Translate this page into:
Consensus recommendations for acute trauma care & outcomes in LMICs from the transdisciplinary research, advocacy & implementation network for trauma in India
For correspondence: Dr Nakul P. Raykar, Department of Trauma and Emergency Surgery, Brigham and Women’s Hospital, Boston, Massachusetts 02115, USA e-mail: nraykar@bwh.harvard.edu
-
Received: ,
Abstract
Background & objectives
Injuries profoundly impact global health, with substantial deaths and disabilities, especially in low- and middle-income countries (LMICs). This paper presents strategic consensus from the Transdisciplinary Research, Advocacy, and Implementation Network for Trauma in India (TRAIN Trauma India) symposium, advocating for enhanced, system-level trauma care to address this challenge.
Methods
Five working groups conducted separate literature reviews on pre-hospital trauma care, in-hospital trauma resuscitation and training, trauma systems, trauma registries, and India’s Towards Improving Trauma Care Outcomes (TITCO) registry. Using a Delphi approach, the TRAIN Trauma India Symposium generated consensus statements and recommendations for interventions to streamline trauma care and reduce preventable trauma mortality in India and LMICs. Experts prioritized interventions based on cost and difficulty.
Results
An expert panel agreed on four pre-hospital consensus statements, eight hospital resuscitation consensus statements, six system-level consensus statements, and six trauma registry consensus statements. The expert panel recommended six pre-hospital interventions, four hospital resuscitation interventions, nine system-level interventions, and seven trauma registry interventions applicable to the Indian context. Of these, 14 interventions were ranked as low cost/low difficulty, five high cost/low difficulty, five low cost/high difficulty, and three high cost/high difficulty.
Interpretation & conclusions
This consensus underscores the urgent need for integrated and efficient trauma systems to reduce preventable mortality, emphasizing the importance of comprehensive care that includes community engagement and robust pre-hospital and acute hospital trauma care pathways. It highlights the critical role of inclusive, system-wide approaches, from enhancing pre-hospital care and in-hospital resuscitation to implementing effective trauma registries to improve outcomes and streamline care across contexts.
Keywords
Consensus statement
injury
pre-hospital trauma care
trauma care
trauma registries
trauma resuscitation
trauma surgery
trauma system
Injuries represent a significant challenge in global health, affecting lives and economies worldwide. They result in about 247.6 million Disability-Adjusted Life Years (DALYs) and cause 4.8 million deaths annually1. Before the pandemic, the World Health Organisation (WHO) reported that injuries, including accidents and violence, contributed to eight per cent of the total global deaths2. Road traffic injuries (RTIs) stand out, causing around 1.15 million deaths each year; with 90 per cent of these occurring in low- and middle-income countries (LMICs)3-8. These injuries not only end lives; but also cause long-term disabilities and impose economic burden due to healthcare expenses and lost productivity2,3.
In India, trauma significantly impacts public health, with the country contributing to over 20 per cent of the global trauma-related deaths. This makes injuries a significant public health issue9-14. According to the Towards Improved Trauma Care Outcomes (TITCO) registry data, the mortality rate among admitted individuals was 21.4 per cent between September 2013 and February 201515. Additionally, while the latest report from WHO3 indicates a global decrease of around five per cent in total RTI fatalities in 2021 compared to 2010, India, conversely, has experienced an 18 per cent increase in fatality rates during the same period16.
Furthermore, enhancing trauma care systems is recognized as a critical intervention. It aligns with the second UN Decade of Action for Road Safety priorities, focusing on post-crash care. This approach is also vital in achieving the Sustainable Development Goals (SDGs) targets, particularly as we surpass the halfway mark of the SDG timeline, underlining the urgent need for action in reducing road traffic injuries and fatalities17,18. It is estimated that over 200,000 lives can be saved every year globally with the implementation of a complete trauma system globally with 100 per cent coverage in LMICs18. However, there is a significant scarcity of scholarly research on the fundamental mechanisms required for establishing resilient trauma systems in LMICs. Effective trauma treatment necessitates a comprehensive and interdisciplinary strategy involving diverse stakeholders across all stages of care, from initial stabilization in the pre-hospital setting to rehabilitation post-discharge18.
The Transdisciplinary Research, Action, and Implementation Network for Trauma in India (TRAIN Trauma India) Symposium was organized to address these challenges. This event gathered a group of experts at the All India Institute of Medical Sciences (AIIMS), New Delhi, to discuss the current state, assess existing best practices, and explore future directions for research and intervention in trauma management using a system-level approach. This manuscript presents the consensus statement from the symposium, focusing on system-level context, pre-hospital resuscitation and transport, initial hospital resuscitation, and trauma registries to identify priorities for interventions that can streamline trauma care and efficiently reduce preventable mortality across contexts.
Material & Methods
Scoping review
Eight months before the symposium, a steering committee of faculty leadership was established, and five working groups were established by the steering committee, each focusing on defining the current state of trauma care in a specific context under the oversight of the steering committee (Fig. 1). Through scoping literature reviews conducted by the individual working groups followed by a Delphi consensus method, this symposium aimed to comprehensively examine the current state of trauma care across diverse contexts, focusing on the various components within trauma systems.
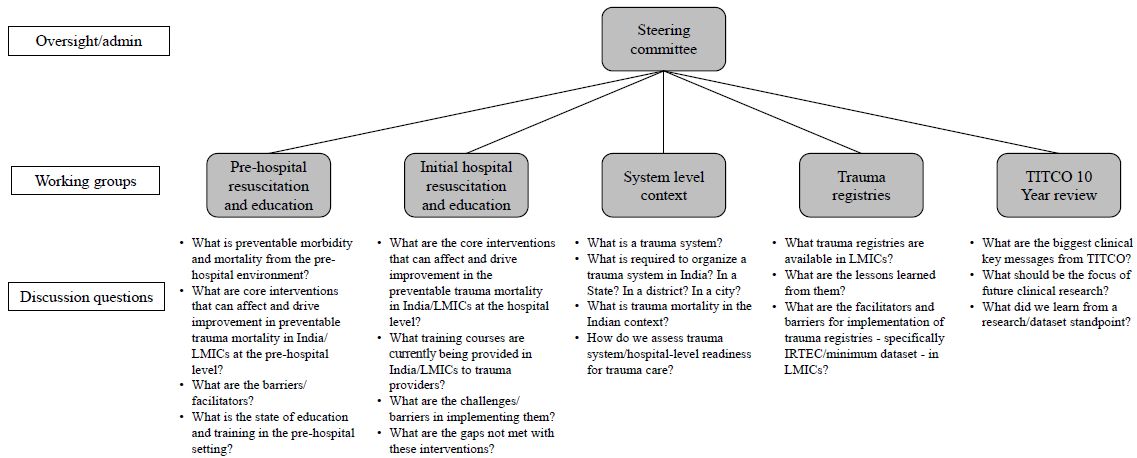
- Summary of working groups for the TRAIN Trauma India Symposium and key questions addressed by each working group. TITCO, towards improved trauma care outcomes; IRTEC, international registry for trauma and emergency care; LMICs, low-and middle-income countries.
Delphi consensus approach was employed to synthesize the output of these working groups and generate a consensus on interventions applicable to the Indian trauma system.
TRAIN trauma India symposium
A trauma symposium was organized in New Delhi from September 30 to October 1, 2023. Experts in trauma care from various disciplines and phases of the patient care continuum were invited.
The symposium saw representation from multiple institutions in trauma surgery, including experts from academic centres across India, as well as a multidisciplinary, multinational global health team with a longstanding history of collaboration in India. Surgeons in attendance represented rural and urban contexts, spanning levels of care from primary to tertiary hospitals. Disciplines represented at the conference included surgery, emergency medicine, anaesthesia, radiology, nursing, patient advocates, policymakers, and representatives from international non-governmental organizations (NGOs).
On the symposium’s first day, they featured presentations of findings from the working groups. A summary of the identified interventions through the literature review was presented to the panel of experts and stakeholders for discussion regarding their applicability in the Indian context, emphasizing feasibility in LMIC regions of the country. Stakeholder discussions were facilitated after each working group presentation, allowing input from multidisciplinary stakeholders.
Steering committee discussions
A list of consensus statements was generated based on topics that emerged during discussions, and a list of proposed interventions was compiled from the working group presentations. The consensus statements and interventions were coded by a panel of six researchers for recurring themes before the second day of the symposium. On the second day, a collated list of recurring themes from consensus statements and the recommended interventions was presented to the expert panel for further discussion and clarification of those relevant to India and LMICs. Of note, no statements were excluded at this stage, but the wording on some statements was adjusted slightly in response to the panellists’ recommendations.
Evaluation of consensus statements
The refined statements and interventions were sent to the expert attendees following the symposium to verify consensus statements and vote on the classification of the interventions according to cost and difficulty of implementation. To prioritize interventions, each attendee classified each intervention as either low cost or high cost and low difficulty or high difficulty. Of the expert panel, seven people participated in the classification of the interventions by cost and difficulty. Based on these votes, a visual representation of these classifications was created as a graph with consensus strength for cost on the x-axis and difficulty on the y-axis. Votes for low cost were assigned a weight of –1, while high cost received a weight of +1. Similarly, responses indicating low difficulty were given a weight of –1, and high difficulty received a +1. The average of the votes determined the consensus strength on cost and difficulty.
Results
Overall, there were four pre-hospital consensus statements, eight hospital resuscitation consensus statements, six system-level consensus statements, and six trauma registry consensus statements. The expert panel reached a consensus on seven pre-hospital interventions, four hospital resuscitation interventions, nine system-level interventions, and seven trauma registry interventions applicable to the Indian context. These interventions were categorized by cost and difficulty and presented for each subgroup. A total of 14 interventions were ranked as low cost/low difficulty, five high cost/low difficulty, five low cost/high difficulty, and three high cost/high difficulty.
Pre-hospital resuscitation and education
The expert panel noted that recognizing and replicating context-specific pre-hospital best practices is imperative for optimizing trauma care. Sustained and repeated pre-hospital training is crucial for maximizing knowledge retention. Collaborative partnerships with nonmedical transport personnel enhance the overall trauma response, and the role of the trauma centre extends beyond immediate care to promote community involvement in trauma care and efforts related to injury prevention through outreach initiatives.
The expert panel reviewed previous pre-hospital interventions synthesized by the pre-hospital resuscitation and education working group and agreed on seven interventions applicable to the Indian context (Supplementary Material: Box 1). The interventions were classified according to cost and difficulty, with five interventions rated as low cost/low difficulty, one low cost/high difficulty, and one high cost/high difficulty (Fig. 2).
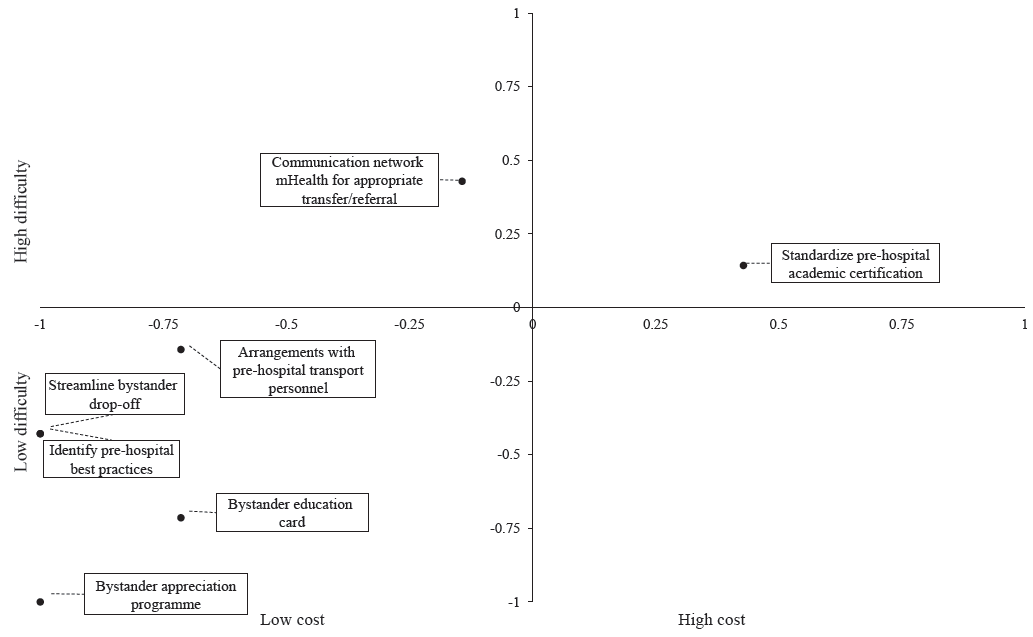
- Chart of proposed pre-hospital resuscitation and education interventions classified by cost and difficulty. The x- and y-axis values represent the strength of consensus on whether the intervention was high or low price or difficulty. Greater absolute value indicates more substantial consensus. Values do not reflect the level of cost or difficulty beyond the binary classification of low or high, as given by negative or positive values, respectively. mHealth, mobile health.
Initial hospital resuscitation
The expert panel noted that real-world, context-appropriate grounding is essential to trauma training. High-quality trauma education requires incorporating practical, skill-based experiences with continual assessments to ensure the effectiveness of training programmes. High-quality trauma training begins with committed clinician educators integrating education and bedside learning. Standardized, high-quality trauma courses, such as National Emergency Life Support (NELS) and Advanced Trauma Life Support (ATLS), provide scalability across multiple contexts. Integrating modern diagnostic tools, such as ultrasound, is a critical aspect of training in contexts where it is available. Point-of-care ultrasound is an essential component of emergency evaluation. It must be integrated into training and clinical pathways for all trauma team members and not limited to physicians alone. Team members that comprise the trauma team may vary by context. As such, inclusion and empowerment of the entire trauma team are essential and can be accomplished through a framework of customization of training, its optimization, strengthening, and further integration. Finally, sustainable and replicable training efforts in diverse contexts will require a combination of grassroots and centralized initiatives.
The expert panel reviewed previous interventions in the hospital resuscitation space as synthesised by the initial hospital resuscitation and education working group and agreed on four interventions that apply to the Indian context (Supplementary Material: Box 2). The interventions were classified according to cost and difficulty, with one intervention rated low cost/low difficulty and three high cost/low difficulty (Fig. 3).
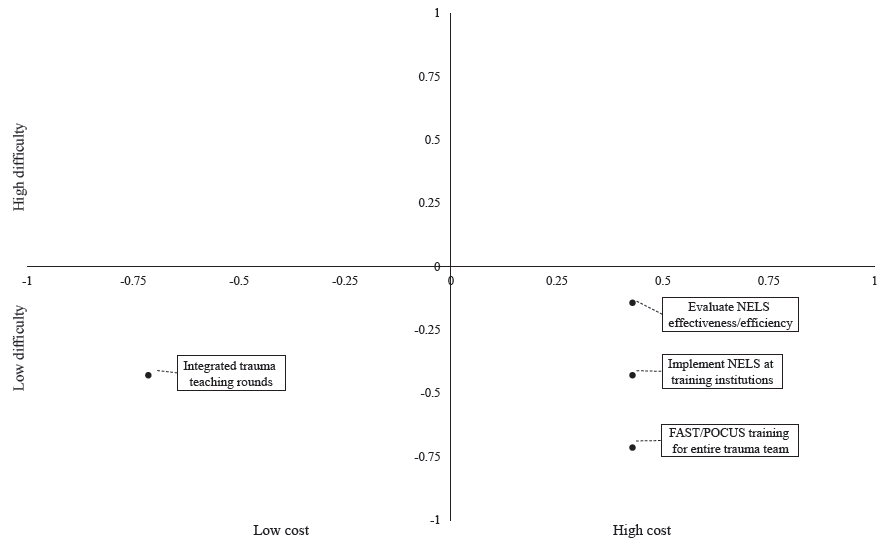
- Chart of proposed initial hospital resuscitation and education interventions classified by cost and difficulty. The x- and y-axis values represent the strength of consensus on whether the intervention was high or low price or difficulty. Greater absolute value indicates more substantial consensus. Values do not reflect the level of cost or difficulty beyond the binary classification of low or high, as given by negative or positive values, respectively. NELS, national emergency life support; FAST, focussed assessment with sonography trauma; POCUS, point-of-care.
System level context
A systems approach to improve trauma outcomes begins with solid leadership and acknowledging that outcome improvement is possible in any environment despite specific challenges. Trauma care designation should be extended to existing facilities after evaluating their trauma care capabilities and services; regular re-verification is essential to ensure the maintenance of established standards of care. Morbidity and mortality reviews are crucial in advancing trauma care, and institutional review of preventable mortality is indispensable for any quality improvement programme. Inter facility referral and transfer systems should be based on physician-to-physician communication, rooted in a culture of collegiality and shared goals of optimized patient care between referring and accepting facilities. Trauma care should prioritize patient welfare while mitigating the risk of catastrophic or impoverishing expenditures for patients. Finally, data-driven strategies can guide governmental commissions toward interventions that maximize the lives saved; hence, data collection should be prioritized.
The expert panel reviewed previous interventions in the trauma systems space synthesized by the System Level Context working group and agreed on nine interventions applicable to the Indian context (Supplementary Material: Box 3). The interventions were classified according to cost and difficulty, with three interventions being rated as low cost/low difficulty, four low cost/high difficulty, and two high cost/high difficulty (Fig. 4).
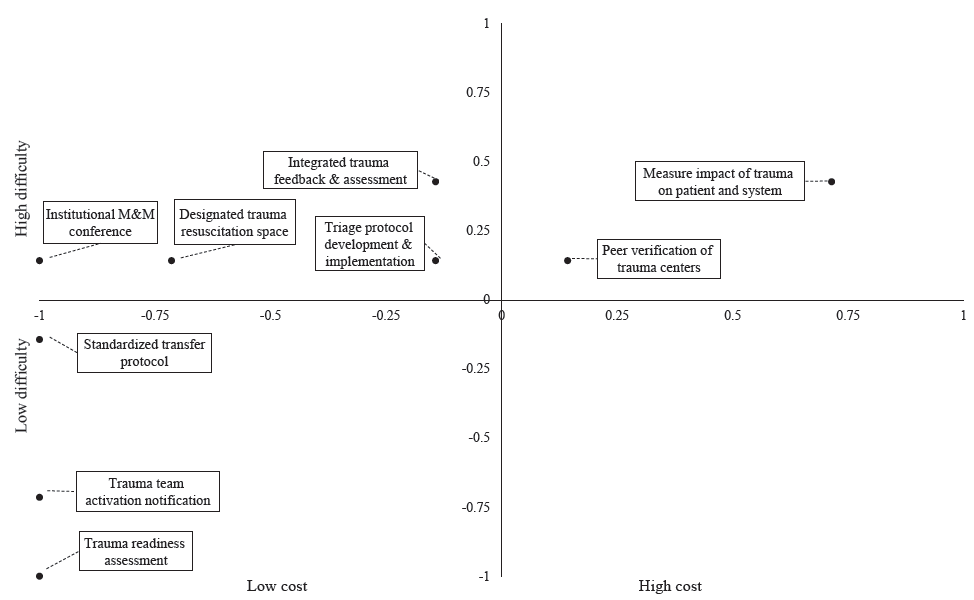
- Chart of proposed trauma system-level interventions classified by cost and difficulty. The x- and y-axis values represent the strength of consensus on whether the intervention was high or low cost or difficulty. Greater absolute value indicates stronger consensus. Values do not reflect the level of expense or difficulty beyond the binary classification of low or high, as given by negative or positive values, respectively. M&M, morbidity & mortality.
Trauma registries
The expert panel reached the following points of consensus on the role of trauma registries. Firstly, as in all clinical medicine, interventions and therapies must be evaluated against real-world effectiveness; high-quality data collection plays a central role in constructing evidence to substantiate existing interventions’ effectiveness and guide further dissemination and implementation efforts. The value of data lies in its actionable insights; however, the data collected by current registries worldwide and within India may not be actionable. This limitation arises because data from one context cannot reliably be compared to a different context, such as urban versus rural or international settings, without consistency in data elements and processes. Nevertheless, prioritizing using available imperfect data sufficient to drive local improvements is recommended over pursuing perfect data collection. Nonetheless, the role of future implementation research is crucial. These efforts aim to provide feedback on existing interventions and improve current data collection models. Trauma registries, if implemented effectively, have the potential to enhance care, cost-effectiveness, and planning. A standardized and inexpensive registry platform is emphasized as it can facilitate the collection of high-quality, actionable data, ensuring the sustainability of existing interventions.
The expert panel reviewed previous interventions involving trauma registries as synthesized by the TITCO 10 Year Review working group and the Trauma Registries working group and agreed on seven interventions that apply to the Indian context (Supplementary Material: Box 4). The interventions were classified according to cost and difficulty, with five interventions rated low cost/low difficulty and two high cost/low difficulty (Fig. 5).
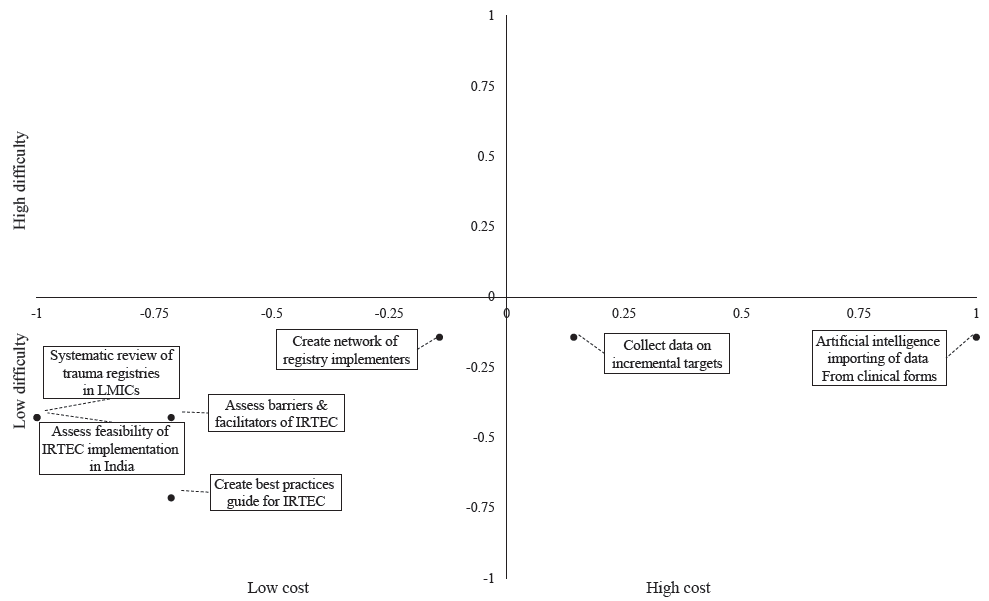
- Chart of proposed initial trauma registry interventions classified by cost and difficulty. The x- and y- axis values represent the strength of consensus on whether the intervention was high or low cost or difficulty. Greater absolute value indicates stronger consensus. Values do not reflect the level of cost or difficulty beyond the binary classification of low or high, as given by negative or positive values, respectively
Discussion
The urgency of establishing effective trauma systems is underscored by their role in reducing preventable deaths, particularly as trauma remains the leading cause of death among younger populations7,8. These recommendations represent a consensus among diverse stakeholders focused on trauma care in India, highlighting the need for comprehensive strategies that encompass community engagement, inclusive leadership, and a patient-centred approach19-21.
An effective trauma system is a complex network of components that must function harmoniously to ensure optimal patient outcomes20,22. If a robust in-hospital trauma care system does not accompany an advanced pre-hospital system, the burden of morbidity and mortality may shift from the pre-hospital to in-hospital settings20. If strong inpatient care is not complemented with high-quality post-discharge follow up and rehabilitation and financial support mechanisms, patients will leave the hospital disabled, isolated, and destitute. A trauma system should always focus on improving patient outcomes, necessitating balanced development across all its elements (Fig. 6).
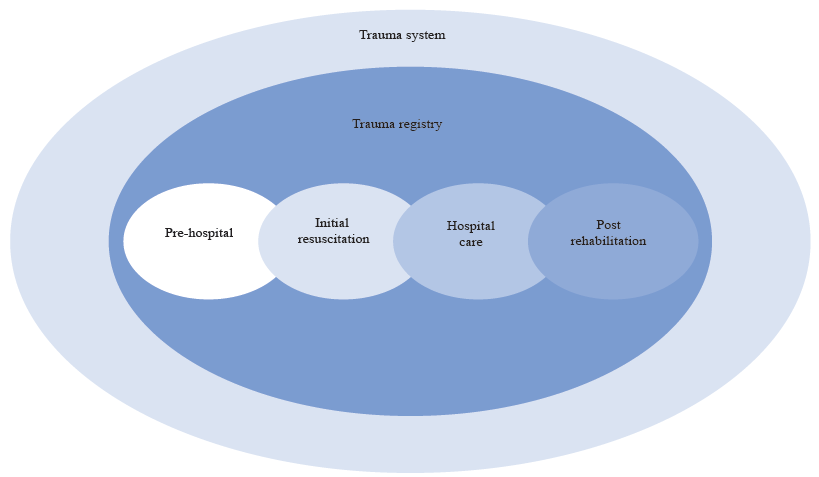
- Schematic depiction of a trauma system illustrating the interactions between system elements, including pre-hospital care, acute hospital treatment, and post-discharge rehabilitation.
Pre-hospital resuscitation and education
Pre-hospital trauma care optimization in resource-limited settings can be achieved by standardizing training, enhancing transfer communication, and utilizing a bystander approach20,21,23. These trauma care systems face challenges such as limited pre-hospital transport vehicles, workforce training, minimal coordination between pre-hospital providers, and scant interpersonal communication within the hospital systems20,21,24. High costs associated with these systems also limit their applicability, posing challenges in accessibility and cost-effectiveness21,24.
Despite these challenges, viable, low-cost interventions exist, focusing on leveraging existing infrastructure and local resources21,24. Programmes like SaveLIFE Foundation’s police bystander training and “Stop the Bleed” civilian bystander training demonstrate how public and non-medical involvement in pre-hospital care can be effective and resource-efficient21,22,25.
This consensus group emphasizes the importance of making it easier for bystanders to provide help and removing barriers often erected by medical and legal systems. Protecting civilian “Good Samaritans” from medicolegal harassment is an essential first step with additional mechanisms for recourse necessary. Hospital systems should protect and celebrate “Good Samaritans”21,25,26.
Standardizing and strengthening pre-hospital training programmes for individuals already serving as pre-hospital caretakers is imperative. Governments should partner with hospitals and academic institutions to establish iterative training opportunities. Establishment of efficient pre-hospital notification systems for transfers, including formal communications and well-publicized contact numbers of triage personnel at the receiving facility are vital. Creating platforms for seamless communication among providers foster responsibility, effective transfers, and partnerships pre-hospital and hospital providers.
In-hospital resuscitation and trauma training
The aetiology of in-hospital trauma mortality is multifaceted, involving patient physiology, timeliness of care, and systemic healthcare issues. However many in-hospital deaths can be averted through timely, coordinated, and skilled interventions focused on optimizing airway, breathing, and circulation20,27. The performance of hospital trauma teams is integral to optimizing outcomes for seriously injured patients24,28,29. In HICs, this is achieved through rapid response mechanisms, clear protocols, and effective team communications24,28,29. Adapting these systems to the diverse contexts of LMICs is challenging but necessary, relying heavily on high-quality training programmes24,28-30.
Trauma training programmes in LMICs are often characterized by high costs, uncertain effectiveness, limited follow up, and poor integration within local care paradigms31,32. The NELS training, launched by the Ministry of Health and Family Welfare of India in 2022, offers a platform for standardized trauma team training, role definitions, streamlined action flows, and cohesive team dynamics during emergency resuscitations33. Expanding this training to include essential diagnostic tools, such as point-of-care ultrasound, for a diverse range of team members, including nurses, medical assistants, and other non-physician clinicians, could significantly improve patient outcomes. Training must be standardized and contextually adapted with regular efficacy audits and assessments, including video reviews of trauma resuscitations and human patient simulators28.
Systems level evaluation - assessments and trauma centre verifications
High-quality trauma team training is essential, but mature trauma systems also require mechanisms to efficiently bring severely injured patients into facilities ready to provide trauma care. This includes efficient triage upon arrival, rapid mobilization of trauma teams and continuous feedback and performance reviews, including morbidity and mortality reviews at the clinical and system levels, for process improvements.
Several studies highlight the benefits of mature trauma systems and caution against blindly implementing these aspects in LMICs but, there is a continuous lack of a centralized, integrated, organized, and holistic trauma care system in India9,11,18,34,35. The first step should be a comprehensive assessment of existing infrastructure, workforce, workflow processes, and system performance. These assessments should be part of a longitudinal implementation framework, integrated into a continuous quality improvement strategy with existing or adequately funded data collection mechanisms.
In the long term, trauma system assessments must be integrated into broader facility assessments to minimize burdens on facilities and healthcare providers18-21, 24. Peer verification of hospitals’ capacity to provide trauma care based on objective performance measures and process capabilities should supersede arbitrary designations or the development of de novo facilities labelled as ‘trauma centres.’ Finally, a patient-centred perspective is vital, focusing on patient’s experience, interactions with the trauma system, and addressing inefficiencies from their viewpoint24,36. Patient-centred care, defined by transparency, individualization, respect, dignity, and choice, is quintessential, especially in high-stress trauma settings20,23,36. Time-series assessments of patient flow through trauma centres can provide insights for system optimizations and effectiveness, ensuring ongoing feedback and improvement.
Information systems and trauma registries
Trauma registries are essential for improving trauma care31,32,37 particularly in LMICs, but they face implementation challenges due to significant disease burdens37-39. Furthermore, these include high initiation and maintenance costs, poor communication between systems, and incomplete data collection and limited analytic capacity38,40.
Standardizing data collection and management practices, with simplified and complete data capture integrated into broader health information systems, can improve the situation11,18,32. Global collaboration and resource sharing between centres with established trauma registries and those developing them are crucial, along with workforce training for data collection and analyses18,35,41,42.
Our group consensus emphasises the need for an affordable and reliable registry with a minimum dataset. The WHO International Registry for Trauma and Emergency Care (IRTEC) could be a viable solution for LMICs, offering training, data maintenance, storage, and analysis support. Additionally, artificial intelligence (AI) and Large Language Models (LLMs), have the potential to reduce data collection costs by automating tasks like importing and analyzing images.
This study was not without some limitations. First, it did not encompass trauma prevention or post-hospital rehabilitation and follow up focusing instead on immediate and acute care aspects. However, preventive strategies to reduce trauma incidence and severity and comprehensive care inclusive of post-hospital rehabilitation and follow up are vital for the holistic recovery of trauma patients. These are critical components of a complete trauma care system and warrant attention in future deliberations.
Our classification of interventions based on cost and difficulty was subjective, reflecting the expert panel’s opinions. Given India’s diversity, it is challenging to represent all regional and hospital-level contexts. Thus, while the symposium’s recommendations aim to be broadly applicable, future implementation should evaluate context-specific barriers and facilitators to ensure feasibility and applicability. Developing and implementing trauma care systems necessitate a balanced approach, considering resource allocation, stakeholder engagement, and continuous evaluation. Focusing on these aspects can help trauma care systems evolve to meet the needs of patients and communities, leading to better recovery outcomes.
Financial support & sponsorship
The symposium was funded by Rick and Sadhana Downs Foundation and Boston Children’s Hospital, Boston, MA 02115 (Project Number: 010-1184-302)
Conflicts of Interest
None.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that no AI- assisted technology was used to assist in the writing of the manuscript, and no images were manipulated using AI.
References
- The global burden of injury: incidence, mortality, disability-adjusted life years and time trends from the global burden of disease study 2013. Inj Prev. 2016;22:3-18.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Injuries and violence. Available from: https://www.who.int/news-room/fact-sheets/detail/injuries-and-violence, accessed on April 5, 2024.
- Global status report on road safety 2023. Available from: https://www.who.int/teams/social-determinants-of-health/safety-and-mobility/global-status-report-on-road-safety-2023, accessed on April 5, 2024.
- Global, regional, and national disability-adjusted life years (DALYs) for 306 diseases and injuries and healthy life expectancy (HALE) for 188 countries, 1990-2013: Quantifying the epidemiological transition. Lancet. 2015;386:2145-91.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Injuries: The neglected burden in developing countries. Bull World Health Organ. 2009;87:246.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Murray JLC, Lopez AD, eds. The global burden of disease: a comprehensive assessment of mortality and disability from diseases, injuries, and risk factors in 1990 and projected to 2020. Vol 43. Cambridge, MA: The Harvard School of Public Health: Harvard University Press; 1996.
- Global health statistics: a compendium of incidence prevalence and mortality estimates for over 200 conditions. Available from: https://www.semanticscholar.org/paper/Global-health-statistics%3A-a-compendium-of-incidence-Murray-Lopez/8964ede8aedd8a6a81be2c0dc156f2d6ef135a0a, accessed on April 5, 2024.
- Addressing the growing burden of trauma and injury in low- and middle-income countries. Am J Public Health. 2005;95:13-7.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Guidelines for essential trauma care: progress in India. World J Surg. 2006;30:930-3.
- [CrossRef] [PubMed] [Google Scholar]
- Trauma care in India: Current scenario. World J Surg. 2008;32:1613-7.
- [CrossRef] [PubMed] [Google Scholar]
- Trauma care in India: A review of the literature. Surgery. 2017;162:S85-106.
- [CrossRef] [PubMed] [Google Scholar]
- Comparing trauma mortality of injured patients in India and the USA: A risk-adjusted analysis. Trauma Surg Acute Care Open. 2021;6:e000719.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- The global burden of disease: 2004 update. Available from: https://www.who.int/publications/i/item/9789241563710, accessed on May 15, 2024.
- 30-Day In-hospital trauma mortality in four urban university hospitals using an Indian trauma registry. World J Surg. 2016;40:1299-307.
- [CrossRef] [PubMed] [Google Scholar]
- Road Accidents in India 2022. Available from: https://morth.nic.in/sites/default/files/RA_2022_30_Oct.pdf, accessed on April 5, 2024.
- The 17 Goals. Available from: https://sdgs.un.org/goals, accessed on April 5, 2024.
- Improvement in trauma care for road traffic injuries: an assessment of the effect on mortality in low-income and middle-income countries. Lancet. 2022;400:329-36.
- [CrossRef] [PubMed] [Google Scholar]
- Guidelines for essential trauma care. Available from: https://www.who.int/publications-detail-redirect/guidelines-for-essential-trauma-care, accessed on April 5, 2024.
- The impact of trauma systems on patient outcomes. Curr Probl Surg. 2021;58:100849.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Trauma training courses and programs in low- and lower middle-income countries: a scoping review. World J Surg. 2021;45:3543-57.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- The effectiveness of trauma care systems at different stages of development in reducing mortality: a systematic review and meta-analysis. World J Emerg Surg. 2021;16:38.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Trauma system development in low- and middle-income countries: a review. J Surg Res. 2015;193:300-7.
- [CrossRef] [PubMed] [Google Scholar]
- Emergency unit assessment of seven tertiary hospitals in Nepal using the WHO tool: a cross-sectional study. Int J Emerg Med. 2023;16:13.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Trauma care in India: capacity assessment survey from five centers. J Surg Res. 2020;252:156-68.
- [CrossRef] [PubMed] [Google Scholar]
- Saving lives on road in India and beyond. Available from: https://savelifefoundation.org/, accessed on April 5, 2024.
- Trauma systems: Origins, evolution, and current challenges. Surg Clin North Am. 2017;97:947-59.
- [CrossRef] [PubMed] [Google Scholar]
- Effectiveness of trauma centers verification: Protocol for a systematic review. Syst Rev. 2019;8:292.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Relationship of trauma centre characteristics and patient outcomes: a systematic review. J Clin Nurs. 2014;23:301-14.
- [CrossRef] [PubMed] [Google Scholar]
- The impact of trauma care systems in low- and middle-income countries. Annu Rev Public Health. 2017;38:507-32.
- [CrossRef] [PubMed] [Google Scholar]
- Impact of trauma system structure on injury outcomes: a systematic review and meta-analysis. World J Surg. 2018;42:1327-39.
- [CrossRef] [PubMed] [Google Scholar]
- The use of tranexamic acid in trauma. Curr Anesthesiol Rep. 2022;12:192-9.
- [CrossRef] [Google Scholar]
- Facilitator Manual for paramedics. National Emergency Life Support. Available from: https://main.mohfw.gov.in/sites/default/files/Facilitator%20Manual%20for%20paramedics.pdf, accessed on May 15, 2024.
- Audit filters for improving processes of care and clinical outcomes in trauma systems. Cochrane Database Syst Rev. 2009;2009:CD007590.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Prehospital care, importance of early intervention on outcome. Acta Anaesthesiol Scand Suppl. 1997;110:71-6.
- [CrossRef] [PubMed] [Google Scholar]
- Missing data in trauma registries: a systematic review. Injury. 2018;49:1641-7.
- [CrossRef] [PubMed] [Google Scholar]
- Trauma registry implementation in low- and middle-income countries: Challenges and opportunities. J Surg Res. 2018;223:72-86.
- [CrossRef] [PubMed] [Google Scholar]
- Global trauma registry mapping: a scoping review. Injury. 2012;43:1148-53.
- [CrossRef] [PubMed] [Google Scholar]
- Trauma registry data collection practices and the impact of hospital data dictionaries: a national survey. J Trauma Nurs. 2022;29:105-10.
- [CrossRef] [PubMed] [Google Scholar]
- Classifying, measuring and improving the quality of data in trauma registries: a review of the literature. Injury. 2016;47:559-67.
- [CrossRef] [PubMed] [Google Scholar]
- Evidence of data quality in trauma registries: a systematic review. J Trauma Acute Care Surg. 2016;80:648-58.
- [CrossRef] [PubMed] [Google Scholar]






