Translate this page into:
Comparative study of endometrial & subendometrial angiogenesis in unexplained infertile versus normal fertile women
For correspondence: Dr Neema Acharya, Department of Obstetrics & Gynaecology, Datta Meghe Institute of Medical Sciences, Deemed to be University, Wardha 442 001, Maharashtra, India e-mail: neemasacharya@gmail.com
-
Received: ,
This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
This article was originally published by Wolters Kluwer - Medknow and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Background & objectives:
Local angiogenesis in endometrium has been shown to be an essential pre-requisite for endometrial receptivity needed for implantation and gestation. Recently, numerous diagnostic gears have been projected to ‘measure’ or ‘estimate’ the endometrial receptivity relying upon angiogenic factors helping throughout implantation. This study evaluated the endometrial and subendometrial blood flow and the local endometrial gland vascular endothelial growth factor (EG-VEGF) expression as markers of local angiogenesis.
Methods:
The present study was done to give quantitative assessment of endometrial thickness (ET), endometrial blood flow and subendometrial blood flow colour Doppler indices with endometrial vascular zones. Endometrial biopsy was taken and with VEGF stained and scored with immunohistochemistry.
Results:
The mean ET for fertile women was 9.41 mm, while in unexplained infertile women it was around 7.90 mm. Upon comparison of ET with EG-VEGF which is considered as a gold standard with correlation coefficient, the present study suggested a positive correlation of EG-VEGF with ET, endometrial pulsatility index (PI), and subendometrial PI also the vascular zones were considered as significant. However, a strong negative correlation was seen with subendometrial resistivity index and PI.
Interpretation & conclusions:
The present study suggests that uterine ultrasound, uterine colour Doppler and EG-VEGF are parameters which can be used as markers of local angiogenesis for endometrial receptivity in the evaluation of women with unexplained infertility.
Keywords
Angiogenesis
Doppler
VEGF
implantation
unexplained infertility
A rising trend observed in carrier-oriented couples, is an increased incidence of infertility12. The main causes of infertility are male factors, uterine, tubal and ovarian factors for female. Upon clinical investigations, most of them do not exhibit any demonstrable cause, and thus such women get labelled as unexplained infertile2. Practically for a couple to be labelled as unexplained infertile, following criteria should be met, i.e., normal ovulatory function, normal semen analysis, normal tubal patency and normal endometrial cavity3. Around 15-30 per cent of the total infertile couples are mainly of this type i.e., unexplained infertility4. A delicate balance is required when it comes to implantation process between human embryo and mother. From a maternal stand point, it is the endometrium that plays the most important role in the implantation process5. Implantation has also been known as ‘The Black Box’of early pregnancy loss6. An efficacious implantation necessitates a normal and functional embryo at the developmental stage of the blastocyst, a receptive endometrium, and a synchrony between embryonic and maternal tissue7.
Numerous diagnostic gears have been projected to measure estimate the endometrial receptivity. These tools include sonographic measures with Doppler and blood flow and molecular expression of vasoactive compounds; both relying upon angiogenic factors helping throughout implantation. A more recent approach to detect endometrial perfusion non-invasively is to detect the blood flow or vascularity of the endometrium during peri-implantation period at endometrial-subendometrial junction8. Thus, with the introduction of Doppler ultrasonography, it is easier to evaluate endometrial and subendometrial blood flow impedance.
Conventionally, endometrial thickness (ET) of greater than 7 mm and a triple-layered endometrial pattern were considered as markers of endometrial receptivity. However, various studies have shown poor implantation rates in spite of good ET and presence of triple-layered endometrial pattern9. Studies have also suggested poor uterine perfusion to be a new found cause of unexplained infertility1011. The blood flow rate of endometrium during the normal menstrual cycle has also been correlated with increased function and expression of many angiogenic factors12.
Endocrine gland derived vascular endothelial growth factor (EG-VEGF), a cell-specific mitogen affecting the endothelium and one of the main factors responsible for vasculogenesis and angiogenesis13. Although the literature mentions above two markers for endometrial angiogenesis viz. EG-VEGF concentration and endometrial and subendometrial blood flow using transvaginal Doppler having potential as predictors of receptivity of endometrium and thereby embryo implantation, the available evidence is still inconclusive for the same. The number of studies done so far is low and also provide sparse data14. Hence, this study was aimed to evaluate the role of endometrial and subendometrial blood flow and local EG-VEGF expression as markers of local angiogenesis in fertile and unexplained infertile women during the peri-implantation period.
Material & Methods
This observational study was carried out over a span of two years between August 2016 to July 2018 in the IVF Clinic, Wardha Test Tube Baby Centre (WTTBC), department of Obstetrics and Gynecology, in co-ordination with the departments of Pathology and Radiology, Acharya Vinoba Bhave Rural Hospital, Datta Meghe Institute of Medical Science, Wardha, India. The study was approved by the Institutional Ethics Committee.
Sample size: The estimated sample size for study was 50 cases and 50 controls based on the following:
η=4σ2[Z1-α/2 +Z1-β]2/E2 where:
σ the assumed Standard Deviation of each treatment response (both treatments assumed equal)=3.9
Z1-α/2 =Related to the chosen significance criteria, α=1.96
Z1-β is the power of test, 80% =0.84
E= Minimum detectable difference between treatment means=28.12-24.27=3.84
η=4*3.9 2 [1.96+0.84] 2/ 3.842.
32.34 (minimum sample size), for a level of significance, a 0.05 and power at 80 per cent.
Inclusion and exclusion criteria: Fifty cases of unexplained infertile women undergoing evaluation for infertility were consecutively recruited in the study group and 50 fertile women were included in the control group. Confounding factors were reduced by matching of study population and restriction by considering the following associated factors. Only those women diagnosed with unexplained infertility were included in the study who fulfilled the following criteria: age <35 yr, not on any medication or treatment for infertility. For the control group, parous women who had proven fertility (having one or more children), with no gynaecological complaint were chosen. Women who were restricted from the study were women who had received hormonal therapy or ovarian stimulation during the cycle of the study. Women having past or present history of pathology of genital tract or ovaries, having any other medical comorbidity or who were on treatment with vasodilators were excluded. Those women whose male partners had abnormal semen analysis were also excluded.
Intervention: A written informed consent was taken from women willing to participate in this study. Of the total 573 infertile women that attended our OPD, 55 cases were those who had unexplained infertility.
All women who participated were given a urinary luteinizing hormone kit (i-Know Ovulation Strip, Piramal Healthcare, Mumbai) to predict ovulation and there after peri-implantation period. Two-dimensional (2D) transvaginal sonography (TVS) was done for a quantitative assessment of ET, endometrial blood flow and subendometrial blood flow colour Doppler indices with endometrial vascular zones. The TVS scan was performed using the E8cS vaginal probe of 4-11 Mega Hertz (MHz) LOGIQ P5 (GE Healthcare pvt. Ltd., Chicago, Illinois, USA).
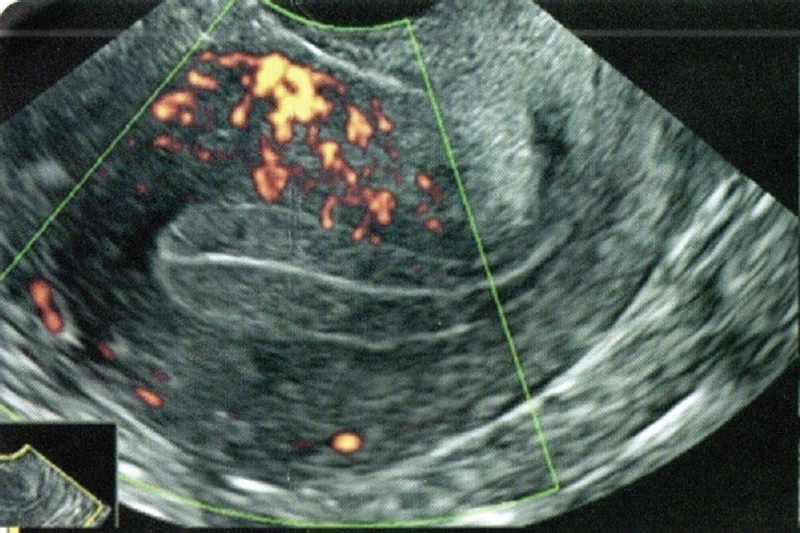
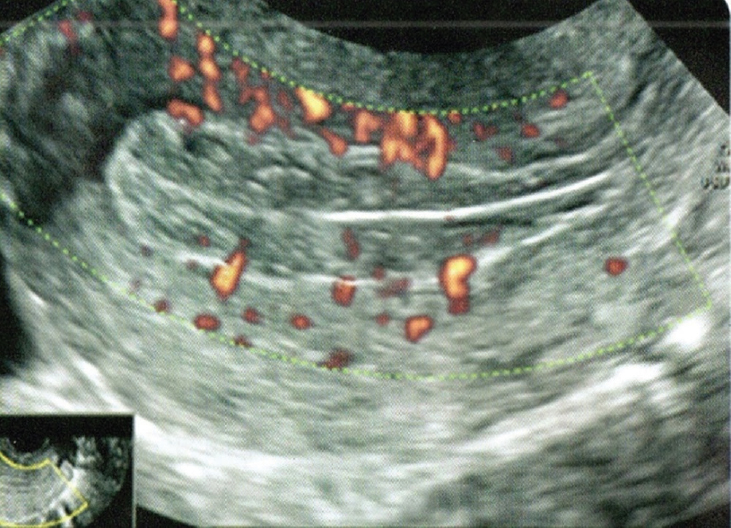
The B mode examination of the ultrasonography was used to evaluate and measure the ET which was labelled as the thickest part of the endometrium sandwiched between two highly reflective echogenic lines in the true uterine longitudinal sagittal scan (Fig. 1). After doing the B mode examination, 2D power 6MHz pulse Doppler was used on the ultrasound machine to gauge the endometrial and sub-endometrial blood flow by doing blood flow analysis (Fig. 2). The Doppler gate was then placed over spiral arteries and sub-endometrial blood flow and measurements were taken on three successive even waveforms. Vascular zones were detected in endometrial-myometrial junction and colour mapping was done accordingly (Figs 3-6). Ultrasonography and Doppler was done on a single machine.

- Representative 2D transvaginal sonography (TVS) scan showing sagittal section of uterus in the secretory phase.
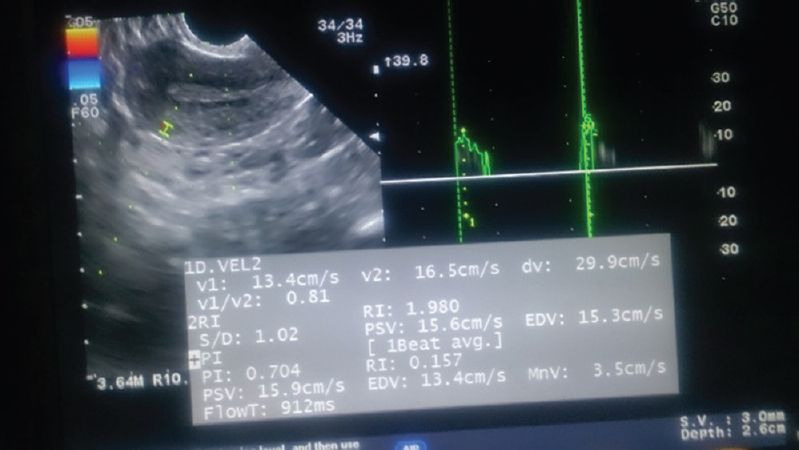
- Representative scan showing Doppler indices of endometrium measured in the secretory phase.

- Representative 2DTVS scan showing the endometrial Vascular zone 0.
- Representative 2DTVS scan showing vascular zone of endometrium in zone 1.
- Representative 2DTVS scan showing vascular zone of endometrium in zone 2.
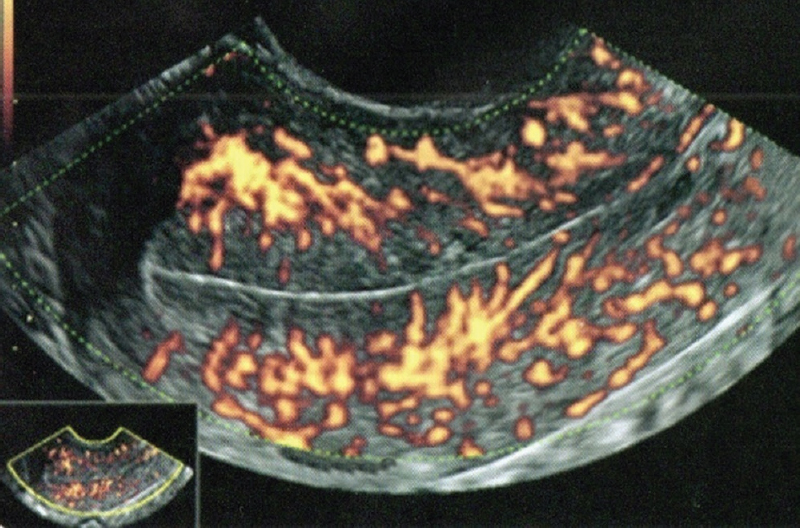
- Representative 2DTVS scan of the vascular zone of endometrium in zone 3.
On the same day of TVS examination and scoring, endometrial samples were drawn using Sterblue Pipelle endometrial suction curette and the biopsy samples were stored in paraffin wax and cut into 4 μm sections and were mounted. One paraffin section was prepared for routine (H and E) examination and the other was positively charged with human recombinant, polyclonal VEGF165 antibody for immunohistochemistry (IHC) study (R & D Systems, Minneapolis, USA). This antibody stained the cytoplasm in positive cells and was studied under Olympus CX21i binocular research microscope and grading was done accordingly (Fig. 7).
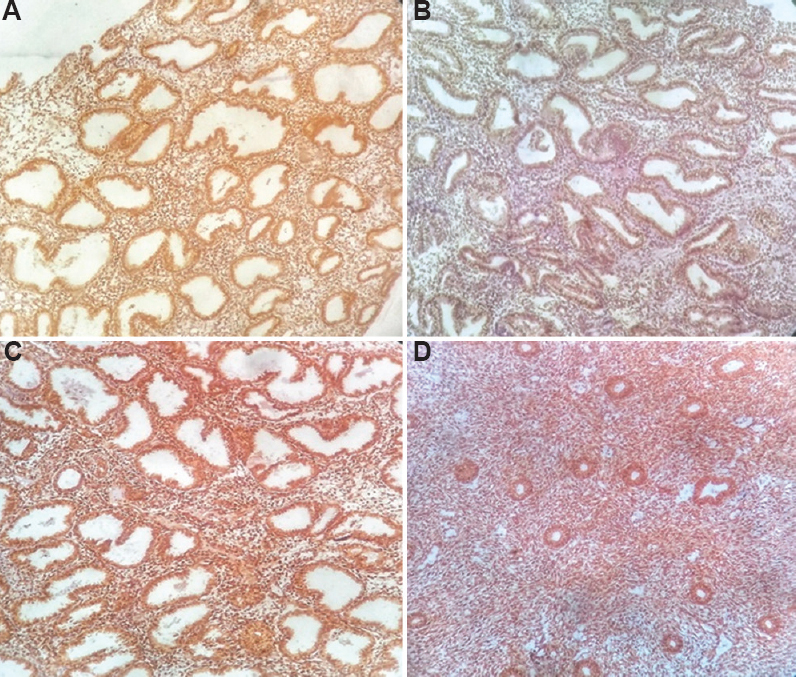
- Endometrial gland vascular endothelial growth factor after immune histochemical staining. (A) grade I, (B) grade 2, (C) grade 3 & (D) grade 4.
Colour mapping of endometrial vascularity was derived from Applebaum scoring system. According to the depth of infiltration of vessels into the ET, zones were distinguished15. The evaluation of staining intensity was performed and studied, later were graded from 0 to 4. The staining was manual in nature16.
Statistical analysis: Data were entered into a predesigned proforma. Statistical analysis was done using inferential and descriptive statistics with the help of Chi-square test, unpaired Student’s t test and Spearman’s Rank order correlation using IBM SPSS 22.0 version (Armonk, NY, USA) and GraphPad PRISM v6.0 (GraphPad Software, CA, USA). P<0.05 was recognized as level of statistically significance. Student’s unpaired t test was done for ET, Doppler and EG-VEGF parameters. Spearman’s Rank order correlation was done for correlation of EG-VEGF with other TVS parameter including Doppler indices and vascularity.
Results
In the present study, out of total of 100 women, 50 cases belonged to unexplained infertile group while 50 controls belonged to fertile group. The mean age distribution in unexplained infertile group was 27.94±4.06 yr while that in fertile group was 27.98±3.53 yr. Out of 50 unexplained infertile women, 66 per cent belonged to primary infertility and rest 34 per cent belonged to secondary infertility. The mean duration of primary infertility was 6.16±2.57 yr while in secondary infertility it was 6.17±1.84 yr.
Table I shows mean value for ET (mm) and parameters of the Doppler study in unexplained infertile and fertile women. The mean value for ET (mm) was 7.90±1.06 mm and for fertile women, it was 9.41±1.09 mm. The mean resistivity index (RI) of endometrial blood flow in unexplained infertile women was 0.54±0.10, while for fertile women, it was 0.50±0.05. The mean value of endometrial pulsatility index (PI) for unexplained infertile women was 0.78±0.09 while in fertile women, it was 1.32±0.13. The mean value of subendometrial RI in unexplained infertile women was 0.72±0.04, while in fertile women, it was 0.32±0.09. The mean subendometrial PI of unexplained infertile women was 0.38±0.11 while in fertile women, it was 1.14±0.09.
| Variables | Mean±SD | |
|---|---|---|
| Unexplained infertile women | Fertile women | |
| ET (mm) | 7.90±1.06*** | 9.41±1.09 |
| Endometrial RI | 0.54±0.10** | 0.50±0.05 |
| Endometrial PI | 0.78±0.09*** | 1.32±0.13 |
| Subendometrial RI | 0.72±0.04*** | 0.32±0.09 |
| Subendometrial PI | 0.38±0.11*** | 1.14±0.09 |
P*<0.01, **<0.001. ET, endometrial thickness; RI, resistivity index; PI, pulsatility index
Table II shows the distribution of women on the basis of the vascular zones and EG-VEGF manual staining score. Out of 100 women examined for vascularity in endometrial and myometrial junction, nil vascularity was found in 36 per cent of unexplained infertile women and six per cent of fertile group. Out of these, only 18 per cent of unexplained infertile women and eight per cent of fertile women had vascularity reaching up to outer most layer of endometrium (Zone 1). Outer half of the endometrial vascularity (Zone 2) was found in 22 per cent in unexplained infertile women and 36 per cent of fertile women. Vascular presence observed penetrating the endometrium (Zone 3) was found in 24 per cent of the unexplained infertile women and 50 per cent of fertile women. The P value was found statistically significant. The Table also shows the distribution of women on the basis on intensity of EG-VEGF staining.
| Distribution of women according to presence of vascularity in different zones | |||
|---|---|---|---|
| Vascular zone | Unexplained infertile group (n=50), n (%) | Fertile group (n=50), n (%) | t test |
| 0 | 18 (36) | 3 (6) | P=0.0003 |
| 1 | 9 (18) | 4 (8) | |
| 2 | 11 (22) | 18 (36) | |
| 3 | 12 (24) | 25 (50) | |
| Total | 50 (100) | 50 (100) | |
| Distribution of women according to EG-VEGF staining manual score | |||
| VEGF staining score | Unexplained infertile group (n=50), n (%) | Fertile group (n=50), n (%) | χ2 test |
| 0 | 18 (36) | 5 (10) | P=0.0001 |
| 1 | 18 (36) | 9 (18) | |
| 2 | 6 (12) | 6 (12) | |
| 3 | 4 (8) | 11 (22) | |
| 4 | 4 (8) | 19 (38) | |
| Total | 50 (100) | 50 (100) | |
| Mean score | 1 | 3 | |
EG-VEGF, endometrial gland-vascular endothelial growth factor
It was also observed that 72 per cent of the unexplained infertile women had absent or light staining of EG-VEGF (score 0 and 1), while rest of the 28 per cent of the unexplained infertile women had uniform EG-VEGF staining of greater intensity. For the same manual score seen in fertile women, it was observed that 72 per cent of fertile women had moderate to intense staining for EG-VEGF against rest of the 28 per cent who had nil to minimum EG-VEGF staining. Score 2, on the other hand, showed equivocal results in both the group. The mean score for EG-VEGF for 50 unexplained infertile women was one (0-1), whereas it was three (2-3) for 50 fertile women.
As shown in Table III, multiple regression analysis was done between the parameters in the study, it was observed that all parameters are independent and are not correlated with EG-VEGF.
| Variables | Unstandardized coefficients | Standardized coefficients (β) | t | P | |
|---|---|---|---|---|---|
| B | SE | ||||
| EG-VEGF | −0.026 | 3.679 | |||
| ET | 0.058 | 0.184 | 0.048 | 0.314 | 0.755 |
| Endometrial RI | −0.716 | 1.796 | −0.061 | 0.399 | 0.692 |
| Endometrial PI | −0.744 | 1.558 | −0.071 | 0.477 | 0.636 |
| Subendomentrial RI | 2.311 | 4.431 | 0.079 | 0.521 | 0.605 |
| Subendomentrial PI | −0.820 | 1.564 | −0.079 | 0.525 | 0.603 |
| Vascular zone | 0.211 | 0.164 | 0.195 | 1.288 | 0.205 |
Table IV shows, correlation (rs, Spearman’s rank correlation coefficient) between EG-VEGF score and sonographic variables to detect angiogenesis. The strength of correlation of EG-VEGF with ET (rs,-0.318) had strongly positive correlation. Strength of correlation of EG-VEGF with endometrial RI (rs,-0.139) shows a negative correlation but P value is non-significant. Correlation of EG-VEGF with endometrial PI (rs,-0.488) concluded there was the strongest correlation. Correlation of EG-VEGF with subendometrial RI (rs,-0.545) had the strongest negative. Subendometrial PI (rs,-0.485) suggested strong positive correlation with statistically significant P value. With correlation with EG-VEGF against vascular zones, rs was found to be (0.335) strongly positive.
| EG-VEGF score | ET | Endometrial RI | Endometrial PI | Subendometrial RI | Subendometrial PI | Vascular zone |
|---|---|---|---|---|---|---|
| rs | +0.318 | −0.139 | +0.488 | −0.545 | +0.485 | +0.335 |
| P | 0.001 | 0.168 | 0.0001 | 0.0001 | 0.0001 | 0.001 |
Discussion
Endometrial receptivity has been defined as a temporary exclusive sequence of factors that make the endometrium amenable to the embryonic implantation17. The endometrium is usually a non-receptive environment for an embryo, except during implantation window which is an optimum period for blastocyst implantation. A human embryo may occur only during a regulated ‘implantation window’ on days 6-10 post ovulation, and surrounded by refractory endometrial status18. Tissue remodelling and angiogenesis are hallmark events during implantation and decidualization. The changing endocrine state of the female during the reproductive cycle and pregnancy results in extensive remodelling of the uterine tissue. There is evidence of endometrial stromal oedema with an increase in the vascular surface area, diameter and total number of capillaries has been reported in the secretory phase during day 21 and 22 of cycle. These changes may be due to oestrogen and progesterone mediated increase in prostaglandins and VEGF production in the endometrium causing vascular permeability.
Expression profiling of genes during the implantation window may aid in identifying genes responsible for implantation failure19. In the present study, the endometrial and subendometrial blood flow and the local EG-VEGF expression were evaluated and compared as markers of local angiogenesis in peri-implantation period of unexplained infertile and fertile women.
For the infertile patients, especially with advanced age, there is a specific parameter that can be seen during TVS known as ‘one stop shop’ which can provide valuable information about the fertility potential within a short time frame. This scan is also known as the ‘fertility scan’ and includes 3D colour power angiography which is generally done between day 10-12 of menstrual cycle. Multivariate regression analysis was used to find out if there is any correlation between unexplained infertility and seven different variables (ET, endometrial PI, endometrial RI, subendometrial flow RI, subendometrial PI, vascular zones and EG-VEGF). It was noted that highest correlation with EG-VEGF was with Endometrial PI, vascular zones, ET, followed by subendometrial PI.
This study was assessed using non-invasive qualitative and quantitative variable (vascular zones, ET, Doppler indices) followed by invasive method (EG-VEGF). The mean ET (mm) for unexplained infertile women was around 7.90±1.06 mm while in fertile women was 9.41±1.09 mm (Table I). Around half of the cases (54%) had minimum ET of 6-8 mm. Almost 32 per cent of fertile women had good ET of more than 10 mm.
One of the strongest predictors of implantation is ET which is dependent on several influences including reproductive age, phase of menstrual cycle, ovarian hormone concentration and endometrial hormone receptor density20. Similar reports have been found in various other cases where the assessment of ET was used to predict pregnancy outcomes and need for IVF-ET further on21. Sources have suggested that the highest pregnancy rate (50%) was seen when ET was around 8-10 mm, least (2.5%) was when the ET was either more than 14 mm or less than 8 mm22.
Endometrial and subendometrial RI for unexplained infertile women in the present study was more than in the fertile women (Table I). Mean PI in endometrial and subendometrial blood flow in unexplained infertile women was less than that in fertile women. Many studies with similar Doppler indices as in the present study have reported similar findings during mid-luteal peri-implantation period through TVS with or without pregnancy outcomes using ART1023. There are also reports of a significant difference seen when Peak Systolic Velocity of spiral artery was done with similar reported findings24. Few studies were found reporting both non-invasive and invasive assessment for endometrial receptivity with similar findings as ours2125. Another study consisted of retrospective analysis of Doppler indices in ART patients, where successful conception was characterized by a significantly lower RI, obtained from subendometrial vessels by transvaginalcolour Doppler ultrasonography26.
Given the findings based on the Doppler indices in the present study, an IVF specialist can start these patients on Sildenafil or Granulocytes-Colony Stimulating Factors.
Varying distribution of vascular zones suggesting poor vascularity was almost always associated with unexplained infertility (54%) in this study. A good vascularity (i.e., for the vessels to reach up to endometrium) was observed in 86 per cent of the fertile women against only 46 per cent of unexplained infertile women. This inference drawn may put forward a hypothesis of unexplained infertile women to have poor vascularity.
In some previous reports pregnancy rates were detected which showed higher pregnancy rates in highly vascular endometrium in contrast to increased miscarriages in pre-pregnant poor vascular endometrium even after successful IVF-ET222728 . A good healthy and vascular endometrium will secrete a higher concentration of growth factors and interleukins aiding in better implantation and better pregnancy outcomes15. To predict outcome of IVF, many grading and staging have come forward based on colour Doppler and ultrasonography (depicting echotexture of endometrium and vascularity)15.
Infertility and endometrial gland vascular endothelial growth factor (EG-VEGF): It is well known that both implantation and VEGF (VEGF-A) gene transcription is enhanced under hypoxic conditions. These are present in microvessels during the secretory period, highlighting a correlation between the increased microvascular density and vascular permeability29. In addition, secretion of VEGF into the lumen of EGs in polarized human endometrial cell cultures suggest that apically secreted VEGF may also function as an endometrial signal for blastocyst development, implantation, or both21.
The mean EG-VEGF score in our study for unexplained infertile was one while the same in fertile women were three showing a significant difference in angiogenic capacity of the endometrium in the above two groups. It was evident that majority of unexplained infertile women had poor EG-VEGF score. As EG -VEGF score indirectly reflects on angiogenesis and endometrial receptivity, our study can also hypothesize poor endometrial receptivity and angiogenesis are major factors associated with unexplained infertile women.
Recent studies have depicted similar outcomes where a direct or indirect quantitative assessment of VEGF has reflected on endometrial angiogenesis establishing better implantation and pregnancy outcomes2129. Newer modalities with different approaches have also been tried for similar purpose, using EG-VEGF and Optical Coherence Test (OCT) of endometrial biopsy. Their findings suggested that OCT appeared to be a promising non-invasive or minimally invasive alternative to study endometrial vascularity in women with reproductive failure14.
Our study has concluded majority of unexplained infertile women had sparse vascularity in endometrial-myometrial junction unlike most of the fertile women who had good vascularity. This may represent an etiological factor in the proposed reduced endometrial receptivity; which is one of the suggested underlying causes in women with unexplained infertility.
Correlation of endometrial gland vascular endothelial growth factor (EG-VEGF) and sonographic variables
It was noted that the highest correlation (rs and P value) with EG-VEGF was with Endometrial PI, vascular zones, ET, followed by subendometrial PI. Previously, there have been significant negative correlation findings with EG-VEGF with endometrial and subendometrial RI. One of the similar study noticed positive correlation with ET, endometrial PI, RI and strong negative correlation with subendometrial RI and PI. Provided EG-VEGF to be gold standard, non invasive markers such as endometrial and subendometrial PI take precedence over vascular zones and ET to understand vasculogenesis in endometrium.
With reference to correlation co-efficiency, the next best evaluation for any unexplained infertile women would be Doppler indices followed by vascular zones and least by ET. A combination of such parameters would be thus most efficient for similar evaluation30.
Overall, the present study suggests that endometrial and subendometrial blood flow should be studied along with ET while evaluating and treating women with unexplained infertility in perimplantation period. The above can be studied by non-invasive methods of ultrasound and colour Doppler for assessment for endometrial receptivity. Endometrial biopsy evaluation by IHC for EG-VEGF should also be done in unexplained infertility in peri implantation period. If found to be abnormal, treatment can be started to improve endometrial blood flow , which may enhance her chance of conceiving. Further research should be done to study on treatment outcomes for improving endometrial angiogenesis and its effect on pregnancy rates. In our study, endometrial and subendometrial RI had a negative correlation with non-significant relation with EG-VEGF, however, further research in a larger sample size may be needed to throw light on this aspect.
Financial support & sponsorship: The first author (MS) received thesis funding support from ICMR, New Delhi.
Conflicts of Interest: None.
References
- Infertility definitions and terminology. Available from: http://www.who.int/reproductivehealth/topics/infertility/definitions/en/
- A journey of hope:an institutional perspective of Japanese outbound reproductive tourism. Curr Issues in Tourism. 2020;23:52-67.
- [Google Scholar]
- Female Infertility. In: StatPearls [Internet]. Florida: StatPearls Publishing; 2021.
- [Google Scholar]
- Potential biochemical markers of uterine receptivity. Hum Reprod. 1999;14(Suppl 2):3-16.
- [Google Scholar]
- Conception to ongoing pregnancy:The 'black box'of early pregnancy loss. Hum Reprod Update. 2002;8:333-43.
- [Google Scholar]
- Illuminating the “Black Box”of progesterone-dependent embryo implantation using engineered mice. Front Cell Dev Biol. 2021;9:640907.
- [Google Scholar]
- Ultrasonography and Doppler Study to Predict Uterine Receptivity in Infertile Patients Undergoing Embryo Transfer. J Obstet Gynaecol India. 2016;66(Suppl 1):377-82.
- [Google Scholar]
- The endometrium in assisted reproductive technology:How thin is thin? J Hum Reprod Sci. 2016;9:3-8.
- [Google Scholar]
- Endometrial spiral artery Doppler parameters in unexplained infertility patients:Is endometrial perfusion an important factor in the etiopathogenesis? J Turk Ger Gynecol Assoc. 2012;13:169-71.
- [Google Scholar]
- Uses of ultrasound and Doppler in assessment of endometrial receptivity in patients of unexplained infertility. Egypt J Hosp Med. 2018;73:7542-50.
- [Google Scholar]
- Circulating angiogenic factors during periovulation and the luteal phase of normal menstrual cycles. Fertil Steril. 2004;81:1322-7.
- [Google Scholar]
- Endocrine Gland-Derived Vascular Endothelial Growth Factor/Prokineticin-1 in Cancer Development and Tumor Angiogenesis. Int J Endocrinol. 2017;2017:3232905.
- [Google Scholar]
- Endometrial vascularization characterized by optical coherence tomography and immunohistochemistry in women undergoing in vitro fertilization-embryo transfer treatment. Medicina (Kaunas). 2019;55:81.
- [Google Scholar]
- Evaluation of uterine biophysical profile and to assess its role in predicting conception among unexplained primary infertility patients. Indian J Community Health. 2014;26:401-5.
- [Google Scholar]
- Estimation of immunohistochemical expression of VEGF in ductal carcinomas of the breast. J Histochem Cytochem. 2011;59:750-60.
- [Google Scholar]
- Endometrial Receptivity in Eutopic Endometrium of Women with Endometriosis It is affected, let me show you why. Fertil Steril. 2017;108:19-27.
- [Google Scholar]
- What is the contribution of embryo-endometrial asynchrony to implantation failure? J Assist Reprod Genet. 2016;33:1419-30.
- [Google Scholar]
- Micro RNA signature and regulatory functions in the endometrium during normal and disease states. Semin Reprod Med. 2008;26:479-93.
- [Google Scholar]
- Influences on endometrial development during intrauterine insemination:Clinical experience of 2,929 patients with unexplained infertility. Fertil Steril. 2013;100:194-9.e1.
- [Google Scholar]
- Assessment of uterine, subendometrial blood flows and endometrial gland vascular endothelial growth factor (EG-VEGF) in women with unexplained infertility. Middle East Fertil Soc J. 2015;20:119-26.
- [Google Scholar]
- The usefulness of endometrial thickness, morphology and vasculature by 2D Doppler ultrasound in prediction of pregnancy in IVF/ICSI cycles. Egypt J Radiol Nucl Med. 2016;47:341-6.
- [Google Scholar]
- Color Doppler Study of Endometrial Spiral Artery in Unexplained Infertility. IJMSIR. 2018;3:86-8.
- [Google Scholar]
- Endometrial and subendometrial perfusion are impaired in women with unexplained subfertility. Hum Reprod. 2004;19:2605-14.
- [Google Scholar]
- Assessment of endometrial receptivity by transvaginal color Doppler and three-dimensional power Doppler ultrasonography in patients undergoing in vitro fertilization procedures. J Ultrasound Med. 2001;20:125-34.
- [Google Scholar]
- Role of endometrial blood flow assessment with color Doppler energy in predicting pregnancy outcome of IVF-ET cycles. Reprod Biol Endocrinol. 2010;8
- [Google Scholar]
- Predictive value of endometrial thickness, pattern and sub-endometrial blood flows on the day of hCG by 2D Doppler in in vitro fertilization cycles:A prospective clinical study from a tertiary care unit. J Hum Reprod Sci. 2011;4:29-33.
- [Google Scholar]
- Vectorial secretion of vascular endothelial growth factor by polarized human endometrial epithelial cells. Fertil Steril. 1998;69:909-15.
- [Google Scholar]
- Optimal timing of ultrasonographic and Doppler evaluation of uterine receptivity to implantation. Reprod Biomed Online. 2008;16:368-75.
- [Google Scholar]






