Translate this page into:
Contact with HIV prevention programmes & willingness for new interventions among truckers in India
Reprint requests: Dr Rakhi Dandona, Addl. Professor, Public Health Foundation of India, ISID campus, 4 Institutional Area, Vasant Kunj, New Delhi 110 070, India e-mail: rakhi.dandona@phfi.org
-
Received: ,
This is an open-access article distributed under the terms of the Creative Commons Attribution-Noncommercial-Share Alike 3.0 Unported, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Background & objectives:
Systematic data on existing coverage and willingness for HIV prevention strategies among truckers are not readily available in India. The present study aimed to further the understanding on contact of truckers with existing HIV prevention services and to assess willingness for new HIV prevention strategies.
Methods:
A total of 1,800 truck drivers and helpers aged 16-65 yr passing through Hyderabad were approached to assess contact made with HIV prevention programmes, history of previous HIV testing and their acceptance for circumcision, oral HIV testing, new medications to control HIV (PrEP) and telephonic counselling. Dried blood samples were collected on filter paper and tested for HIV. Multiple logistic regression was performed for analysis of association between contact with HIV prevention programme and socio-demographic, sexual risk behaviour variables and work characteristics.
Results:
A total of 1,602 (89%) truckers gave interview and provided blood sample. Forty five truckers tested positive for HIV resulting in HIV prevalence of 2.8 per cent (95% CI 2.0-3.6%). Only 126 truckers (7.9%; 95% CI 6.5-9.2%) reported ever being contacted by staff providing HIV prevention interventions. Previous HIV testing was reported by19 per cent (95% CI 17.3-21.2%). Those reporting contact with HIV prevention programmes ever were more likely to have undergone HIV testing (odds ratio 3.6, 95% CI 2.4-5.4). The acceptance for pre-exposure prophylaxis (PrEP) was 87 per cent, oral HIV testing 98 per cent, and telephonic counselling 82 per cent, but was only 9 per cent for circumcision. Truckers who reported having sex with a man and those who halted regularly at dhabas were significantly more willing to undergo circumcision for HIV prevention (odds ratios 2.7, 95% CI 1.4-5.4 and 2.1, 95% CI 1.3-3.2, respectively).
Interpretation & conclusions:
Our findings showed that truckers had low contact with HIV prevention programmes, suggesting a need for urgent measures to reach this population more effectively. The willingness for new HIV interventions was high except for circumcision. These findings could be used for further planning of HIV prevention programmes for truckers in India.
Keywords
Circumcision
HIV
HIV prevention programmes
oral HIV testing
truck drivers
Truck drivers and helpers (truckers) are known to be at an increased risk for HIV and other sexually transmitted infections (STIs) in India123. There are about 5-6 million truck drivers and helpers in India, of whom approximately 3.5 million are long-distance truckers4. At the population-level, truckers are 2-5 times more likely to be HIV-infected than men in other professions5.
The extant literature on truckers from India has focused mostly on prevalence and risk factors of HIV transmission with little focus on utilization of HIV prevention services67891011. We have previously reported that even though the publicly-funded HIV prevention programmes for truck drivers in the State of Andhra Pradesh are cost-effective7, truckers on an average made only 2.2 contacts annually with these programmes which was grossly inadequate to yield desired and sustained HIV intervention impact8. HIV prevention interventions have been focused on truckers in India since 1996 with funding from the National AIDS Control Organization (NACO)12, however, de-emphasis of HIV prevention programming targeting this population has occurred.
As reducing HIV infection in truckers could have a potential beneficial impact on HIV infection at large, we undertook this study to improve our understanding on contact of truckers with existing HIV prevention services and to assess their willingness to go for HIV prevention strategies not currently part of the National Programme in India [circumcision, oral HIV testing, medications to control HIV- i.e. pre-exposure prophylaxis (PrEP) and telephonic counselling] but have received much attention in some other settings131415.
Material & Methods
We conducted a study of truck drivers and helpers (truckers) who transited through Hyderabad city in southern India during 2010-2011. The study protocol was approved by the Human Ethics Committees of the Public Health Foundation of India, New Delhi, MEDICITI- Hyderabad, and the Lifespan/Tufts/Brown Centre for AIDS Research, Providence, USA, and was also approved by the Health Ministry Steering Committee, Government of India.
Sample size and selection of participants: Assuming HIV prevalence of 6 per cent from the previous literature in this population16, the target sample size was 1,200 truck drivers and 600 helpers in order to get at least 90-100 cases of HIV positivity. Long-haul truckers working on trucks of N1 and N2 categories (3.5 tonnes or below and up to a maximum mass of 12.5 tonnes) as per the Central Motor Vehicles Rules of India17 travelling a minimum of 800 kilometres one-way, and those aged between 16 to 65 yr with primary occupation as a trucker for at least 3 months prior to the study, and speaking any of three languages- Hindi, Telugu or English- were considered eligible to participate.
The potential participants were recruited from 12 halt points along the four major entry routes around Hyderabad. The halt points included private parking areas, transport company parking areas, and parking areas around petrol pumps. Proportional sampling technique was followed to maintain adequate representation of truckers to their estimated available numbers at each halt point based on a scoping exercise. As trucks were parked in an organized fashion in most of these halt points, systematic listing of the trucks parked (from entry to exit point) was undertaken to document the vehicle number, whether long-haul truck or not, number of truckers per truck with their age and language spoken by them. This information was used to identify the eligible truckers for the study. A potential respondent was chosen to participate in the study from every 3rd or 5th truck depending on the sample size required from each halt point with the first respondent chosen randomly from the sampling interval. The sample of truckers at halt points ranged from 50 to 180. Drivers and helpers from the same truck were not recruited. To avoid re-interview, a record of the truck registration number of the already recruited truckers was maintained to avoid duplication. Ten interviews on an average were conducted each day.
Data collection: Potential participants were contacted by a team of three trained interviewers during April to November 2010. Written informed consent for participation was sought from each participant following which the interviewers conducted interview using a questionnaire designed specifically to meet the objectives of this study. The questionnaire was translated into Hindi and Telugu for administration by ensuring conceptual and semantic equivalence with the English version. The bilingual study research staff worked with a set of truckers throughout the process of translation and back-translation to address inconsistencies and cultural nuances relevant in this context, and to arrive at appropriate wording for those with a low literacy level. Each participant was asked a series of questions about lifetime history of sexual contact, risk behaviour, HIV/STI prevention practices and beliefs, contact with HIV/STI prevention services, STI history, and their attitudes towards circumcision as HIV prevention intervention, oral HIV testing, new medications for HIV prevention, and telephonic counselling. Interviews were conducted in private either in a separate room provided by the transport agency on request or in many instances inside the truck cabin in order to ensure privacy.
At least five drops of blood were collected on a filter paper (Whatman No. 3; Whatman International Ltd, Maidstone, Kent, UK) by finger-prick method following the interview. All samples were initially tested for HIV antibody or antigen by a fourth-generation ELISA (Genscreen ULTRA HIV Ag-Ab, Bio-Rad, France), and the positive samples were tested by a fourth-generation ELISA (Vidas HIV Duo Ultra; bioMérieux, Marcy-l’Etoile, France) to confirm the presence of HIV antibody or antigen. Blood samples were also tested for HSV2 IgG (HerpeSelect 2 ELISA IgG, FOCUS Diagnostics, California, USA) and syphilis (Treponostika TP recombinant, bioMérieux, Marcy-l’Etoile, France).
As the HIV test results were unlinked to the participant identity, those interested in knowing their HIV status were referred to the nearest voluntary counselling and testing centre. All participants were offered a blanket valued at  120 (USD 2.7) and a free-of-cost first visit referral to the GATI community health clinic in Hyderabad as a token of appreciation for their participation.
120 (USD 2.7) and a free-of-cost first visit referral to the GATI community health clinic in Hyderabad as a token of appreciation for their participation.
Data analysis: SPSS version 17.0 (SPPS Statistics Standard, USA) was used for data analysis. Descriptive statistics were calculated for relevant quantitative variables. The analysis of contact with HIV prevention programme among truckers was done along with its associations with socio-demographic, work characteristics and sexual risk behaviour variables using multiple logistic regression. The frequency of such contacts and types of services provided during such contacts were recorded. Trucking routes for this analysis were classified as south-east (Tamil Nadu, Andhra Pradesh, Assam, Bihar, Chhattisgarh, Jharkhand, Nagaland, Orissa, and West Bengal), south-west (Karnataka, Kerala, Andhra Pradesh, Maharashtra, Goa, Gujarat and Rajasthan), and others. Certain behavioural risk factors were compared between those who were ever contacted by HIV prevention programme and those who had no such contact. Multiple logistic regression was also performed for the associations of HIV prevalence and of having tested for HIV previously in truckers with various socio-demographic (age, literacy, state of residence) and work-related characteristics (type of trucker, duration of work as trucker, frequently travelled route, type of halt point) and sex-related risk behaviour [sex with female sex worker (FSW), sex with men, last female sex partner, contact with HIV prevention programmes). As 99.4 per cent of the Hindu respondents were not circumcised and 96.9 per cent of Muslim respondents were circumcised, religion and circumcision were not used as variables in the model.
Results of acceptance of three types of HIV interventions are presented. A brief description about these viz. medications that could prevent HIV transmission, HIV test using oral swab and circumcision was given to each participant. Following the description of each, participant's comprehension was assessed through a teach-back approach18. Next, they were asked a set of five questions to assess their likelihood of acceptance to get more information and potentially utilize these interventions. The responses were recorded using a 4-point Likert scale (very likely to very unlikely). For this analysis, very likely and likely responses were considered as likelihood of acceptance to get more information about these interventions or to utilize these. The participants were also asked about likelihood of considering counselling for sensitive/personal health matters over phone. Multiple logistic regression results are presented for likelihood of considering circumcision as HIV prevention intervention and for telephonic counselling with socio-demographic, work characteristics and behavioural risk variables. In all multiple logistic regression models, the effect of each category of a multi-categorical variable was assessed by keeping the first or last category as reference and all the variables considered were introduced simultaneously in the model and 95% confidence interval (CI) for the odds ratio (OR) are presented.
Results
A total of 1,800 truckers aged 16-65 yr were recruited for the study from 12 halt points of whom 1,608 (89.3%) were interviewed and 1,602 (89%) participants gave blood sample. Of these 1,602 participants, 1,047 (65.4%) were truck drivers and 555 (34.6%) truck helpers. Table I shows the details of socio-demographic, work characteristics and behavioural risk variables of these participants. The median duration of work as a truck driver was 9 yr (range 1-40 yr) and as a helper was 2 yr (range 1-40 yr). Eighty one truckers (5.1%) reported having sex with other men, of whom 47 (58%) reported to have had sex with a man one time only. Of these 81, 46 (56.8%) reported insertive sex with men, and 56 (69.1%) did not use a condom for the last sex act with a man. The median number of lifetime male sex partners was 1.00 (range 1 to 20) for truckers.
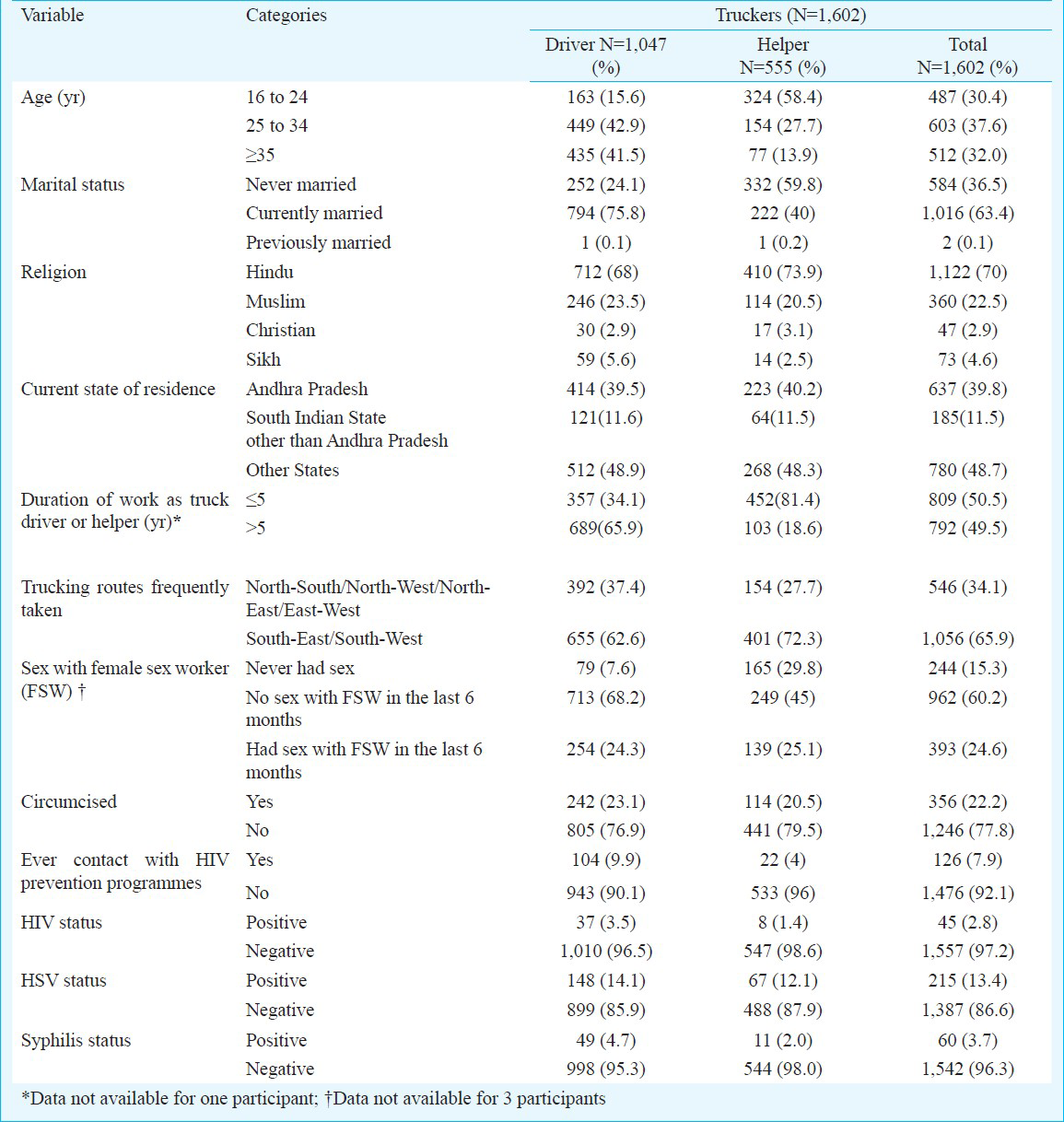
A total of 45, 215 and 60 truckers tested positive for HIV, HSV and syphilis, respectively. The prevalence of HIV was 2.8 per cent (95% CI 2.0-3.6%), HSV was 13.4 per cent (95% CI 11.7-15.1%) and of syphilis was 3.7 per cent (95% CI 2.8-4.7%). With multiple logistic regression, those not circumcised (OR 4.7, 95% CI 1.4-15.6) and those who frequently parked trucks at parking lots (OR 1.9, 95% CI 1.0-3.5) were significantly more likely to be HIV positive (data not shown).
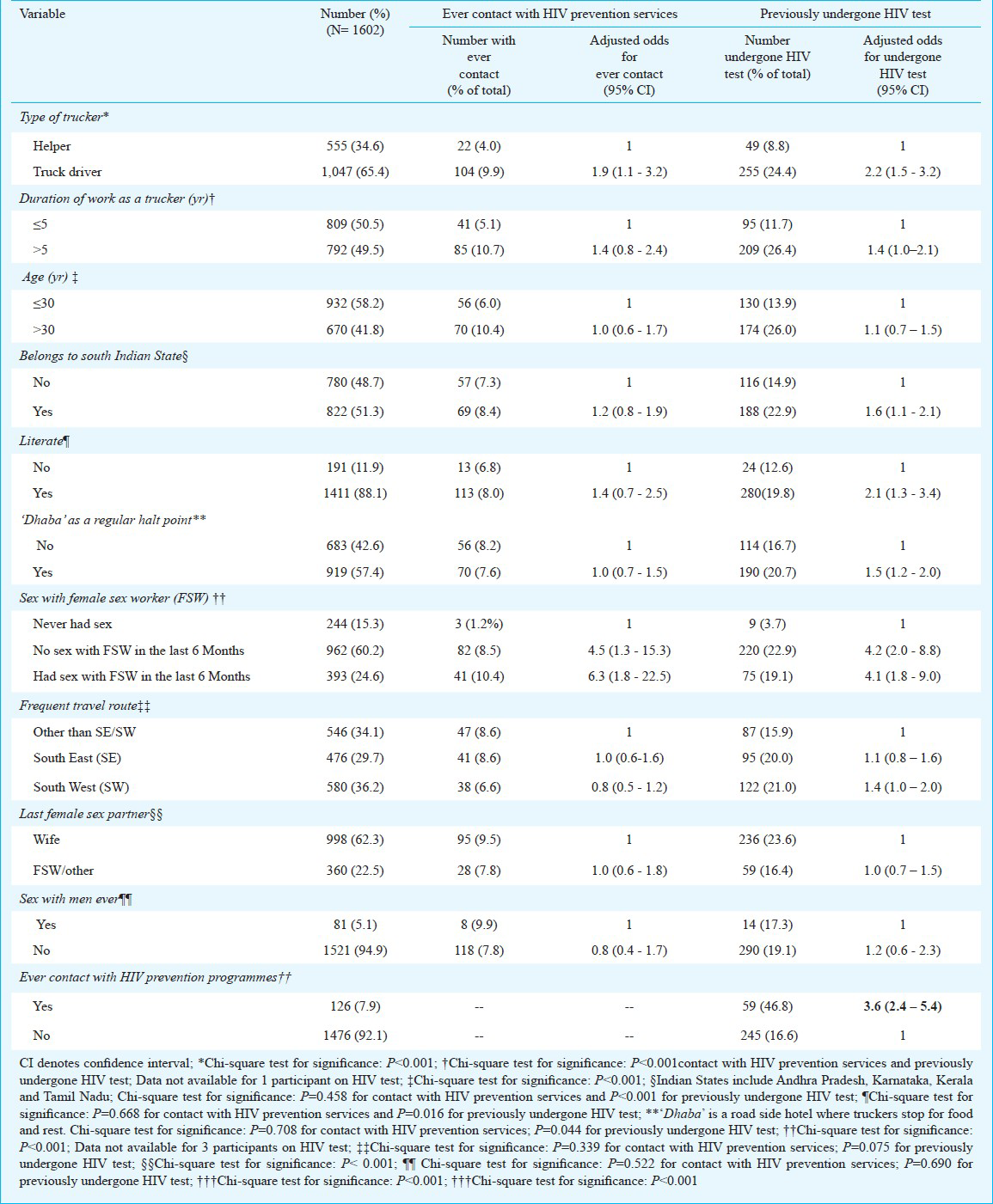
Contact with HIV prevention programmes: Of the 1,602 participants, only 126 truckers (7.9%; 95% CI 6.5-9.2%) reported being contacted at least once by a person/NGO staff providing HIV prevention interventions. However, 98 (6.1%; 95% CI 4.9-7.3%) of the 1,602 truckers reported that they had met someone providing HIV prevention services only once. A little over half of such contacts were made in Hyderabad city (54.8%). In adjusted analyses, those who reported having sex with FSW in the last 6 months (OR 6.3, 95% CI 1.8-22.5) as compared with those who never had sex, and truck drivers (OR 1.9, 95% CI 1.1-3.2) as compared with cleaners were significantly more likely to report a contact with HIV prevention programmes ever (Table II). Those who reported not having sex with FSW in the last 6 months had lower odds (OR 4.5, 95% CI 1.3-15.3) of reporting a contact with HIV prevention services than those who reported sex with FSW in the last 6 months.
Among the various kinds of services provided during such contacts, the major ones were provision of information on HIV/STI including printed materials (54.9%), information of safe sex (18.4%) and provision of free condoms (13%), whereas HIV testing (7.2%) and provision of free medication for STIs were the lowest (6.5%).
Significantly lower proportion of those with contact ever with HIV prevention programmes reported FSW as the partner for last sex episode as compared with those with no contact ever with such programmes (Fig.). However, the former were significantly more likely to report a woman other than wife/FSW to be the last sex partner as compared with the latter (Fig.). Among the 1,353 who reported having sex ever, 336 (24.8%) truckers reported more than one sex partner in the last 6 months. A higher proportion of truckers (38; 30.9%) among the 123 truckers who reported contact ever with HIV prevention programmes reported more sex partners in the last 6 months as compared with 298 (24.2%) of the 1,230 truckers who reported no contact ever with HIV prevention programmes. Among the 258 (16.1%) truckers who reported having experienced genital symptoms ever, the former were significantly more likely to get treatment for genital symptoms as compared with the latter.

- Exposure to HIV prevention services by select variables for truckers. *Data not available for 5 participants; †Chi-square test for significance, P<0.001; ‡Chi-square test for significance, P=0.029.
Previously tested for HIV: Of the 1,602 participants, 304 (19%, 95% CI 17.3-21.2%) truckers reported having undergone HIV testing previously. With multiple logistic regression, those reporting no sex with FSW in the last six months (OR 4.2, 95% CI 2.0-8.8), those with contact ever with HIV prevention programmes (OR 3.6, 95% CI 2.4-5.4), truck drivers (OR 2.2, 95% CI 1.5-3.2), those literate (OR 2.1, 95% CI 1.3-3.4) and those who halt regularly at dhabas (OR 1.5, 95% CI 1.2-2.0) were significantly more likely to have undergone HIV testing previously (Table II). Among the 304 truckers who had undergone HIV testing previously, the most common place of HIV testing was a private clinic/hospital (47.7%), and the most common reason reported for having undergone HIV testing was doctor's advice for illness/surgery (32.2%) followed by voluntary testing (29.9%).
Likelihood of acceptance for HIV interventions:
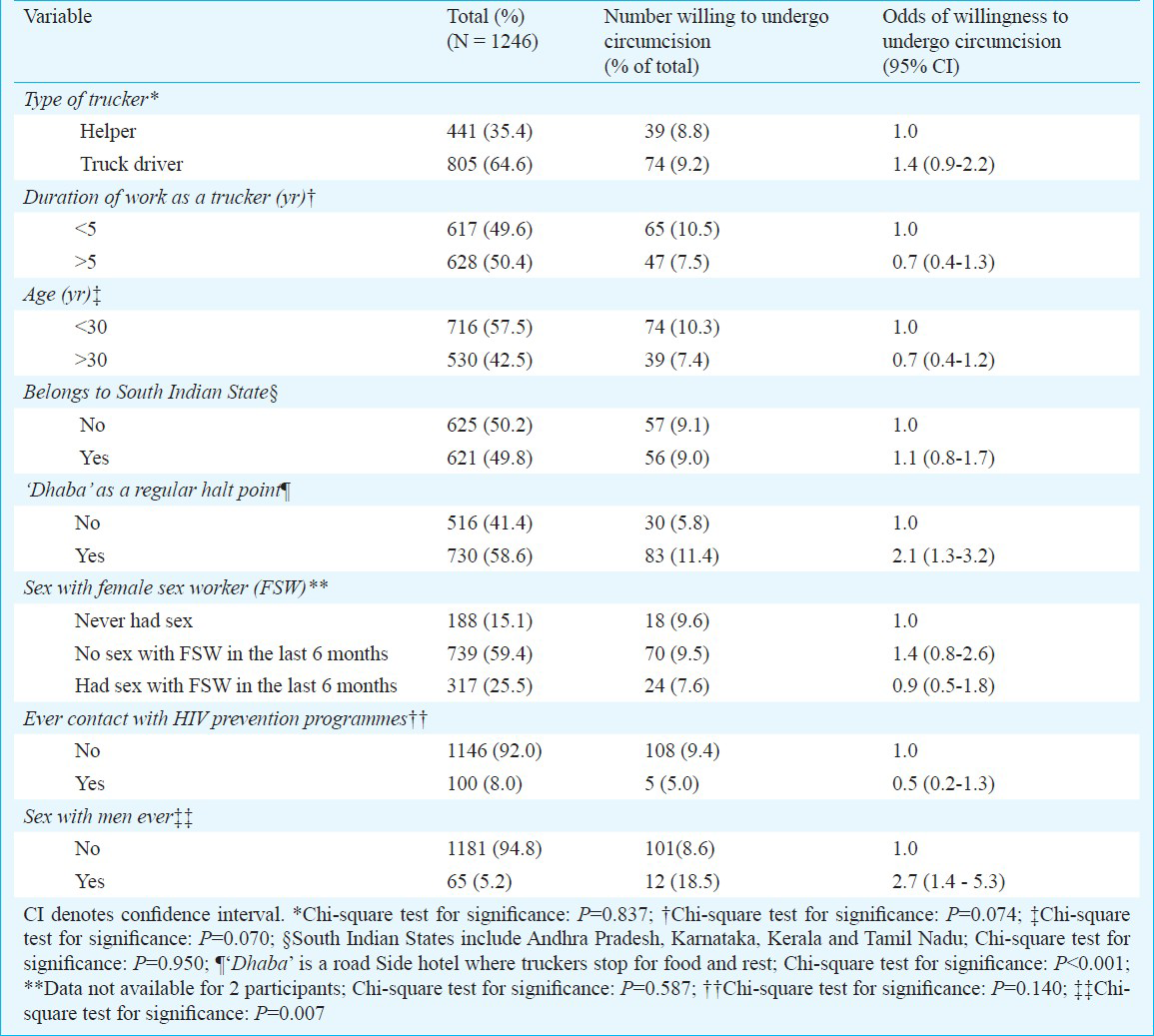
Circumcision - Of the 1,602 participants, 1,246 (77.8%) truckers reported that they were not circumcised. Of these, 198 (15.9%) were likely to get more information about circumcision for HIV prevention, 183 (14.7%) were likely to recommend it to their friends, 112 (9%) expressed interest in getting circumcised if provided free over the next 3 years by a healthcare provider, and 106 (8.5%) were likely to pay to get circumcised. On applying multiple logistic regression, truckers who halt regularly at dhabas (OR 2.1, 95% CI 1.3 - 3.2) and those who reported having sex with a man ever (OR 2.7, 95% CI 1.4 - 5.3) were significantly more likely to be accept circumcision for HIV prevention (Table III).
New medications for HIV control - The participants were asked if they would accept taking a pill in near future either to be taken once daily or one pill a day for 28 days to prevent HIV infection. Of the 1,602 participants, 1,398 (87.3%) truckers were likely to get more information about such a new medication if it became available, and 1,350 (84.3%) expressed interest in obtaining this medication if provided free over the next 3 years by a healthcare provider and 1,214 (75.8%) were likely to pay for it. Of the 1,377 truckers who were likely to consider this new medication, 582 (42.3%) were likely to consider taking a pill once a day and 795 (57.7%) for a pill one day before sex and then for 28 days. A total of 1,393 (87%) truckers were likely to recommend it to their friends, if necessary.
Oral HIV testing - All participants were briefed about testing for HIV using oral swab and then asked about their likelihood to utilize it. Of the 1,602 participants, 1,572 (98.1%) truckers were likely to get more information about the HIV oral test, 1,557 (97.2%) expressed interest in considering this test if provided free over the next 3 years by a healthcare provider, 1,379 (86.1%) were likely to pay for it, and 1,478 (92.3%) were likely to recommend it to their friends, if necessary.
Telephonic counselling - Of the 1,602 participants, 1,014 (63.3%) truckers reported possessing a mobile phone, of whom 76 per cent were truck drivers. Among the 1,014 who reported possessing a mobile phone, 831 (82%) were likely to consider discussion of sensitive or personal health information over phone with a doctor/health care provider. The remaining preferred to discuss such information in person. When asked about the possibility of receiving HIV test results over phone instead of in person, 838 (82.6%) preferred receiving results over phone. On applying multiple logistic regression, those frequently parking trucks at the dhabas (OR 2.2, 95% CI 1.6-3.1) were significantly more likely to prefer discussing sensitive or personal health information with a health care provider over a mobile phone (detailed data not shown).
Discussion
Findings from this study of truck drivers and helpers who transited through Hyderabad city indicated that exposure to HIV prevention programmes was low with less than one-twelfth of the participants reporting a contact made with HIV prevention intervention ever. Despite this low contact, the willingness for new HIV interventions introduced in this study was significantly high among the study population except for circumcision.
The results of this study may not be generalizable to truckers all over India, but the relatively large sample size of the study conducted on truckers passing through in a large city in southern India suggest that the findings are likely to be applicable to a large proportion of truckers either living or passing through southern India.
HIV prevention services for truckers in India are provided by NACO through a large number of organizations at the State and district levels. It is estimated that nearly 60 per cent of this high-risk group needing targeted interventions is covered by the NACO interventions through over 100 non-governmental organisations (NGOs) providing HIV prevention services19. In our study, it was found that only 7.9 per cent truckers reported being contacted at least once by a person/NGO staff providing HIV prevention interventions, among whom the majority reported only one contact in their lifetime. We have previously reported from this State that the annual contacts of truckers with public funded HIV prevention programmes was grossly inadequate to yield desired and sustained HIV intervention impact8. A recent study of targeted intervention, Avahan, among long distance truck drivers showed the non-exposure to any intervention ranging from 36 to 63 per cent along the four routes where the intervention was active with the exposure to HIV interventions being the lowest on south-east route11. However, the HIV intervention coverage between our study and this study is not directly comparable as the latter considered only truck drivers and they were recruited from transshipment locations covering the bulk of India's transport volume along the four routes where the intervention was active. Findings from this study and that from the Avahan study highlight that truckers in contact with prevention programmes are likely to have a lower risk behaviour as compared to those who did not, thereby, highlighting that it would be useful for the contacts and coverage to increase to reduce risk behaviour in this population. In the background of scaling up of HIV prevention being one of the most important priority for control of the HIV epidemic, the gap between the intent of targeted HIV prevention strategies and their actual coverage warrants for an urgent need for scaling up of preventive measures in this population group in India.
In this study, the truckers who had reported contact ever with HIV intervention were significantly less likely to have FSW as their last sex partner than those who did not and they were also more likely to have undergone HIV test previously. These findings suggest the beneficial effect of intervention programmes, and further stress the need for increased reach and intensity of these programmes specifically tailored for them11. We have previously estimated that the cost per DALY (disability-adjusted life year) saved from the averted HIV infections from HIV prevention interventions targeted at truckers in Andhra Pradesh was  27.4 which is much lower than the per capita gross domestic product in Andhra Pradesh suggesting that such a programme was cost-effective7. A recent report on assessment of population level effect of Avahan initiative in India has revealed a strong beneficial association between well-planned and managed large-scale HIV prevention programmes and reduction in HIV prevalence at the population level also20.
27.4 which is much lower than the per capita gross domestic product in Andhra Pradesh suggesting that such a programme was cost-effective7. A recent report on assessment of population level effect of Avahan initiative in India has revealed a strong beneficial association between well-planned and managed large-scale HIV prevention programmes and reduction in HIV prevalence at the population level also20.
The overall prevalence of HIV was 2.8 per cent, HSV was 13.4 per cent and of syphilis was 3.7 per cent in the population studied. Similar HIV prevalence was reported among truck drivers from a recent evaluation of Avahan11, and a relatively high HIV and STI prevalence among truck drivers in India than reported in this study has been reported previously1352122, however, several of these studies did not use a systematic approach to sample generation.
We documented likelihood of acceptance for four novel HIV prevention and control methods in this study population. Our results indicated high levels of likelihood of acceptance of oral rapid HIV testing, medications for HIV prophylaxis, and telephonic counselling for HIV. However, circumcision as a tool of HIV prevention was not found to be acceptable with less than 10 per cent of participants likely to consider circumcision. It is likely that some respondents may change their willingness after having opportunity to reflect on these interventions post interview, however, this is beyond the scope of this study.
Acceptance for oral HIV testing was very high (97%). This is an encouraging finding given the low numbers of having undergone previous HIV test (19%) reported by the study participants. In India, oral testing has not yet been used in non-clinical settings and in populations at high-risk for HIV such as truckers. Studies among FSW clients in clinical setting in India have demonstrated preference of oral testing over blood sample collection methods in part due to the reduction in pain and anxiety with the former2324. With such low rates of HIV testing among truckers, it is possible that oral testing for HIV could increase testing rates even in non-clinical settings242526 including mobile clinics which are used to contact the hard-to-reach populations in field settings. Furthermore, oral tests allow patients to receive their test results much faster than traditional technique and thus can significantly lower the chances of losing the patients to follow-up27.
With regards toPrEP, the study participants expressed a high degree of likelihood to get more information, obtain this if provided free of cost, and to discuss with friends about it. This is in contrast to a recent study using the AIDS risk reduction model which demonstrated that truck drivers in India exhibited low levels of initial commitment towards PrEP. The same study also indicated that cost was a major barrier to initial commitment for PrEP22. In a cohort of men who have sex with men, cost was a significant predictor of intent-to-use PrEP with not having to pay for PrEP as one of four statistically significant predictors of this initial commitment28. Interestingly, about three quarters of the participants in this study were likely to pay for PrEP, however, this finding will have to be interpreted with caution as the respondents were not informed of PrEP cost. With limited studies on initial commitment to PrEP and its effectiveness in India, our findings provide useful insights regarding its acceptance as potential future HIV prevention strategy, although analyses of funding and cost-effectiveness will be required.
Circumcision has been shown to decrease the risk of HIV acquisition in men by 50-60 per cent in randomized controlled trials from Africa293031. Circumcision may be a potential candidate for mobile populations such as truckers who are at an increased risk of HIV acquisition, however, less than 10 per cent of those not circumcised in this study were likely to consider circumcision as a method for HIV prevention. Truckers parking trucks at dhabas more frequently and those who reported having sex with men were more likely to consider circumcision. Given that majority of participants were Hindus, social-cultural and religious norms could have an effect on their preferences to obtain circumcision. Our findings were similar to a previously published report on initial commitment to circumcision in Indian truck drivers22.
Feasibility of telephonic counselling for HIV was assessed for those participants who reported possession of a mobile phone in this study. The results indicated that a substantial proportion was likely to consider discussing sensitive or personal health information over phone with a doctor or health care provider and also preferred receiving HIV test results over phone. Telephonic counselling could, much like oral testing, help ensure that mobile populations receive their results by reducing the need for clients to make multiple trips to the testing site. In other mobile populations, clients who are offered telephonic follow up have been found to be significantly more likely to receive their results and post-test counselling than those who are only offered face-to-face notification3233. Telephonic counselling methods have undergone limited study in India1034 and our findings encourage the possible use of a mobile phone as a tool in disseminating HIV prevention information among this hard to reach mobile population.
In general, truckers with dhabas as their regular halt point showed less risk behaviour for HIV and more willingness for novel interventions. Dhabas are eating and resting joints mostly catering to truckers on highways. Increasingly, these dhabas are participating in HIV prevention activities thereby increasing the chances of truckers being in contact with intervention programmes, and often the dhaba owners are peer-educators for such programmes3536.
In conclusion, HIV prevalence rates have remained low in India with high prevalence among high-risk and vulnerable groups including truckers. Therefore, prevention measures targeting this group are crucial. Our findings suggest that there exists a wide gap between the intent of targeted HIV prevention strategies for truckers and existing exposure of truckers to interventions, indicating the need to find ways of reaching a higher proportion of truckers with HIV prevention interventions. These preliminary data indicate a high level of willingness and interest for new HIV prevention interventions which could be utilized to explore further feasibility of these in this population. With the transport sector being an integral part of economic growth and access to HIV treatment still low, planning for the next phase of HIV/AIDS control in India could utilize these findings to design appropriate prevention packages for this high-risk and vulnerable mobile population.
Acknowledgment
This study was funded by a Grant (P30AI042853) from the National Institutes of Health, USA. The views expressed in this paper are those of the authors and do not necessarily reflect the views of the funding agency, organisations that facilitated this study, or the institutions employing the authors.
References
- Risk behavior, sexually transmitted infections and HIV among long-distance truck drivers: a cross-sectional survey along national highways in India. AIDS. 2008;22(Suppl 5):S81-S90.
- [Google Scholar]
- A study of knowledge, sexual behaviour and practices regarding HIV/AIDS among long distance truck drivers. Indian J Public Health. 2009;53:243-5.
- [Google Scholar]
- Sexual behaviour among long distance truck drivers. Indian J Community Med. 2006;31:153-6.
- [Google Scholar]
- Technical report: India HIV estimates 2006. New Delhi: National Institute of Medical Statistics and National AIDS Control Organization; 2007.
- [Google Scholar]
- A population-based study of human immunodeficiency virus in south India reveals major differences from sentinel surveillance-based estimates. BMC Med. 2006;4:31.
- [Google Scholar]
- Economic analysis of HIV prevention interventions in Andhra Pradesh state of India to inform resource allocation. AIDS. 2009;23:233-42.
- [Google Scholar]
- Cost-effectiveness of HIV prevention interventions in Andhra Pradesh state of India. BMC Health Serv Res. 2010;10:117.
- [Google Scholar]
- Outputs and cost of HIV prevention programmes for truck drivers in Andhra Pradesh, India. BMC Health Serv Res. 2009;9:82.
- [Google Scholar]
- General hygiene, sexual risk behaviour and HIV prevalence in truck drivers from Andhra Pradesh, South India: implications for prevention interventions. Int J STD AIDS. 2009;20:39-45.
- [Google Scholar]
- Using digital communication technology fails to improve longitudinal evaluation of an HIV Prevention Program aimed at indian truck drivers and cleaners. AIDS Behav. 2012;16:1359-63.
- [Google Scholar]
- Heading towards the safer highways: an assessment of the Avahan prevention programme among long distance truck drivers in India. BMC Public Health. 2011;11(Suppl 6):S15.
- [Google Scholar]
- National AIDS Control Organization. HIV data. New Delhi: Ministry of Health and Family Welfare, Government of India; Available from: http://www.nacoonline.org/Quick_Links/HIV_Data
- [Google Scholar]
- Novel HIV prevention strategies: the case for Andhra Pradesh. Indian J Med Microbiol. 2008;26:1-4.
- [Google Scholar]
- Modeling interventions to assess HIV epidemic impact in Africa. J Acquir Immune Defic Syndr. 2011;58:121-4.
- [Google Scholar]
- Replacement of conventional HIV testing with rapid testing: mathematical modelling to predict the impact on further HIV transmission between men. Sex Transm Infect. 2011;87:588-93.
- [Google Scholar]
- Risk factors associated with HIV in a population-based study in Andhra Pradesh state of India. Int J Epidemiol. 2008;37:1274-86.
- [Google Scholar]
- Department of Road Transport and Highways (DRTH), Goverment of India. In: The Central Motor Vehicles Rules. New Delhi, India: DRTH; 1989.
- [Google Scholar]
- Closing the loop: physician communication with diabetic patients who have low health literacy. Arch Intern Med. 2003;163:83-90.
- [Google Scholar]
- National AIDS Control Programme: Response to the HIV epidemic in India. New Delhi: NACO; 2007.
- [Google Scholar]
- Assessment of population-level effect of Avahan, an HIV-prevention initiative in India. Lancet. 2011;378:1643-52.
- [Google Scholar]
- Containing HIV/AIDS in India: the unfinished agenda. Lancet Infect Dis. 2006;6:508-21.
- [Google Scholar]
- Initial commitment to pre-exposure prophylaxis and circumcision for HIV prevention amongst Indian truck drivers. PLoS One. 2010;5:e11922.
- [Google Scholar]
- Impact of round-the-clock, rapid oral fluid HIV testing of women in labor in rural India. PLoS Med. 2008;5:e92.
- [Google Scholar]
- Rapid oral fluid-based point-of-care HIV testing: applicability in developing countries. Indian J Med Res. 2007;126:171-3.
- [Google Scholar]
- Australian men who have sex with men prefer rapid oral HIV testing over conventional blood testing for HIV. Int J STD AIDS. 2010;21:428-30.
- [Google Scholar]
- Choosing HIV counseling and testing strategies for outreach settings: A randomized trial. J Acquir Immune Defic Syndr. 2005;38:348-55.
- [Google Scholar]
- Rapid HIV testing of clients of a mobile STD/HIV clinic. AIDS Patient Care STDs. 2005;19:253-7.
- [Google Scholar]
- Pre-exposure antiretroviral prophylaxis attitudes in high-risk Boston area men who report having sex with men: limited knowledge and experience but potential for increased utilization after education. J Acquir Immune Defic Syndr. 2009;50:77-83.
- [Google Scholar]
- Male circumcision for HIV prevention in young men in Kisumu, Kenya: a randomised controlled trial. Lancet. 2007;369:643-56.
- [Google Scholar]
- Male circumcision for HIV prevention in men in Rakai, Uganda: a randomised trial. Lancet. 2007;369:657-66.
- [Google Scholar]
- Joint strategic action framework to accelerate the scale-up of voluntary medical male circumcision for HIV prevention in Eastern and Southern Africa. 2012-2016. 2011. Available from: www.who.int/hiv/pub/strategic-action-2012-2016/en/index.html
- [Google Scholar]
- A meta-analysis of the effectiveness of alternative HIV counseling and testing methods to increase knowledge of HIV status. AIDS. 2006;20:1597-604.
- [Google Scholar]
- Telephone notification of HIV test results: impact in King County, Washington. Sex Transm Dis. 2007;34:796-800.
- [Google Scholar]
- Design of a randomized trial to evaluate the influence of mobile phone reminders on adherence to first line antiretroviral treatment in South India - the HIVIND study protocol. BMC Med Res Methodol. 2010;10:25.
- [Google Scholar]
- NACO to supply condoms dhabas, auto workshops and barber shops to prevent HIV/AIDS in Indian villagers. Available from: http://www.dancewithshadows.com/pillscribe/naco-tosupply-condoms-dhabas-auto-workshops-and-barber-shopsto-prevent-hivaids-in-indian-villagers
- [Google Scholar]
- Truckers turn teachers, dhabas schools for HIV classes. Available from: http://ibnlive.in.com/news/truckers-turnteachers-dhabas-schools-for-hiv-classes/50088-3.html
- [Google Scholar]






