Translate this page into:
Cutaneous & subcutaneous phaeohyphomycosis by Lasiodiplodia theobromae
*For correspondence: rungmei@gmail.com
-
Received: ,
This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
This article was originally published by Wolters Kluwer - Medknow and was migrated to Scientific Scholar after the change of Publisher.
A 40 yr old male† on triple immunosuppression one year after renal transplantation, presented to the Microbiology department of Sanjay Gandhi Postgraduate Institute of Medical Sciences, Lucknow, India, with multiple, violaceous nodules with discharging sinuses over the inter-scapular area, measuring 12 × 10 cm (Figure A) in October 2018. Aspirated pus showed pigmented, septate, branching fungal hyphae, suggestive of phaeohyphomycosis on KOH wet mount (Figure B) and Gram stain (Figure C). Culture grew a black mycelial fungus (Figure D – obverse and Figure E – reverse). The isolate was confirmed as Lasiodiplodia theobromae by sequencing.
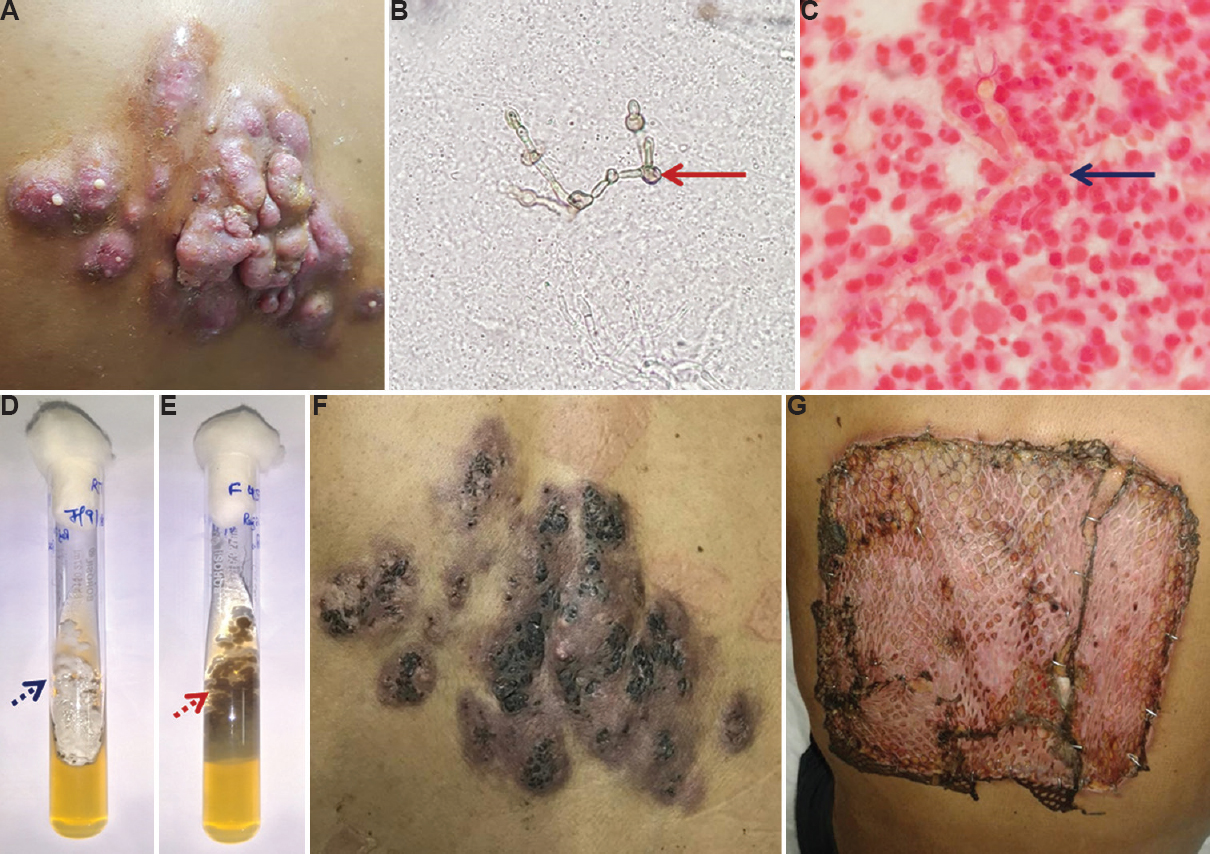
- (A) Multiple, violaceous nodules with discharging sinuses over the inter-scapular area (at presentation). (B) KOH wet mount (×40) showing pigmented, septate, branching fungal hyphae with hyphal swellings (solid red arrow). (C) Gram stain (×100) showing septate, branching fungal hyphae with hyphal swellings (solid blue arrow). (D) Obverse of tube culture on Sabouraud dextrose agar showing black mycelial fungus (dotted blue arrow). (E) Reverse of the Sabouraud dextrose agar tube showing black mycelial fungus (dotted red arrow). (F) Lesion after three months of itraconazole therapy. (G) Skin grafting on the third post-operative day.
The patient was treated with itraconazole (200 mg B.D. P.O.) for 12 wk (Figure F), followed by wide excision and skin grafting (Figure G). Post-operatively, tablet itraconazole was continued for 12 wk. On follow up, after six months grafted skin was healthy.
Conflicts of Interest: None.





