu.com/news/national/coronavirus-lockdown-govt-helpline-receives-92000-calls-on-child-abuse-and-violence-in-11-days/article31287468.ece, accessed on February 22, 2024.
- A mental health training program for community health workers in India: Impact on knowledge and attitudes. Int J Ment Health Syst. 2011;5:17.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Training Community health workers in geriatric mental health: Process of manual development and pilot testing findings. Asian J Psychiatr. 2018;38:12-5.
- [CrossRef] [PubMed] [Google Scholar]
- Impact of technology driven mental health task-shifting for accredited social health activists (ASHAs): Results from a randomised controlled trial of two methods of training. Community Ment Health J. 2023;59:175-84.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Tele-mentoring and monitoring of the national mental health program: A bird’s-eye view of initiatives from India. Available from: https://telehealthandmedicinetoday.com/index.php/journal/article/view/262, accessed on April 16, 2024.
- Intervention-based mental health training for community level workers in India - A systematic review. J Family Med Prim Care. 2022;11:1237-43.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Three steps to flatten the mental health need curve amid the COVID-19 pandemic. Depress Anxiety. 2020;37:405-6.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Counseling in developing countries: Turkey and India as examples. J Ment Health Couns. 2005;27:149-60.
- [Google Scholar]
- Six steps in quality intervention development (6SQuID) J Epidemiol Community Health. 2016;70:520-5.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Process evaluation of complex interventions: Medical research council guidance. BMJ. 2015;350:h1258.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Effectiveness of NIMHANS ECHO blended tele-mentoring model on integrated mental health and addiction for counsellors in rural and underserved districts of Chhattisgarh, India. Asian J Psychiatr. 2018;36:123-7.
- [CrossRef] [PubMed] [Google Scholar]
- Short videos, or long videos? A study on the ideal video length in online learning. IEEE Conference Publication. In: IEEE Xplore. International Conference on Information Technology (ICIT). Amman: Jordan; 2021. p. :366-70.
- [Google Scholar]
- The impact of short videos on student performance in an online-flipped college engineering course. Humanit Soc Sci Commun. 2022;9:327.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Active learning through online quizzes: better learning and less (busy) work. J Geo Higher Edu. 2017;41:24-38.
- [CrossRef] [Google Scholar]
- The contribution of therapist effects to patient dropout and deterioration in the psychological therapies. Clin Psychol Psychother. 2017;24:575-88.
- [CrossRef] [PubMed] [Google Scholar]
- Incentives for learning: How free offers help or hinder motivation. Int J Res Marketing. 2022;39:380-95.
- [CrossRef] [Google Scholar]






