Translate this page into:
Contribution of medical colleges to tuberculosis control in India under the Revised National Tuberculosis Control Programme (RNTCP): Lessons learnt & challenges ahead
Reprint requests: Dr S.K. Sharma, Former Chairman, National Task Force for involvement of Medical Colleges in the Revised National Tuberculosis Control Programme, Goverment of India Professor & Head, Department of Medicine, All India Institute of Medical Sciences, New Delhi 110 029, India e-mail: sksharma.aiims@gmail.com
-
Received: ,
This is an open-access article distributed under the terms of the Creative Commons Attribution-Noncommercial-Share Alike 3.0 Unported, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Medical college faculty, who are academicians are seldom directly involved in the implementation of national public health programmes. More than a decade ago for the first time in the global history of tuberculosis (TB) control, medical colleges of India were involved in the Revised National TB Control Programme (RNTCP) of Government of India (GOI). This report documents the unique and extraordinary course of events that led to the involvement of medical colleges in the RNTCP of GOI. It also reports the contributions made by the medical colleges to TB control in India. For more than a decade, medical colleges have been providing diagnostic services (Designated Microscopy Centres), treatment [Directly Observed Treatment (DOT) Centres] referral for treatment, recording and reporting data, carrying out advocacy for RNTCP and conducting operational research relevant to RNTCP. Medical colleges are contributing to diagnosis and treatment of human immunodeficiency virus (HIV)-TB co-infection and development of laboratory infrastructure for early diagnosis of multidrug-resistant and/or extensively drug-resistant TB (M/XDR-TB) and DOTS-Plus sites for treatment of MDR-TB cases. Overall, at a national level, medical colleges have contributed to 25 per cent of TB suspects referred for diagnosis; 23 per cent of ‘new smear-positives’ diagnosed; 7 per cent of DOT provision within medical college; and 86 per cent treatment success rate among new smear-positive patients. As the Programme widens its scope, future challenges include sustenance of this contribution and facilitating universal access to quality TB care; greater involvement in operational research relevant to the Programme needs; and better co-ordination mechanisms between district, state, zonal and national level to encourage their involvement.
Keywords
Control
India
medical colleges
MDR-TB
XDR-TB
Revised National Tuberculosis Control Programme (RNTCP)
tuberculosis
Introduction
Tuberculosis (TB) is a dreadful infectious disease with devastating social and economic consequences. India is one of the high TB burden countries. More adults die from TB than from any other infectious disease in India1. With its commitment to reduce the morbidity, mortality and disability due to TB and eliminate it as a public health problem, the Government of India (GOI), after piloting the DOTS strategy successfully from 1993-1996, had initiated the Revised National Tuberculosis Control Programme (RNTCP) adopting the DOTS strategy in 1997. Subsequently, the Programme had expanded to cover the entire population of the country in March 20062. In India, TB patients are managed by several healthcare providers involving diverse sectors from the government, non-governmental organizations (NGOs) and the private and corporate sectors. Effective control of TB will be possible if all these sectors join together and work towards a common goal.
A substantial proportion of patients with TB are managed at medical colleges across the country. From the TB control point of view, medical colleges, in both the government and private sectors are recognized to occupy a key position with a unique potential for involvement with the RNTCP. To widen access and improving the quality of TB services, involvement of medical colleges and their hospitals is of paramount importance. Being tertiary care medical centres, large numbers of patients seek care from the medical colleges. In addition, the role of medical college faculty in TB control as key opinion leaders and role models for practicing physicians and as teachers imparting knowledge, skills and shaping the attitude of medical students cannot be underestimated. There is a pressing need for all medical colleges to advocate and practice DOTS strategy which provides the best opportunity for cure of TB patients. In addition, medical colleges have the diagnostic facilities for extra-pulmonary TB (EPTB), human immunodeficiency virus (HIV)-TB co-infection, multidrug-resistant TB and extensively drug-resistant TB (M/XDR-TB). Recognizing the potential of involving medical colleges in TB control a decade ago, the RNTCP of GOI, for the first time in the world conceived and implemented the unique experiment of involving the academicians who constitute the faculty in the public health programme for TB control. A mechanism of National, Zonal and State level Task Forces was conceived for the involvement of medical colleges, wherein the sole responsibility of participation of medical colleges in DOTS strategy lies with the faculty of medical colleges, which perhaps made them more responsive.
Involvement of medical colleges in TB control: history and past activities
Since 1997, concerted efforts have been made to involve medical colleges and their hospitals in the Programme when the first National Consensus Conference on TB was held in New Delhi34. This meeting was followed by two meetings in 2001 at the National Tuberculosis Institute (NTI), Bengaluru5 and the All India Institute of Medical Sciences (AIIMS) - World Health Organization, South-East Asia Regional Office (WHO, SEARO), New Delhi Meeting on the Involvement of Medical Colleges in TB and Sexually Transmitted Infections (STI) / HIV Control held at AIIMS, New Delhi6. Professors from over 35 prestigious medical colleges/institutes participated in these meetings and accepted RNTCP as a control programme with potential for a “remarkable success” in TB control in India and expressed their commitment to the Programme. In the meeting recommendations were made to consider medical colleges as an integral part of the RNTCP. As per these recommendations, it was envisaged that medical colleges will offer RNTCP diagnostic and treatment services, teach and carry out advocacy about RNTCP, and participate in implementation and monitoring of the Programme.
The October 2002 National Level Workshop of Medical Colleges at AIIMS, New Delhi, was instrumental in developing the structure and processes required for the effective nation-wide participation of medical colleges in the Programme. Seven medical colleges located in the different zones of the country at New Delhi, Chandigarh (North), Jaipur, Mumbai (West), Kolkata (East), Vellore (South) and Guwahati (North-East) were identified as nodal centres and were requested to lead the initiative of participating in the Programme (Figs 1A and 1B). Nodal faculty members from these seven medical colleges, were trained at the national institutes [e.g., National Tuberculosis Institute (NTI), Bengaluru].
![Structure of medical college involvement in RNTCP: CTD, Central TB Division; NTI, National Tuberculosis Institute, Bengaluru; LRS, Lala Ram Sarup Institute of Tuberculosis and Respiratory Diseases; TRC, Tuberculosis Research Centre [presently known as National Institute for Research in Tuberculosis (NIRT)], Chennai; WHO, World Health Organization; STO, State Tuberculosis Officer; RNTCP, Revised National Tuberculosis Control Programme.](/content/175/2013/137/2/img/IJMR-137-283-g001.png)
- Structure of medical college involvement in RNTCP: CTD, Central TB Division; NTI, National Tuberculosis Institute, Bengaluru; LRS, Lala Ram Sarup Institute of Tuberculosis and Respiratory Diseases; TRC, Tuberculosis Research Centre [presently known as National Institute for Research in Tuberculosis (NIRT)], Chennai; WHO, World Health Organization; STO, State Tuberculosis Officer; RNTCP, Revised National Tuberculosis Control Programme.
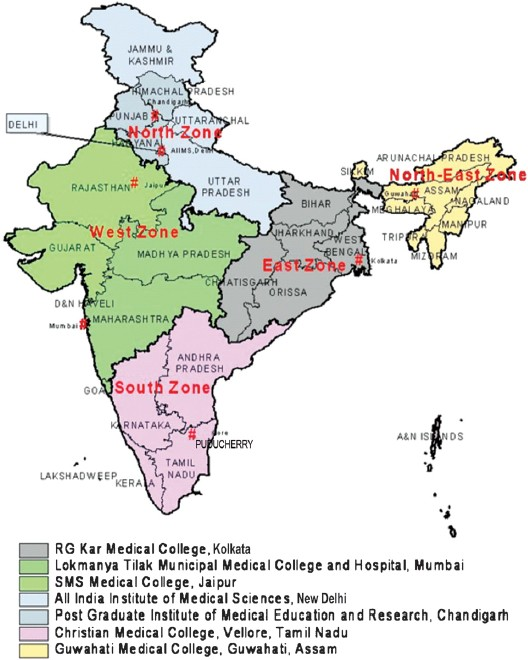
- Various zones and nodal centres as per the structure of medical college involvement in RNTCP.
- RNTCP, Revised National Tuberculosis Control Programme.
Structure of the National, Zonal and State Task Force
A Task Force mechanism at the National, Zonal and State level (Fig. 1A) was established. Subsequently, there were consensus workshops in the States with medical colleges which further detailed the exact mechanisms for collaboration. This formed the basis for GOI's policy of involving medical colleges in TB control.
The National Task Force (NTF) consisted of representatives from the zonal nodal centres, Zonal Task Forces, central TB institutes, WHO-SEARO and the Central TB Division, Ministry of Health and Family Welfare (MoHFW), GOI was formed. The main role of the NTF was to guide, provide leadership and advocacy for the RNTCP, develop policies regarding medical colleges’ involvement in the RNTCP, coordinate between the Central TB Division, MoHFW, GOI, and monitor the activities of the Zonal Task Forces.
The Zonal Task Forces (ZTF) facilitated the establishment of State Task Forces (STF), coordinated between the national and State level Task Forces, as well as between medical colleges and the State/District TB Centres, and monitored the activities of the STF. Zonal division of States for this activity comprised five States in the East, eight each in the North-East, and the North, five in the South and five States in the West zone. However, the real implementing unit was the STF, which undertook the necessary activities to facilitate establishment of Directly Observed Treatment (DOT) centres, as well as other activities, in all the medical colleges in the respective States. Over the subsequent years, wider interaction with medical colleges has occurred through a series of sensitization seminars, training of medical college faculty staff at Central TB institutes, national and zonal level workshops.
Steps for involvement of individual medical colleges included sensitizing faculty members about RNTCP services, identifying a faculty member as a “Nodal Officer” for coordinating RNTCP activities and training of staff. Other steps included formation of a “Core Committee” consisting of the heads of various departments (Box 1). Core Committees, at the level of medical colleges facilitated inter-departmental coordination for implementation of DOTS strategy. Designated Microscopy Centres (DMC) and DOT Centres were established in all government and private medical colleges and these were equipped with suitably trained additional manpower in the form of laboratory technician (LT) and TB health visitor (TBHV). The RNTCP is one of the National Disease Control Programmes being implemented under National Rural Health Mission (NRHM) of GOI. NRHM is implemented through a mechanism of Health Societies established at State and District level. These Health Societies provide necessary administrative and financial support to medical colleges as per approved policy of RNTCP for implementation of Programme activities.
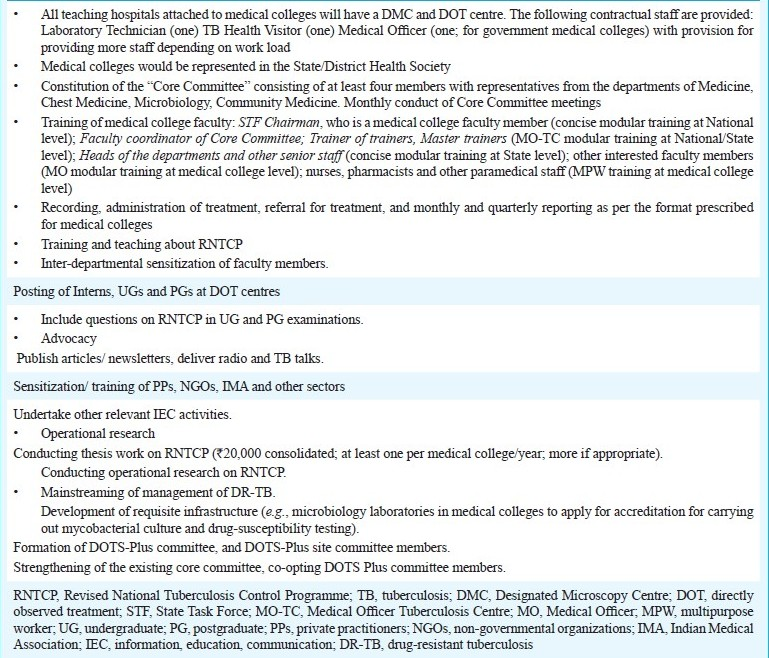
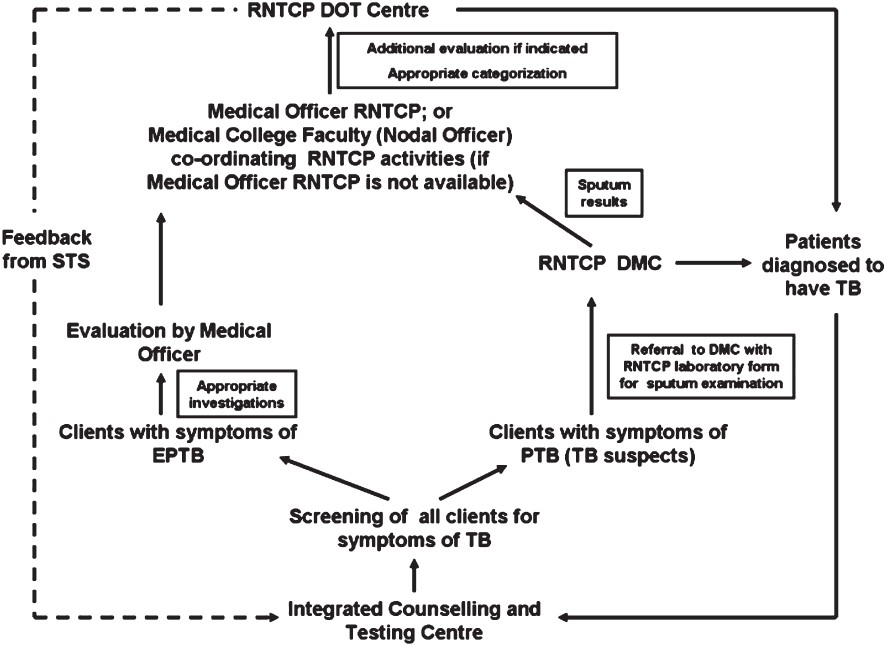
- Framework for the involvement of medical colleges in RNTCP
In 2003, action plans for the different levels of Task Forces were formulated and in 2004, the progress was reviewed and future course of action was planned. These annual meetings of the Task Forces also provided an important forum for consultation with the medical fraternity on issues or new initiatives being considered by the Programme such as external quality assurance of sputum microscopy, drug resistance surveillance, TB/HIV management and coordination, management of M/XDR-TB and DOTS plus7–15.
Recording and reporting formats at the medical colleges
Consequent to the decision in the NTF held in November 2004, NTF 2005 had recommended that the existing recording formats of RNTCP would be used to document the processes in the medical college. Further, the medical colleges submitted the monthly peripheral health institution (PHI) report to the concerned Tuberculosis Unit (TU)/District (Fig. 2). In addition, it was recommended that the medical colleges, States and Zones shall submit reports to the next level on a quarterly basis on separate reporting formats. These were subsequently revised during the NTF workshops held in 2006 and 2007. The quarterly reporting formats have been implemented from the first quarter of 2006 onwards.
- Medical colleges reporting scheme under the Revised National Tuberculosis Control Programme.
- TB, tuberculosis; PHI, Peripheral Health Institution.
Contributions made by medical colleges in RNTCP policy formulation
In addition to the Core Committee meetings, recording and reporting of data, the medical college representatives had actively taken part in the STF meetings and the respective ZTF meetings that were held annually. Further, certain faculty members from medical colleges (e.g., Chairperson STF) also participated in the NTF meeting held annually. The action plans evolved in various ZTF meetings were deliberated upon in the NTF meeting and consensus action plan was evolved for guiding the RNTCP policy. This annual activity had been a key contributor to the RNTCP and responsible for many of the revisions and reforms that have constantly featured in the evolution of the RNTCP.
The NTF has been the voice of the collective opinion of academicians in medical colleges and has contributed in shaping key policy issues, such as, ensuring that teaching and training regarding RNTCP and provision of infrastructural facilities like DMC and DOT Centre at medical colleges are made mandatory by Medical Council of India (MCI); rational use of fluoroquinolone antibiotics in the treatment of respiratory tract infections; airborne infection control policy, among others.
Operational research
The RNTCP facilitated the conduct of operational research (OR) relevant to Programme needs by providing funds. To facilitate conduct of OR, State OR committees were formed in all the States with medical colleges and Zonal OR committees were formed in all the five zones. The OR Committees sanction funding for research projects ranging from up to  100,000 (State OR Committee),
100,000 (State OR Committee),  500,000 to
500,000 to  1,500,000 (Zonal OR Committee) and above
1,500,000 (Zonal OR Committee) and above  1,500,000 (National OR Committee). The RNTCP also instituted a consolidated grant amount of
1,500,000 (National OR Committee). The RNTCP also instituted a consolidated grant amount of  20,000 for postgraduate thesis conducted on OR topics relevant to the Programme needs; at least one postgraduate thesis grant per medical college per year is awarded.
20,000 for postgraduate thesis conducted on OR topics relevant to the Programme needs; at least one postgraduate thesis grant per medical college per year is awarded.
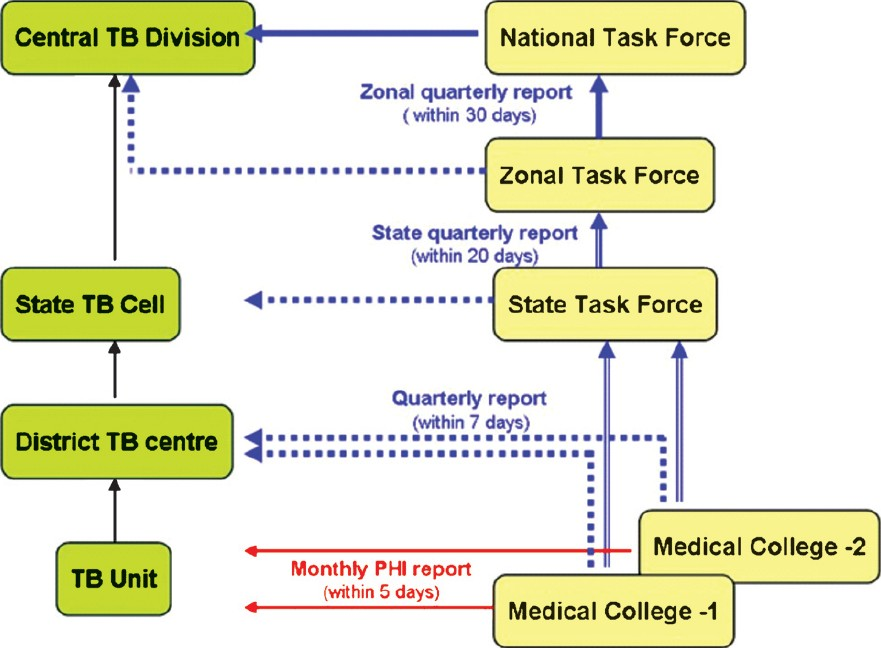
HIV-TB coordination and care
The RNTCP units (DMC and DOT Centre) and the Informed Counselling and Testing Centres (ICTC) in the medical colleges have been actively involved in the HIV-TB cross-referral mechanism (Fig. 3) of the RNTCP and the National AIDS Control Organization (NACO). The medical colleges, by their involvement with NACO, provide facilities for CD4+/CD8+ count testing and provision of anti-retroviral therapy through anti-retroviral treatment (ART) centres for HIV-TB co-infection.
- Referral to and from medical college RNTCP DMC and DOT Centres and ICTC. HIV testing of TB patients should not be done only for the purpose of categorization.
- HIV, human immunodeficiency virus; TB, tuberculosis; ICTC, Integrated Counselling and Testing Centres; RNTCP, Revised National Tuberculosis Control Programme; DMC, Designated Microscopy Centre; PTB, pulmonary tuberculosis; EPTB, extra-pulmonary tuberculosis; HIV, human immunodeficiency virus; STS, Senior Treatment Supervisor.
Management of M/XDR-TB
The diagnosis and treatment monitoring by sputum smear microscopy via quality assured laboratory services are key components of the RNTCP strategy. Keeping pace with its expansion and the increased demand for quality laboratory services, the RNTCP, by facilitating the establishment of accredited Intermediate Reference Laboratories (IRLs) and DOTS-Plus sites at certain medical colleges has also contributed to capacity building for surveillance, diagnosis and treatment of MDR-TB. As a part of this exercise, the RNTCP has facilitated establishment of infrastructure for the diagnosis of MDR-TB by providing line-probe assay, liquid culture and GeneXpert MTB/RIF in future in the IRLs at the medical colleges. Several medical colleges in the country have already obtained accreditation for their laboratories for culture and drug-susceptibility testing under RNTCP; the processing of applications of several other medical colleges in underway.
Key contributions made by medical colleges in TB control in India
The key contributions made by medical colleges in RNTCP policy formulation and programme implementation during the last decade are shown in Box 2.
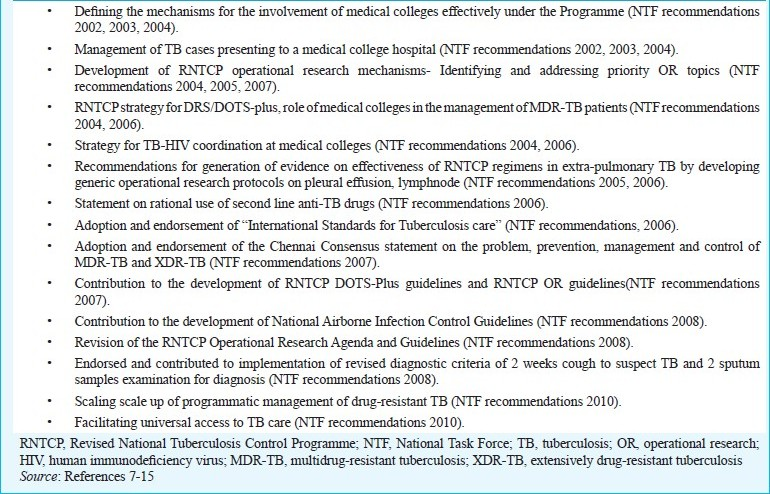
- The key contributions made by medical colleges in RNTCP policy formulation and programme implementation during the last decade
Status of medical college involvement
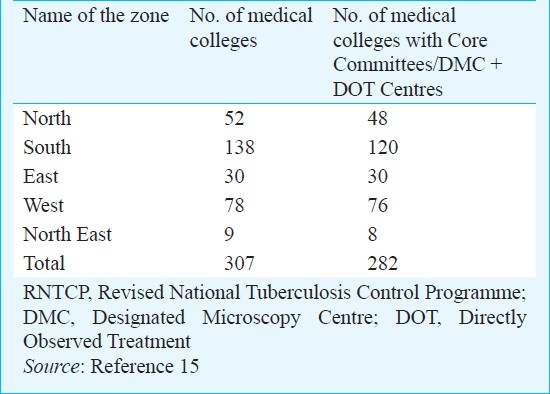
By the end of December 2010, 282 of the 307 (92%) medical colleges were involved in the RNTCP implementation. In these medical colleges, Core committees have been formed and DMC and DOT centres have been established under the Programme (Table I)15. Out of the 282 medical colleges involved, 244 (87%) have submitted their reports for all the quarters during the period July 2009 to June 201015. The remaining medical colleges were new and were in the process of being involved.
Contractual staff provided by RNTCP
By the end of December 2010, RNTCP had sanctioned the following contractual staff: 192 medical officers; 266 LTs; and 258 TBHVs. Of these, 142 medical officers, 245 LTs and 241 TBHVs were in place15.
Microscopy activities at the medical colleges
During the period July 2009 to June 2010, 92,071 of the 6,11,683 patients (15%) who had undergone sputum smear examination for diagnosis at the DMCs in the medical colleges were diagnosed to have smear-positive pulmonary TB. Of these, 18,452 (20%) patients were started on DOTS from the DOT Centres in the medical colleges, while 65,563 (71%) were referred for treatment to the DOT centres at their place of domicile. During the same period, 45115 smear-negative patients and 81,615 patients with EP-TB were either started on DOTS from the DOT Centres in the medical colleges, or were referred for treatment to the DOT centres at their place of domicile. All the DMCs in the medical colleges have actively participated in the quality assurance protocol of the RNTCP which included on-site supervision, panel testing, and random blinded rechecking (RBRC) of routine slides.
Overall, at a national level, medical colleges contributed to 25 per cent of the TB suspects referred for diagnosis, 23 per cent of new smear-positives diagnosed, 7 per cent DOT provision within medical colleges and 86 per cent treatment success rate for new smear-positive patients (Figs 4A and 4B)110–15.
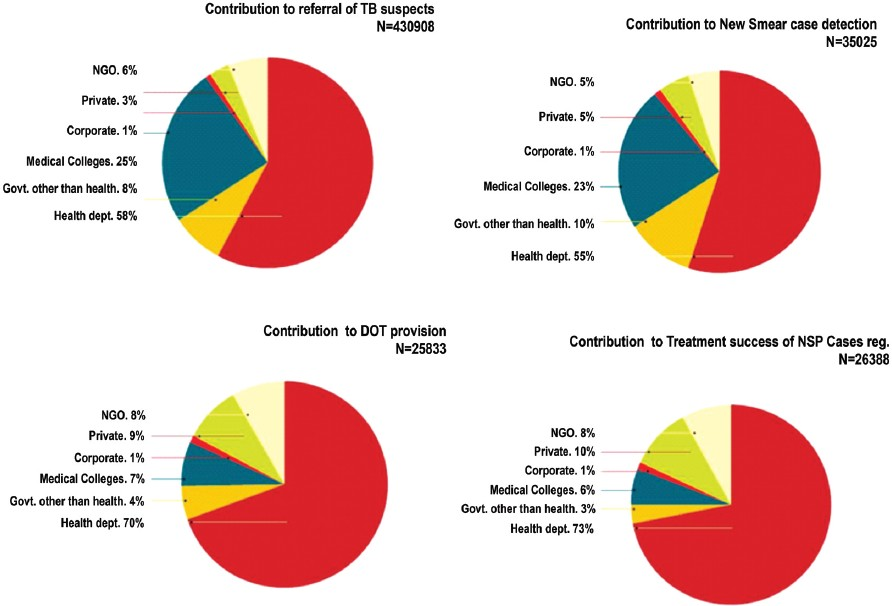
- Contribution of medical colleges to various diagnostic and therapeutic achievements of the RNTCP as documented in 14 districts in the Intensified PPM Project. These districts are large urban areas in 14 different States: Thiruvananthapuram (Kerala), Chennai (Tamil Nadu), Bangalore (Karnataka), Bhopal (Madhya Pradesh), Bhubaneswar (Orissa), Ranchi (Jharkhand), Patna (Bihar), Kolkata (West Bengal), Pune-Mumbai (Maharashtra), Ahmedabad (Gujarat), Jaipur (Rajasthan), Lucknow (Uttar Pradesh), Chandigarh and New Delhi.
- RNTCP, Revised National Tuberculosis Control Programme; PPM, public-private mix; NGO, Non-governmental Organizations Reproduced from Reference 1 with permission
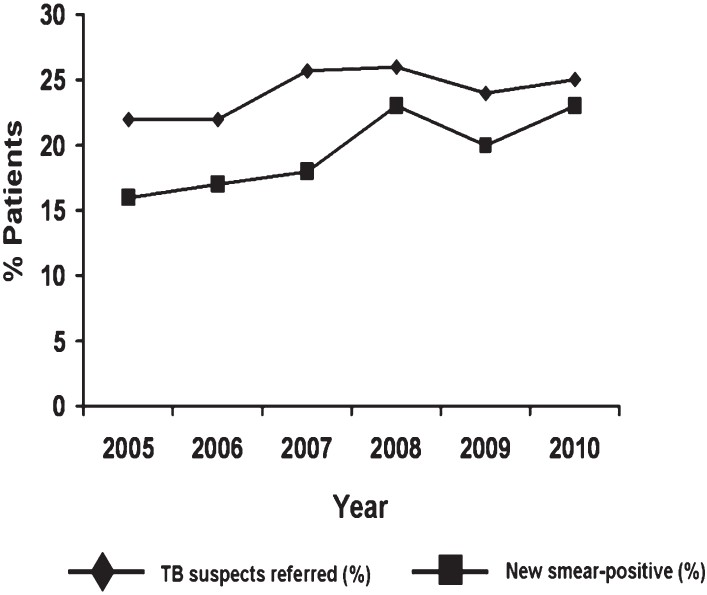
- Annual contribution of medical colleges (2005-2010) to referral of TB suspects and detection of new smear-positive patients under the Revised National Tuberculosis Control Programme.
-
Source: References 6-13.
Referral for treatment and feedback status
Of the sputum positive patients referred for treatment during the period April 2009 to March 2010 the feedback to the referring medical college regarding treatment initiation status has been received from 73 per cent of sputum positive cases, 68 per cent of the sputum negative pulmonary TB cases and 62 per cent of the EPTB cases15.
Supervision and monitoring by the STFs
During July 2009 to June 2010, all States organized at least one STF meeting; in total there were 55 STF meetings. There were 77 medical college visits by the STF members and 19 visits by the ZTF members15.
RNTCP advocacy activities undertaken by medical college staff
The medical colleges have reported 21 publications on RNTCP in peer reviewed journals during the period July 2009 to June 2010. All States have reported participation of the medical college faculty in Television/Radio / Newspapers to disseminate information related to RNTCP. A total of 301 Workshops/Seminars/CMEs (continuing medical education) were conducted on RNTCP in the medical colleges. The medical college faculties have also reported conducting 31 State-level CMEs/workshops on RNTCP across the country during the period15.
TB-HIV collaboration in medical colleges
During July 2009 to June 2010, 216 medical college reported having both ICTC and DMCs in their premises; of these, 205 have established standard cross referrals between ICTC and DMCs. One hundred and forty two medical colleges also have ART centers and at all these centres, mechanisms to refer HIV co-infected patients to RNTCP for diagnosis and treatment of TB have been established15.
Operational research activities undertaken by medical colleges
All the five zones have formed zonal OR Committees, and all the states with medical colleges have the state OR Committees. In 2011, 72 thesis proposals and 14 OR proposals were approved by various Zonal OR Committees1. All the State OR Committees have met atleast once during the period July 2009 to June 2010. The State OR Committees have forwarded 41 OR proposals to the Zonal OR Committee for funding. Of these, 31 proposals have been approved for funding by the Zonal OR Committee. The State OR Committees approved 70 postgraduate thesis proposals for funding from RNTCP. Large multicentric OR studies on efficacy of RNTCP Category III treatment in EPTB, such as lymph node TB16, TB pleural effusions17 and Category I treatment in abdominal TB (patient recruitment ongoing) are expected to provide valuable data on the performance of the RNTCP DOTS regimens.
Participation in the Joint Monitoring Mission
The RNTCP was started on a pilot basis in 1993 based on the recommendations of the first review held in 1992. The second joint programme review, conducted in February 2000, found the functioning of the Programme to be successful and had recommended rapid expansion of quality RNTCP services to cover the entire country by 2005. The third review was conducted in September 2003 by a team of 20 national (including faculty members from medical colleges) and 22 international TB experts. The team made field visits to five States, namely, Maharashtra, Orissa, Rajasthan, Tamil Nadu, and Uttar Pradesh18. The Joint Monitoring Mission (JMM) 2006 was jointly organized by the GOI and WHO during October 200619, and consisted of a team of 24 national experts (including faculty members from leading medical colleges) and 36 international TB experts with the objective of reviewing the performance and plans of the RNTCP, and to recommend steps needed to sustain and further improve the Programme. For reviewing the preparatory activities for DOTS-Plus, the State of Gujarat was selected. To observe TB/HIV activities and to visit the NTI for human resource development (HRD) issues, the State of Karnataka was selected. Three other States were randomly selected from the north and east of the country (Madhya Pradesh, West Bengal, Punjab and Haryana, being smaller States, were combined as one unit). The fourth in the series of JMMs was organized in April 200920 and included representatives from all major national (including faculty members from medical colleges) and international partners of RNTCP. The JMM team had visited five states (Gujarat, Rajasthan, Tamil Nadu, Himachal Pradesh and Uttarakhand) and one Union Territory (Puducherry). The fifth in the series of JMMs organized in August 2012 also included faculty members from medical colleges along with national and international partners of RNTCP. The JMM team had visited 12 districts in six states, namely, Bihar, Maharashtra, Punjab, Karnataka, West Bengal and Uttar Pradesh21.
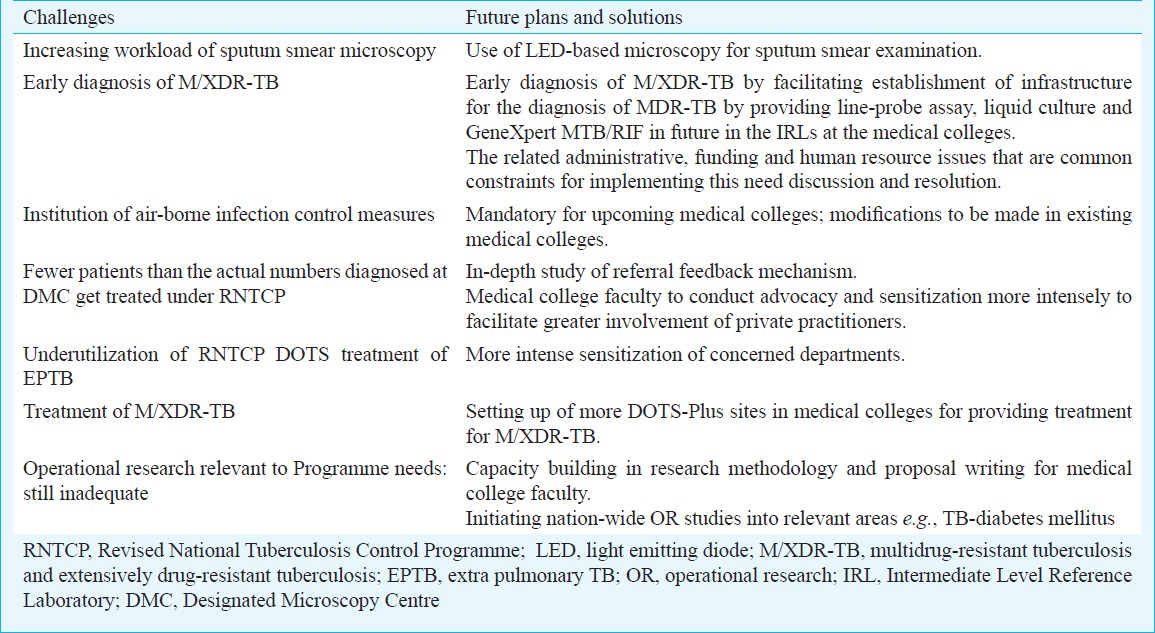
The key Challenges faced in the involvement of medical colleges in the RNTCP and suggested solutions are shown in Table II.
Discussion
Till the time involvement of medical colleges in the RNTCP was conceived, the interaction between the academicians in the medical colleges and the Programme managers was sparse and on many occasions discordant. The young doctors in training seldom got an opportunity to practice what was preached to them22. As a result, the facilities available under the RNTCP were seldom utilized to the full extent possible. Keeping in mind the needs of the country, a future “5-Star” doctor who would take up the responsibilities as a care provider, decision maker, communicator, community leader, and a manager was visualized and such a future doctor would not only serve the patients and the community but would also gain their respect3. The involvement of medical colleges in TB control envisaged and successfully implemented by the RNTCP for more than a decade in India is an extraordinary effort. The Task Force mechanism has entrusted the responsibility to medical colleges to ensure their effective contribution to the efforts of GOI in TB control. The successful amalgamation of the public health approach and the expertise of academicians has immensely benefited the RNTCP and TB control in India and facilitated the emergence of the “future doctor” from among the medical students3.
A model DOT Centre was established at AIIMS, New Delhi, to serve as a role model for other medical colleges in the country with the help of WHO-SEARO in September 20012324. The initial experience gained at this model DOT centre was subsequently adopted for evolving the modus operandi for involvement of medical colleges in the implementation of the RNTCP. During 2001-2005, 1490 patients were evaluated at the DOT Centre at the AIIMS hospital, New Delhi23. Of the 768 patients with cough, 27 per cent were found to be sputum positive for acid-fast bacilli (AFB). Among patients who were initiated on DOTS, cure was achieved in 92 per cent of new sputum smear positive patients; treatment completion was achieved in 91 per cent of EPTB and 75 per cent sputum-negative pulmonary TB patients. Overall treatment success was achieved in 86 per cent24. Further, this is also reflected by the fact that, over the last decade, medical colleges have consistently contributed to nearly 25 per cent of the chest symptomatic referred for sputum smear examination and nearly 20 per cent of new sputum smear-positive patients detected annually (Fig. 4A and 4B).
This reflects a significant achievement because, this large proportion of patients would have otherwise been diagnosed to have TB on radiological or other grounds and not by the reliable sputum smear examination method. These patients would also have received sub-optimal non-DOTS treatment if the medical colleges were not intensely involved in the RNTCP. The robust reporting system that has been developed has provided useful surveillance data and feedback on the functioning of the Programme. Irrespective of which medical college in the country the patient is diagnosed to have TB, the referral mechanisms for treatment have facilitated the delivery of DOTS at the patient's place of domicile.
Medical colleges, by virtue of being referral centres with more facilities for invasive procedures and histopathological and microbiological methods of diagnosis, have enhanced diagnostic yield of EPTB, such as, TB pleural effusion, lymph node TB, abdominal TB, neurological TB, among others. These have, thus, contributed to early diagnosis of EPTB cases and facilitated institution of the standard of care i.e., DOTS for these patients. Medical college involvement has also facilitated more active involvement of paediatricians in the RNTCP and effective utilization of RNTCP diagnostic and therapeutic services for paediatric TB.
Some problems have been identified in the implementation of RNTCP activities in medical colleges, especially in the new medical colleges set up in the private sector. These include delay in formation of Core Committees, establishment of DMCs in some of the medical colleges. Technical doubts about efficacy of DOTS regimens particularly in EPTB cases have lingered on. Consequently, many patients with EPTB, especially, orthopaedic and neurological TB are being treated with non-DOTS treatment resulting in inadequate utilization of the RNTCP programme.
Constraints and challenges ahead
The inadequacies in staff and human resources shortage at all levels requires rectification. Issues, such as, staff vacancies in medical colleges not being filled up on time, and salaries to RNTCP contractual staff not being at par with payments in the sector also need to be addressed. In some states, delay/non-release of funds to STFs has resulted in non-performance of planned activities. There is a need to ensure financing essential for sustenance of this model. In states with a large number of medical colleges, such as Karnataka, visit by the STF Chairperson has become a practical problem. Increasing the number of STF Chairpersons could perhaps be a solution to this problem. Poor and inadequate airborne infection control practices in most of the medical colleges, especially the overcrowded government medical colleges has been another issue of concern. There is an urgent need for advocacy regarding education on cough hygiene and etiquette. Weaknesses that are evident in supervision capacity and quality as well as in planning, monitoring and evaluation need to be addressed.
In medical colleges, there is a need for enhanced inter-departmental sensitization and better advocacy for RNTCP and need for more contribution in pulmonary TB (smear-positive and smear-negative cases) and EPTB cases. There is also a need for strengthening the feedback for transferred out cases. This can be facilitated by holding regular core committee meetings, more intense and sustained sensitization regarding the Programme and enhanced inter-departmental cooperation. Establishment of IRLs and DOTS-Plus sites for M/XDR-TB in medical colleges would contribute to capacity building and strengthening of mycobacteriology laboratory services in the department of microbiology in medical colleges. Availability of quality assured accredited laboratories in medical colleges would facilitate better management of drug-resistant TB and HIV-TB co-infection. Active medical college involvement in prior planning and efficient management of drug logistics cycle will avoid shortages and will ensure timely supply of drugs. However, in spite of all these deterrents and shortcomings, the landmark decision taken more than a decade ago to involve medical colleges in TB control appears to have extraordinary foresight. This has resulted in the establishment of DOTS as the standard of care for TB patients in all medical colleges and their hospitals. It is expected that through their own practice, senior faculty (professor) in medical colleges will influence the practice in the private sector as well as the future generation of physicians thus making DOTS the standard of care for TB patients in the country. This will ensure that all TB patients, irrespective of where they seek care, receive the best available care, free of cost. Several issues need to be streamlined and improved upon in the coming years to make this partnership between the RNTCP and the medical colleges a truly effective collaboration.
As the Programme widens the scope of services that it provides, medical colleges will have an increasingly important role to play in areas such as TB/HIV co-infection, external quality assurance of the sputum microscopy network, drug-resistance surveillance and management of multidrug-resistant TB patients. The RNTCP needs active support of medical colleges in carrying out OR in these areas to guide the development of the Programme's future policies. Recently, medical colleges have also begun participation in airborne infection control policy implementation25. This will involve engineering works, renovation of existing infrastructure by involving medical college authorities. Medical colleges also have the potential for evaluating the efficacy of isoniazid preventive treatment (IPT) in the field setting. Thus, by their active involvement in the “3Is”, namely, intensified case finding, (airborne) infection control policy, and IPT medical colleges are active partners in the implementation of the RNTCP.
The beginning and the progress made so far seem promising. But, the need of the hour is to sustain the momentum gained and push medical college involvement forward by continuing coordination and communication. The OR relevant to the Programme needs can be further facilitated by providing attractive funding and a clear-cut modus operandi with a specified time-line so as to attract interested faculty members from medical colleges to take up research studies. Identifying thrust areas relevant to current needs of the Programme, and making available quality generic protocols can facilitate OR studies to be carried out in medical colleges in multicentre mode. There is also a need for visible networking to facilitate the widespread dissemination of the outcomes and results documented in the OR studies so that this will also enthuse and inspire more research relevant to the Programme needs. The experience from India in involving medical colleges in national Programme shows that tangible additional benefits can be obtained in TB control, especially by improving case detection. In view of this, involvement of medical colleges should be promoted widely and the experience replicated not only in the region but also globally.
References
- Central TB Division. TB India 2012. Revised National TB Control Programme. In: Annual Status Report. New Delhi: Central TB Division, Ministry of Health and Family Welfare, Government of India; 2012.
- [Google Scholar]
- The Revised National Tuberculosis Control Programme (RNTCP) In: Sharma SK, Mohan A, eds. Tuberculosis (2nd ed). New Delhi: Jaypee Brothers Medical Publishers; 2009. p. :894-917.
- [Google Scholar]
- The role of medical schools in tuberculosis control. In: Sharma SK, Mohan A, eds. Tuberculosis (1st ed). New Delhi: Jaypee Brothers Medical Publishers; 2001. p. :597-600.
- [Google Scholar]
- The role of medical colleges in tuberculosis control. In: Sharma SK, Mohan A, eds. Tuberculosis (2nd ed). New Delhi: Jaypee Brothers Medical Publishers; 2009. p. :839-45.
- [Google Scholar]
- Medical College Conference on RNTCP, Bangalore. 2001. Available from: http://www.tbcindia.nic.in/Press%20release%20Bangalore.html
- [Google Scholar]
- AIIMS-WHO Meeting on the Involvement of Medical Schools in TB and STI/HIV Control. Report on an Informal Consultation on November 28-30, 2001 and Follow-up meeting on April 29, 2002
- [Google Scholar]
- Recommendations of the 1st National Task Force meeting for Involvement of Medical Colleges in the RNTCP, New Delhi, October 29-31, 2002. Available from: http://tbcindia.nic.in/Pdfs/NTF%20Rec%202002.pdf
- [Google Scholar]
- Recommendations of the 2nd Meeting of the National Task Force for involvement of Medical Colleges in the RNTCP, New Delhi, November 22, 2003. Available from: http://tbcindia. nic.in/pdfs/Recomm%202nd%20NTF%20ws%20Nov03%20FINAL.pdf
- [Google Scholar]
- Recommendations of the 3rd National Task Force Meeting for Involvement of Medical Colleges in the RNTCP, New Delhi, November 23-24, 2004. Available from: http://tbcindia.nic.in/pdfs/Recomm%203rd%20NTF%20mtg%20Nov04%20Final.pdf
- [Google Scholar]
- Recommendations of the 4th National Task Force Meeting for Involvement of Medical Colleges in the RNTCP, New Delhi, November 3-5, 2005. Available from: http://tbcindia.nic.in/Pdfs/Minutes%20and%20Recommendations%20of%20the%20NTF%202005.pdf
- [Google Scholar]
- Recommendations of the 5th National Task Force Meeting for Involvement of Medical Colleges in the RNTCP, New Delhi, November 9-11, 2006. Available from: http://tbcindia.nic.in/Pdfs/Minutes%20and%20Recommendations%20of%20NTF%202006.pdf
- [Google Scholar]
- Recommendations of the 6th National Task Force Meeting for Involvement of Medical Colleges in the RNTCP, New Delhi, October 29-31, 2007. Available from: http://tbcindia.nic.in/Pdfs/Minutes%20and%20Recommendations%20of%20NTF%202007.pdf
- [Google Scholar]
- Recommendations of the 7th National Task Force Meeting for the Involvement of Medical Colleges in the RNTCP, New Delhi, October 22-24, 2008. Available from: http://tbcindia.nic.in/Pdfs/NTF%20_2008_%20recomendations.pdf
- [Google Scholar]
- Recommendations of the eighth National Task Force meeting for the Involvement of Medical Colleges in the RNTCP, New Delhi, October 30-31, 2009. Available from: http://tbcindia.nic.in/Pdfs/NTF%20_2009_%20recomendations.pdf
- [Google Scholar]
- Report of the National Task Force 2010.Presented at the National Task Force Meeting for involvement of Medical Colleges in the RNTCP, Hyderabad, 18-20, January 2011. Available from: http://tbcindia.nic.in/documents.html
- [Google Scholar]
- Tuberculous lymphadenopathy: a multicentre operational study of 6-month thrice weekly directly observed treatment. Int J Tuberc Lung Dis. 2013;17:234-9.
- [Google Scholar]
- Outcomes of Category III DOTS treatment in immunocompetent patients with tuberculosis pleural effusion. Int J Tuberc Lung Dis. 2012;16:1505-9.
- [Google Scholar]
- Joint Tuberculosis Programme Review, India. September 2003. SEA-TB-265. 2003. New Delhi: World Health Organization Regional Office for South-East Asia; Available from: http://209.61.208.233/LinkFiles/Reports_sea-tb-265.pdf
- [Google Scholar]
- Joint Tuberculosis Programme Review, India, 2006. 3-17 October 2006. SEA-TB-299. 2006. New Delhi: World Health Organization Regional Office for South-East Asia; Available from: http://203.90.70.117/PDS_DOCS/B0628.pdf
- [Google Scholar]
- Joint Monitoring Mission Revised National Tuberculosis Control Programme (RNTCP), India. 15-28 April 2009.SEATB-321. 2009. New Delhi: World Health Organization Regional Office for South-East Asia; Available from: http://www.tbcindia.nic.in/Pdfs/JMM-Report-2009.pdf
- [Google Scholar]
- WHO-Gol Joint Monitoring Mission 2012. Key Observations and Recommendations. Available from: http://www.tbpartnershipindia.org/Documents/WHO-GOI%20Joint%20%20Monitoring%20Mission%202012%20_Debrief.pdf
- [Google Scholar]
- Medical schools and tuberculosis control: bridging the discordance between what is preached and what is practiced. Indian J Chest Dis Allied Sci. 2004;46:5-7.
- [Google Scholar]
- DOTS centre at a tertiary care teaching hospital: lessons learned and future directions. Indian J Chest Dis Allied Sci. 2004;46:251-6.
- [Google Scholar]
- DOTS at a tertiary care center in northern India: successes, challenges and the next steps in tuberculosis control. Indian J Med Res. 2006;123:702-6.
- [Google Scholar]
- Central TB Division, Directorate General of Health Services, Ministry of Health & Family Welfare, Govt. of India. Guidelines on Airborne Infection Control in Healthcare and Other Settings. In the context of tuberculosis and other airborne infections April 2010. Available from: http://www.tbcindia.nic.in/pdfs/Guidelines_on_Airborne_Infection_Control_April2010P rovisional.pdf
- [Google Scholar]






