Translate this page into:
Coagulation abnormalities & thromboprophylaxis in COVID-19
For correspondence: Dr Amit Malviya, Department of Cardiology, North Eastern Indira Gandhi Regional Institute of Health and Medical Sciences, Mawdiangdiang, Shillong 793 018, Meghalaya, India e-mail: dramit_malviya@rediffmail.com
This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
This article was originally published by Wolters Kluwer - Medknow and was migrated to Scientific Scholar after the change of Publisher.
Abstract
The ongoing pandemic of novel coronavirus 2019 is rapidly evolving, and newer organ- and system-specific manifestations are being observed. Thrombotic complications and coagulopathy are frequent manifestations of the disease, especially in sick patients, which appear to be unique and distinct from sepsis-induced coagulopathy, disseminated intravascular coagulation and other viral infection-induced coagulation abnormalities. Elevated D-dimers and fibrinogen in the early stage of the disease with minimally deranged prothrombin time and platelet counts are prominent and distinguishing features. Venous and arterial thromboses, as opposed to bleeding events, are the major clinical correlates. There is much to be known about the pathogenesis of COVID-associated coagulopathy; however, the mechanisms overlap with thrombotic microangiopathy, haemophagocytic syndrome and antiphospholipid syndrome compounded by the diffuse endothelial damage. The recommendations regarding the treatment are still evolving, but antithrombotic therapy has a definite role in positive outcomes of sick patients.
Keywords
Anticoagulants
coagulopathy
coronaviruses
COVID-19
disseminated intravascular coagulation
pulmonary embolism
SARS-CoV-2
The novel SARS-CoV-2 pandemic is evolving at a rapid pace globally. The newer manifestations of the disease and its complications are frequently reported since its early reports from Wuhan, China1. This global pandemic has affected around 181 million people throughout the world and caused more than 3.5 million deaths till May & June 2021 end2. The death due to COVID-19 predominantly occurs due to respiratory complications and subsequent multiorgan involvement. However, a sizable number of patients die due to cardiac injury and multiorgan failure3. There is no proven cure currently, and the antiviral agents along with other repurposed drugs including hydroxychloroquine were shown not to be effective45.
Thromboembolic complications such as deep venous thrombosis (DVT) and pulmonary thromboembolism (PTE) are being consistently diagnosed in critically-ill COVID-19 patients, and they correlate with adverse outcomes6. Coagulopathy is usually observed in patients with severe COVID-19, likely due to infection-associated inflammatory changes and disseminated intravascular coagulation (DIC)7. The administration of low-molecular-weight heparin (LMWH) has been reported to reduce mortality in critically-ill patients who have sepsis-induced coagulopathy (SIC) or with significantly raised D-dimer levels8. Here we aim to discuss the coagulation abnormalities and their pathophysiology in COVID-19 and the currently available management strategies.
Coagulation abnormalities in SARS and Middle East respiratory syndrome (MERS) epidemic: Lessons from the past
In the past, closely-related viruses such as SARS-CoV and MERS-CoV have caused epidemics in 2003 and 2012, respectively910. These epidemics were lesser in scale as compared to the current pandemic, but relevant information from these epidemics could be crucial in understanding the dynamics of the present COVID-19 pandemic.
SARS-CoV-1 originated in China in 2003 and affected 29 countries, with a mortality rate of approximately 10 per cent9. Coagulopathy and thromboembolic manifestations similar to COVID-19 were reported with SARS-CoV-1. An autopsy study of eight cases of SARS revealed the presence of PTE, DVT and multiorgan infarcts in 4, 3 and 2 patients, respectively11. Umapathi et al12 reported ischaemic strokes in five of 206 SARS patients, with approximately 30 per cent incidence of venous thromboembolism (VTE) in patients who were critically ill. The predominant coagulation abnormalities seen were thrombocytopenia (44.8%), deranged activated partial thromboplastin time (aPTT, 42.8%) and elevated D-dimer (45.0%)13. Furthermore, the sensitivity and specificity of thrombocytopenia (in combination with other systemic features such as muscle pains, fever, loose stools, sore throat and lymphopenia) in effectively detecting SARS-CoV-1 were 100 and 86.3 per cent, respectively14.
MERS-CoV originated in Saudi Arabia in 2012 and utilized dipeptidyl peptidase-4 receptor for cellular entry. It spread to 26 countries and the total confirmed cases of MERS-CoV were 2494 with case fatality rate of 37.1 per cent10. Like SARS-CoV-1 disease, thromboembolic complications and haematologic manifestations were common. Pre-clinical studies involving transgenic mice with human dipeptidyl peptidase-4 receptors established their role in MERS-associated coagulation abnormalities15. Thrombocytopenia was common and DIC was seen in the non-survivors16.
Coagulation abnormalities in COVID-19
SARS-CoV-2–associated coagulopathy was distinct from other similar RNA viruses (such as Ebola, Lassa and dengue fever) where haemorrhagic manifestations were common. Instead, bleeding complications are uncommon in COVID-19. Majority of the patients are asymptomatic; however, in minority of affected individuals (especially with comorbidities and elderly population) who go on to develop severe disease, it led to a hyperinflammatory state (cytokine storm) known as thromboinflammatory state or COVID-19–associated coagulopathy (CAC)1718. Triggering of coagulation cascade as a defense mechanism to limit the viral dissemination becomes uncontrolled and detrimental.
The increase in VTE, myocardial infarction and pulmonary embolism suggests the hypercoagulable state in COVID-1917. In addition, coagulation abnormalities in CAC are different from DIC. In the setting of COVID-19, direct viral insult to endothelial cells in pulmonary and systemic circulation has been hypothesized as one of the key mechanisms for inciting hypercoagulation19. Multiple factors are known to contribute to CAC. First, cytokine storm stimulates coagulation cascade and synthesis of pro-inflammatory cytokines such as interleukin (IL) 1-beta and IL-6. These cytokines augment tissue factor expression on immune cells and set off the extrinsic pathway. Second, release of plasminogen activator inhibitor-1 and reduced activity of urokinase-type plasminogen activator result in suppression of fibrinolytic system. Third, pro-inflammatory cytokines and damaged endothelium lead to platelet activation and aggregation. Fourth, the presence of endothelial damage further hastens the thrombotic process20.
There are various coagulation abnormalities in COVID-19 patients such as normal or marginally prolonged prothrombin time (PT) and aPTT, normal or marginally increased platelet counts, elevated fibrinogen level, elevated D-dimer level, enhanced factor VIII activity and elevated von Willebrand factor (vWF) antigen, which are consistent with endothelial injury21. Most common abnormalities are raised D-dimers and fibrinogen levels. Elevation of coagulation markers in the hospital setting is associated with poor outcomes with decreased survival17. The difference between CAC and DIC is summarized in Table I.
| Variable | CAC | DIC |
|---|---|---|
| PT | Modestly increased | Higher than CAC |
| aPTT | Normal | Often increased |
| D-dimer levels | Markedly increased | Increased |
| Fibrinogen | Increased | Decreased |
| Platelet count | Mildly reduced | Markedly reduced |
Source: Ref 66. PT, prothrombin time; aPTT, activated partial thromboplastin time
Clinical correlates of COVID-19 coagulopathy
The venous and arterial thrombotic manifestations seen in COVID-19 patients include DVT, PTE, myocardial infarction and ischaemic stroke222324. VTE has been reported in up to one-third of the patients managed in intensive care unit (ICU) despite prophylactic anticoagulation (17-47%)25. Risk factors include immobilization during critical care, acute inflammatory state, endothelial cell damage and stasis.
Pulmonary embolism (PE) is the mortality leading cause of death in COVID-1926. The cumulative incidence of PE was 20.6 and 23 per cent in two different case series from Italy27. The embolism was frequently present in segmental arteries of pulmonary artery28. There exists a controversy on PE or pulmonary thrombosis due to direct endothelial injury by the SARS-CoV-2. Ackermann et al29 reported unique post-mortem morphological and molecular abnormalities, which supported angiocentric predilection of inflammation. In addition to widespread vascular endothelial damage and thrombotic changes, intussusceptive angiogenesis was also reported as a dominant contributor to the formation of new vessels (angiogenesis)30.
Epidemiological data
The study on baseline characteristics of the first 99 patients hospitalized in Wuhan suggested elevated aPTT, PT and D-dimer in 6, 5 and 36 per cent patients, respectively. Elevated levels of inflammatory biomarkers including IL-6, erythrocyte sedimentation rate (ESR) and C reactive protein (CRP) were also reported in these patients31. In a study comprising 449 severe COVID-19 patients, 22 per cent had an International Society of Thrombosis and Haemostasis, SIC score (ISTH-SIC) >48. The initial studies from the Netherlands reported 27 per cent cumulative incidence of VTE in ICU patients32. The second study reported 11 and 23 per cent incidence of symptomatic VTE at 7 and 14 days, respectively33. As compared to patients admitted in general wards, the hazard ratio for VTE in ICU patients was reported to be 3.8 (95% CI, 1.3-12)33. In an Italian cohort, 67 patients of COVID-19 were enrolled in the emergency department. As compared to controls, significantly elevated fibrinogen levels were found in COVID-19 patients (601 vs. 455 mg/dl, P<0.01). The proportion of patients with fibrinogen levels >400 mg/dl (86 vs. 58%; P<0.01) was also significantly higher34.
Pathogenesis of coagulopathy and thrombosis in COVID-19 patients
The COVID-19 patients commonly present with unique coagulation abnormalities which mirror the disease severity and confer vulnerability for thromboembolic complications1835. Apart from abnormal coagulation parameters reported by observational studies, various autopsy reports have highlighted the presence of platelet-fibrin thrombi in pulmonary as well as systemic vasculature, along with the features of endothelial injury and intussusceptive angiogenesis29. Though the exact underlying mechanisms for haemostatic abnormalities are not yet completely understood, the participation of multiple complex pathways has been contemplated in the pathogenesis of CAC (Fig. 1).
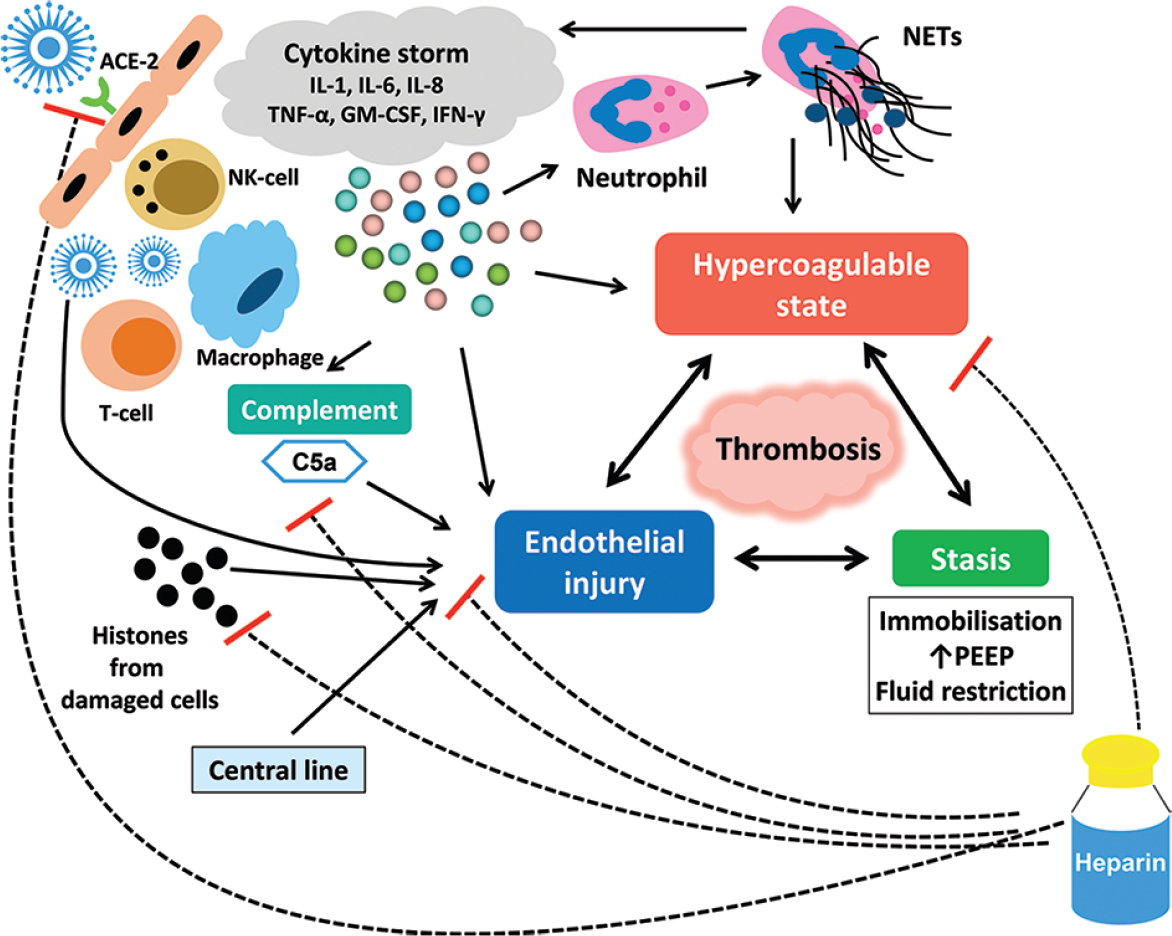
- Pathogenesis of COVID-19–associated coagulopathy. The S1 subunit of Spike ‘S’ protein on the surface of SARS-CoV-2 virus engages with membrane-bound cellular receptor carboxypeptidase ACE2 presents over the cell membrane of lung epithelial cells (pulmonary alveolar type II cells). S2 subunit stalk mediates cellular binding of SARS-CoV-2. After entry, virus replicates and causes cytokine storm, complement activation, activation of macrophages, T-cells, NK-cells, neutrophils; and increase in angiotensin II levels. Direct viral injury, complement activation, histones from damaged cells and raised angiotensin II levels collectively produce endothelial injury. Cytokine storm, complement activation, antiphospholipid antibodies and NETs create hypercoagulable state in COVID-19. Furthermore, immobilization, raised PEEP and fluid restriction produce stasis, and completes the Virchow's triad of thrombosis. The positive effect of heparin is multifactorial. Heparin prevents both endothelial injury and thrombus formation in COVID-19. Black arrows indicate upregulation, and dotted lines with red bar indicate downregulation. ACE2, angiotensin converting enzyme 2; APLA, antiphospholipid antibody; GM-CSF, granulocyte monocyte colony stimulating factor; IL, Interleukin; INF-γ, Interferon-γ; NK cell, natural killer cell; NETs, neutrophils extracellular traps; PEEP, positive end expiratory pressure; TNF-α, tumour necrosis factor-a.
To some extent, CAC mimics the features of DIC, SIC and/or thrombotic microangiopathy718 In a study, relative to 71 per cent COVID-19 non-survivors who were labelled as DIC (as per the ISTH criteria), merely 0.6 per cent COVID-19 survivors exhibited DIC features35.
A small number of COVID-19 patients (approximately 5%) present with platelet count less than 100,000/µl during the course of illness, reflecting lack of role of DIC-like consumption coagulopathy as an underlying process363738. The clinical relevance of these haemostatic abnormalities is affirmed by the high incidence of thromboembolic manifestations18. The presence of these abnormalities has been reported to be associated with more severe illness and higher mortality risk3940. The haemostatic abnormalities in COVID-19 have been shown to go hand-in-hand with elevation in pro-inflammatory cytokines levels38. This indicates intricate involvement of coagulation and inflammatory cascades in the natural history of COVID-1941.
The major closely associated mechanisms that contribute to coagulation abnormalities and thrombotic events include activation of coagulation cascade, repression of fibrinolysis, platelet activation and endothelial dysfunction20. In addition to preponderance of diffuse alveolar damage and cardiac involvement, the autopsy studies have specifically highlighted the presence of thrombi comprising platelets and fibrin in pulmonary and systemic vasculature424344454647. Multisystem involvement with widespread thrombosis in post-mortem COVID-19 studies was found to be unaffected by the presence or absence of pre-existing comorbidities44. In a multicentre study, Borczuk et al46 reported macrothrombi and microthrombi in 42 and 84 per cent patients, respectively. Carsana et al42 reported the presence of fibrin thrombi during post-mortem examination among 87 per cent of cases. These thrombi were predominantly demonstrated in the blood vessels adjacent to lung parenchyma with maximum alveolar and endothelial damage, and their presence was associated with high D-dimer levels in the peripheral blood42. These findings highlight the contribution of coagulopathy in the overall pathogenesis of COVID-19 and its complications, especially thrombosis.
It is now well recognized that the respiratory system is the predominant portal of entry for SARS-CoV-2. Like other coronaviruses, it gains cellular access by engaging angiotensin-converting enzyme 2 (ACE2)4849. ACE2 is a transmembrane carboxypeptidase that is abundantly distributed on pulmonary alveolar epithelium and vascular endothelium, and it normally regulates the renin-angiotensin system (RAS). The availability of ACE2 on cellular surface is decreased following its internalization with SARS-CoV-2 viral particles, thereby compromising its normal catalytic action on angiotensin II50. As a consequence, there is excess of angiotensin II in the circulation which exerts vasoconstrictive, inflammatory and procoagulant effects4951. Invasion of lungs by SARS-CoV-2 triggers the immune system. Various cytokines are produced by the immune cells that include tumour necrosis factor-α (TNF-α), interferon-γ, ILs (including IL-1 and IL-6) and others3752. Apart from the perpetuation of the inflammatory process, these cytokines also stimulate extensive tissue factor expression on circulatory mononuclear cells and also cause widespread stimulation of the coagulation cascade. As a protective mechanism to restrict the viral spread, it is suggested that the formation of microthrombi and neutrophil extracellular traps (NETs) in pulmonary vasculature is initiated early in the disease course53. Subsequently, this process spills over to systemic circulation, generating large amounts of thrombin and a procoagulant milieu across the body17. Excessive secretion of pro-inflammatory cytokines culminates in cytokine storm which clinically manifests in the form of multiorgan dysfunction54. These patients inevitably need ICU care and have dismal prognosis555657.
The role of endothelial injury in the pathogenesis of CAC has been substantiated58. V Goshua et al59 have reported that COVID-19 patients admitted in ICU display remarkable elevation in plasma ultra-large vWF and P-selectin levels relative to non-ICU patients. Apart from direct damage caused by SARS-CoV-2, it is proposed that endothelial integrity is adversely affected by inflammatory cytokines, NETs, hypoxia and complement stimulation60. The expression of thrombomodulin on the endothelial cells prevents thrombus formation on their surface. The endothelial injury leads to enhanced shedding of thrombomodulin from endothelial surface, making it vulnerable to thrombus formation61. The ultra-large vWF multimers and P-selectin stored in Wibel–Palade bodies are released by the injured endothelium. The excess of ultra-large vWF particles in circulation leads to thrombotic microangiopathy by causing platelet aggregation and activation21. These findings are in congruence with the post-mortem reports which have demonstrated features of endothelial cell injury in the form of endothelial apoptosis and loss of tight junctions29. The intussusceptive angiogenesis noted on autopsy has also been attributed to pro-angiogenic properties of vWF levels62.
Collectively, available literature suggests that the coagulation abnormalities seen in COVID-19 patients overlap with DIC, thrombotic microangiopathy and SIC. These abnormalities are more pronounced in critically ill patients where these predict survival. Multiple mechanisms are proposed to explain CAC. The identification of key drivers of coagulopathy in this context shall be crucial to define the potential therapeutic targets.
Management of thrombotic complications in COVID-19
As delineated by the early studies, hypercoagulability has emerged as a unique and consistent feature of COVID-19. Thromboprophylaxis has now become an integral part of the management protocols for hospitalized COVID-19 patients17. However, many patients develop thrombotic complications despite receiving standard-dose thromboprophylaxis. Therefore, a higher heparin dose has been used for this purpose. There are no robust, high-quality data to support such practice. However, considering the data from observational studies and autopsy reports, it is apparent that inflammation, coagulopathy and thrombotic manifestations go hand-in-hand in COVID-1918. Whether increasing dose of heparin will clinically benefit the patients with severe COVID-19 is not known. The ongoing trials looking into the safety and efficacy of various anticoagulant regimens shall be able to provide a solution for this conundrum.
Various guidelines have been put forward by the professional societies to assist the healthcare workers in dealing with the menace of coagulopathy and thrombosis in COVID-196364. Most of these recommendations are based on the opinions of expert panels and findings of observational studies. In India, the Ministry of Health and Family Welfare has published recommendations for the management of COVID-19 patients65. High-quality evidence supported by the randomized trials is currently lacking for managing coagulopathy in COVID-19. Various studies have been initiated to find the optimum management of coagulation abnormalities in such patients.
Venous thromboembolism prophylaxis for COVID-19 patients
Immunothrombosis has been described in the pre-COVID era to highlight the two-way association that exists between inflammation and coagulation cascade. COVID-19 pathophysiology provides further support to this association6667. The ability of heparin to block thrombin production, especially in the lung vasculature, is the main mechanism through which it limits the ongoing SARS-CoV-2–driven inflammation666869. However, the advantage of heparin over other anticoagulants in the setting of COVID-19 is also reinforced by its potential multiple ancillary mechanisms of actions7071. These include anti-inflammatory action through inhibition of neutrophil chemotaxis and sequestration of circulating cytokines (including IL-6), acute-phase reactants and complement factor 5a7172737475. Through its binding to histones emanating from the damaged cells and interfering with their methylation, heparin might confer endothelial protection and improve microcirculation7677. Some experimental studies have shed light on the antiviral action of heparin in the context of herpes virus and Zika virus infection6869. It is proposed that by engaging spike S1 receptor binding domain of SARS-CoV-2, heparin exerts antiviral action70. However, there is no published literature which supports direct oral anticoagulants (DOACs), fondaparinux or warfarin (vitamin K antagonist) exhibiting similar properties.
LMWH has certain advantages over unfractionated heparin (UFH) in the setting of COVID-19 due to the lower incidence of heparin-induced thrombocytopenia and less frequent dosing intervals in the former. Once-daily dosing schedule also makes fondaparinux a reasonable alternative to LMWH, but longer half-life and difficulties in achieving reversal are its drawbacks. UFH is preferable in situations where patients develop renal impairment (creatinine clearance <30 ml/min) and have increased bleeding risk. Studies suggest that DOACs achieve variable plasma levels in COVID-19 patients who are simultaneously receiving antiviral and experimental drugs78. The patients with absolute contraindications to pharmacological thromboprophylaxis may be the candidates for mechanical thromboprophylaxis with intermittent pneumatic compression.
Symptomatic non-hospitalized patients
Thrombosis has been reported to be the presenting manifestation of COVID-197980. Considering the limited number of hospital beds in resource-constraint settings, many patients might be receiving home-based care for mild symptoms. The current guidelines do not suggest prophylactic anticoagulation for these patients. However, there is a need for more data on the thrombotic risk among these patients.
Non ICU hospitalized COVID-19 patients
Administration of LMWH or UFH as prophylactic anticoagulation is the standard of care for hospitalized patients who are acutely-ill8182. It seems obvious that the thrombotic risk is more among the hospitalized COVID-19 patients, but the exact magnitude is not yet known. In the absence of absolute contraindications, universal thromboprophylaxis with standard anticoagulant doses is currently the accepted norm for non-ICU patients64. Failure of standard dose prophylactic anticoagulation to prevent VTE has been seen in critically-ill patients832. This has resulted in acceptance of a more aggressive policy towards thromboprophylaxis by using intermediate-dose regimens, especially in critically-ill patients8. At present, there are no published trials to support this strategy.
ICU hospitalized COVID-19 patients
ICU patients have higher tendency for developing VTE and mortality83. The ideal thromboprophylaxis strategy for these patients is yet to be defined. Use of LMWH at standard prophylactic and intermediate doses is found to be beneficial84. Intermediate-dose thromboprophylaxis with LMWH (0.5 mg/kg twice a day) shall be considered for obese patients [body mass index (BMI) >30 kg/m2]. The safety and efficacy of therapeutic dose LMWH as prophylaxis in all ICU patients are not yet proven64. A simplified approach to VTE prophylaxis and treatment has been described in Fig. 2.
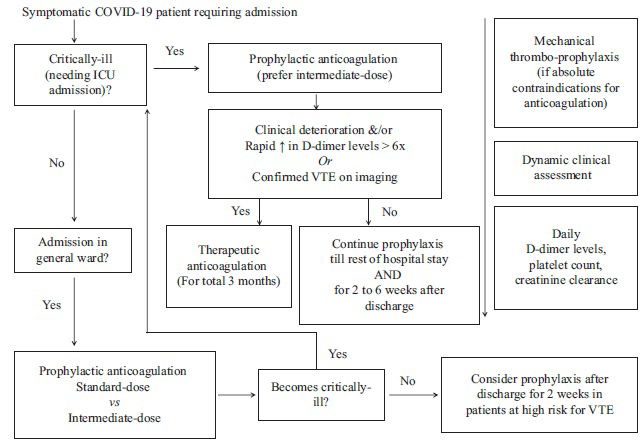
- Proposed flow diagram for the management of symptomatic COVID-19 patients with anticoagulation on the basis of available evidence. VTE, venous thromboembolism.
Role of post-discharge thromboprophylaxis
The benefit of post-discharge thromboprophylaxis for preventing VTE is not yet clear. The overall incidence of VTE after discharge is low, and hence, post-discharge prophylaxis for all patients is not necessary. Two recent retrospective studies have analyzed VTE and bleeding rates among COVID-19 patients following discharge. Patell et al85 reported thrombotic and bleeding complications at 30 days after discharge in 2.5 and 3.7 per cent COVID-19 patients, respectively. Roberts et al86 observed that VTE risk following discharge was comparable between COVID-19 and non-COVID patients who were hospitalized for other medical illnesses [OR 1.6 (95% CI 0.77-3.1)]. Adopting an individualized approach tailored to each patient's bleeding and thrombotic risk is pragmatic. Patients with low bleeding risk who have another indication for continuing thromboprophylaxis (such as pregnant women, following orthopaedic procedure and continued inpatient care at an alternate centre) may benefit from post-discharge thromboprophylaxis85. As per the ISTH guidelines, COVID-19 patients with additional prothrombotic risk factors who may benefit from 2-6 wk extended-thromboprophylaxis include those with old age, ICU stay, active malignancy, past history of VTE, elevated D-dimer during hospitalization (>2 times the upper limit of normal) and IMPROVE-VTE score ≥464.
Role of VTE risk stratification in hospitalized COVID-19 patients
Universal thromboprophylaxis in all hospitalized patients is preferred approach rather than the individualized approach guided by the risk assessment scores6487. Padua VTE prediction score and IMPROVE VTE risk assessment score estimate the thrombotic risk by incorporating various patient-specific factors such as old age, immobilization, presence of malignancy, past history of VTE and presence of thrombophilia6487. Based on the severity of clinical features and derangement in haemostatic parameters (D-dimer levels, platelet count, PT and aPTT), Thachil et al88 have proposed a staging system for COVID-related coagulopathy. It is based on the assumption that due to entry of SARS-CoV-2 through respiratory tract, CAC initially manifests as microthrombi in pulmonary vasculature (stage 1). With clinical worsening, progression from microthrombi to macrothrombi takes place which may have role of full dose anticoagulation (stage 2). In stage 3, there is further worsening with requirement for mechanical ventilation or extracorporeal membrane oxygenation (ECMO). In addition to full-dose anticoagulation, the possible role of experimental strategies [such as fibrinolysis, designer heparin molecules (heparan sulphate)] is proposed for stage 3 patients89. The validation of such staging systems in prospective studies is required.
Diagnosis of venous and arterial thromboses in COVID-19 patients: Do we need to screen all patients at admission?
There is an ongoing debate on the strategy which should be followed in testing for DVT or PTE in hospitalized patients – aggressive versus conservative. It needs to be emphasized that performing compression ultrasound for DVT and echocardiography to look for right ventricular (RV) strain is difficult for COVID-19 patients, especially those who are on mechanical ventilation. As there is a high risk of transmission of infection to other hospitalized patients and healthcare staff, adopting a rational approach towards carrying out these investigations for VTE diagnosis is prudent. Isolated elevation of D-dimer levels may not be beneficial in guiding testing for VTE, as D-dimer levels elevation can be seen in a majority of hospitalized patients. This finding is not specific for VTE in acutely-ill patients90. Close monitoring for the signs of clinical deterioration with supervision of D-dimer trajectory is a pragmatic strategy.
The current guidelines advise against the routine VTE screening in the hospitalized patients64. The utilization of point-of-care tests such as compression ultrasound and echocardiography should be guided by the clinical suspicion. Worsening of clinical parameters and development of asymmetrical limb swelling are the clues that may suggest that the patient is having VTE. A sudden clinical deterioration should specifically prompt a close look at echocardiography to see for acute right atrium (RA)/right ventricle (RV) dilation suggesting acute pulmonary embolism (PE).
As per a recent systematic review, symptomatic arterial thrombosis can develop in up to four per cent critically ill patients91. Uncommonly, either free floating aortic thrombus or acute aortic occlusion (AAO) due to thrombosis has been reported. Free floating aortic thrombus is usually an incidental imaging finding which is infrequently associated with limb or visceral ischaemia9293. Development of acute ischaemia involving extremities and/or visceral organs (renal infarct, mesenteric ischaemia, etc.) should raise suspicion of aortic occlusion9495. There are limited data on the ideal therapeutic strategy for AAO in COVID-19 patients96. As per the available literature, COVID-19 patients with a small recent non-obstructing aortic thrombus can be initially managed with therapeutic anticoagulation alone. However, patients with extensive organized obstructing aortic thrombosis should be considered for emergency surgical treatment (thrombectomy or axillo–bifemoral bypass) or catheter-directed thrombolysis, followed by therapeutic anticoagulation9597.
Aspirin is a non-steroidal anti-inflammatory drug with anti-inflammatory, antithrombotic and analgesic properties. Use of low-dose aspirin is currently controversial in COVID-19 patients. However, some studies have reported improved outcomes with aspirin use97. Aspirin is also recommended for the treatment in children with post-COVID multisystem inflammatory syndrome and thrombotic complications98.
Treatment of VTE in COVID-19 patients
Low molecular weight heparin (LMWH) has advantages over unfractionated heparin (UFH) and direct oral anti coagulants (DOACs) in the hospitalized COVID-19 patients. Optimization of therapeutic UFH requires that continuity of infusion is maintained and regular blood sampling for activated partial thromboplastin time (aPTT) is performed. UFH may repeatedly expose the healthcare workers to the patient and hence shall not be practicable in the COVID-19 setting. In contrast to warfarin, DOACs does not require regular monitoring. Hence, these shall be the preferred choice in the post-discharge period and the same shall significantly reduce the subsequent healthcare contact. The summary of VTE prevention and treatment is described in Table II.
| Clinical scenario | Choice and dosing considerations for anticoagulation# | Intensity and dose of anticoagulant | Duration |
|---|---|---|---|
| VTE prophylaxis in non-critically-ill COVID-19 patients (general ward) | Preference order: LMWH/fonda > UFH > DOAC Prefer UFH if CrCl <30 ml/min Prefer intermediate-dose if weight >100 kg/BMI >30 kg/m2 50% dose reduction if platelet count <50×109/l Stop anticoagulation if platelet count <25×109/l |
Standard-dose prophylaxis: Enoxaparin 40 mg s.c. OD UFH 5000 units s.c. BID/TID Fondaparinux 2.5 mg s.c. OD Rivaroxaban 10 mg PO OD Apixaban 2.5 mg PO OD |
Till the length of hospital stay (consider prophylactic anticoagulation at discharge for two weeks in patients at high risk for VTE but low bleeding risk) |
| Intermediate-dose prophylaxis: Enoxaparin 0.5 mg/kg s.c. OD or 40 mg s.c. BID UFH 7500 units s.c. BID/TID Fondaparinux 5 mg s.c. OD |
|||
| VTE prophylaxis in critically-ill COVID-19 patients (ICU) | Preference order: LMWH > UFH > Fonda/DOAC Prefer UFH if CrCl <30 ml/min Prefer intermediate-dose if weight >100 kg/BMI >30 kg/m2 50% dose reduction if platelet count <50×109/l Stop anticoagulation if platelet count <25×109/l |
Intermediate-dose prophylaxis: Enoxaparin s.c. 0.5 mg/kg OD or 40 mg BID UFH 7500 units s.c. BID/TID Fondaparinux 5 mg s.c. OD |
Continue prophylactic anticoagulation at discharge for 2-6 wk in patients with low bleeding risk |
| Therapeutic anticoagulation: Enoxaparin 1 mg/kg s.c. BID UFH IV bolus 80 units/kg followed by infusion at 18 units/kg/h (adjusted according to aPTT) Fondaparinux 7.5 mg s.c. OD Rivaroxaban 20 mg PO OD Apixaban 5 mg PO BID |
|||
| VTE treatment in COVID-19 patients in hospital | Preference order: LMWH > UFH > Fonda > DOAC Prefer UFH if CrCl <30 ml/min 50% dose reduction if platelet count <50×109/l Stop anticoagulation if platelet count <25×109/l |
Therapeutic anticoagulation: Enoxaparin 1 mg/kg s.c. BID UFH IV bolus 80 units/kg followed by infusion at 12-18 units/kg/h (adjusted according to aPTT) fondaparinux 7.5 mg s.c. OD Rivaroxaban 20 mg PO OD Apixaban 5 mg PO BID |
Minimum three months duration |
| VTE treatment in COVID-19 patients after discharge | Preference order: LMWH/DOAC >warfarin | Enoxaparin 1 mg/kg s.c. BID Rivaroxaban 20 mg PO OD Apixaban 5 mg PO BID |
Source: Refs 6466. #Mechanical thromboprophylaxis in patients with absolute contraindications for anticoagulant therapy. VTE, venous thromboembolic; LMWH, low-molecular-weight heparin; UFH, unfractionated heparin; BMI, body mass index; DOAC, direct oral anticoagulants; ICU, intensive care unit; IV, intravenous; BMI, body mass index; aPTT, activated partial thromboplastin time; crcl, creatinine clearance; SC, subcutaneous; OD, once daily; BID, twice daily; TID, three times a day; PO, per oral.
Limitations of the study
In this review, an attempt was made to summarize the contemporary literature on COVID-19–associated coagulation abnormalities and their management. The standard methodology for systematic review and meta-analysis could not be pursued. There is a rapid expansion in literature related to this topic, and it is expected that high-quality studies shall enrich our knowledge pertaining to pathogenesis and management of CAC in the near future.
Gaps in current knowledge
There is no clear consensus on the optimal dose of heparin for thromboprophylaxis. The optimal strategy for the monitoring of anticoagulation is also not yet clear. The role of tissue plasminogen activator in critically-ill COVID-19 patients needs to be defined. There is a need for prospective studies to assess the magnitude of thrombotic risk and optimal duration of thromboprophylaxis after discharge in such patients.
Conclusion
To summarize, COVID-19 is accompanied by a hypercoagulable milieu which is not only distinct from the usual DIC but also has substantially increased VTE risk in the hospitalized patients. Due to paucity of high-quality data pertaining to CAC, it remains an Achilles’ heel in the management of these patients and requires more studies focussed on this aspect. Based on currently available evidence, all hospitalized patients should receive prophylactic anticoagulation. Furthermore, management is rapidly evolving and ongoing trials will throw more light on the effectiveness and safety of anticoagulation strategies.
Financial support & sponsorship: None.
Conflicts of Interest: None.
References
- A novel coronavirus from patients with pneumonia in China, 2019. N Engl J Med. 2020;382:727-33.
- [Google Scholar]
- World Health Organisation. Weekly epidemiological update on COVID-19 - 25 May & June 2021. Available from: https://www.who.int/publications/m/item/weekly-epidemiological-update-on-covid-19---25-may-2021
- Association of cardiac injury with mortality in hospitalized patients with COVID-19 in Wuhan, China. JAMA Cardiol. 2020;5:802-10.
- [Google Scholar]
- Repurposed antiviral drugs for Covid-19 - Interim WHO solidarity trial results. N Engl J Med. 2021;384:497-511.
- [Google Scholar]
- Chloroquine and hydroxychloroquine for COVID-19: Time to close the chapter. Postgrad Med J 2020 doi: 10.1136/postgradmedj-2020-138585
- [Google Scholar]
- Confirmation of the high cumulative incidence of thrombotic complications in critically ill ICU patients with COVID-19: An updated analysis. Thromb Res. 2020;191:148-50.
- [Google Scholar]
- Clinical Characteristics of Coronavirus Disease 2019 in China. N Engl J Med. 2020;382:1708-20.
- [Google Scholar]
- Anticoagulant treatment is associated with decreased mortality in severe coronavirus disease 2019 patients with coagulopathy. J Thromb Haemost. 2020;18:1094-9.
- [Google Scholar]
- World Health Organization. Geneva (Switzerland): World Health Organization; 2003 Summary of probable SARS cases with onset of illness from 1 November 2002 31 July 2003. Available from: https://www.who.int/csr/sars/country/table2004_04_21/en
- World Health Organization. Middle East Respiratory Syndrome Coronavirus (MERS-CoV). Available from: http://www.who.int/emergencies/mers-cov/en/
- Analysis of deaths during the severe acute respiratory syndrome (SARS) epidemic in Singapore: Challenges in determining a SARS diagnosis. Arch Pathol Lab Med. 2004;128:195-204.
- [Google Scholar]
- Large artery ischaemic stroke in severe acute respiratory syndrome (SARS) J Neurol. 2004;251:1227-31.
- [Google Scholar]
- A major outbreak of severe acute respiratory syndrome in Hong Kong. N Engl J Med. 2003;348:1986-94.
- [Google Scholar]
- Predictive model of diagnosing probable cases of severe acute respiratory syndrome in febrile patients with exposure risk. Ann Emerg Med. 2004;43:1-5.
- [Google Scholar]
- Middle east respiratory syndrome coronavirus causes multiple organ damage and lethal disease in mice transgenic for human dipeptidyl peptidase 4. J Infect Dis. 2016;213:712-22.
- [Google Scholar]
- Epidemiological, demographic, and clinical characteristics of 47 cases of Middle East respiratory syndrome coronavirus disease from Saudi Arabia: A descriptive study. Lancet Infect Dis. 2013;13:752-61.
- [Google Scholar]
- COVID-19 and its implications for thrombosis and anticoagulation. Blood. 2020;135:2033-40.
- [Google Scholar]
- Coagulation abnormalities and thrombosis in patients with COVID-19. Lancet Haematol. 2020;7:e438-40.
- [Google Scholar]
- COVID-19-related severe hypercoagulability in patients admitted to intensive care unit for acute respiratory failure. Thromb Haemost. 2020;120:998-1000.
- [Google Scholar]
- Endothelial cells orchestrate COVID-19 coagulopathy. Lancet Haematol. 2020;7:e553-e555.
- [Google Scholar]
- Cardiovascular manifestations of COVID-19: An evidence-based narrative review. Indian J Med Res. 2021;153:7-16.
- [Google Scholar]
- Mechanisms of stroke and the role of anticoagulants in COVID-19. J Formos Med Assoc. 2020;119:1721-2.
- [Google Scholar]
- A review of cardiac manifestations and predictors of outcome in patients with COVID-19. Heart Lung. 2020;49:848-52.
- [Google Scholar]
- Venous thromboembolism in COVID-19: Towards an ideal approach to thromboprophylaxis, screening, and treatment. Curr Cardiol Rep. 2020;22:52.
- [Google Scholar]
- Acute pulmonary embolism: An unseen villain in COVID-19. Indian Heart J. 2020;72:218-9.
- [Google Scholar]
- Acute pulmonary embolism associated with COVID-19 pneumonia detected with pulmonary CT angiography. Radiology. 2020;296:E186-8.
- [Google Scholar]
- Pulmonary embolism in patients with COVID-19: Awareness of an increased prevalence. Circulation. 2020;142:184-6.
- [Google Scholar]
- Pulmonary vascular endothelialitis, thrombosis, and angiogenesis in Covid-19. N Engl J Med. 2020;383:120-8.
- [Google Scholar]
- Intussusceptive angiogenesis: Expansion and remodeling of microvascular networks. Angiogenesis. 2014;17:499-509.
- [Google Scholar]
- Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: A descriptive study. Lancet. 2020;395:507-13.
- [Google Scholar]
- Incidence of thrombotic complications in critically ill ICU patients with COVID-19. Thromb Res. 2020;191:145-147.
- [Google Scholar]
- Incidence of venous thromboembolism in hospitalized patients with COVID-19. J Thromb Haemost. 2020;18:1995-2002.
- [Google Scholar]
- Clotting factors in COVID-19: Epidemiological association and prognostic values in different clinical presentations in an Italian Cohort. J Clin Med. 2020;9:1371.
- [Google Scholar]
- Abnormal coagulation parameters are associated with poor prognosis in patients with novel coronavirus pneumonia. J Thromb Haemost. 2020;18:844-7.
- [Google Scholar]
- COVID-19 and thrombotic or thromboembolic disease: Implications for prevention, antithrombotic therapy, and follow-up: JACC state-of-the-art review. J Am Coll Cardiol. 2020;75:2950-73.
- [Google Scholar]
- Clinical course and outcomes of critically ill patients with SARS-CoV-2 pneumonia in Wuhan, China: A single-centered, retrospective, observational study. Lancet Respir Med. 2020;8:475-81.
- [Google Scholar]
- Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395:497-506.
- [Google Scholar]
- Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: A retrospective cohort study. Lancet. 2020;395:1054-62.
- [Google Scholar]
- Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus-infected pneumonia in Wuhan, China. JAMA. 2020;323:1061-9.
- [Google Scholar]
- Thromboinflammation and the hypercoagulability of COVID-19. J Thromb Haemost. 2020;18:1559-61.
- [Google Scholar]
- Pulmonary post-mortem findings in a series of COVID-19 cases from northern Italy: A two-centre descriptive study. Lancet Infect Dis. 2020;20:1135-40.
- [Google Scholar]
- Autopsy findings and venous thromboembolism in patients with COVID-19: A prospective cohort study. Ann Intern Med. 2020;173:268-77.
- [Google Scholar]
- Postmortem findings in Italian patients with COVID-19: A descriptive full autopsy study of cases with and without comorbidities. J Infect Dis. 2020;222:1807-15.
- [Google Scholar]
- Pulmonary and cardiac pathology in African American patients with COVID-19: An autopsy series from New Orleans. Lancet Respir Med. 2020;8:681-6.
- [Google Scholar]
- COVID-19 pulmonary pathology: A multi-institutional autopsy cohort from Italy and New York City. Mod Pathol. 2020;33:2156-68.
- [Google Scholar]
- Pulmonary pathology of COVID-19: A review of autopsy studies. Curr Opin Pulm Med. 2021;27:184-92.
- [Google Scholar]
- SARS-CoV-2 cell entry depends on ACE2 and TMPRSS2 and is blocked by a clinically proven protease inhibitor. Cell. 2020;181:271-80.e8.
- [Google Scholar]
- Functional assessment of cell entry and receptor usage for SARS-CoV-2 and other lineage B betacoronaviruses. Nat Microbiol. 2020;5:562-9.
- [Google Scholar]
- Vasculopathy and coagulopathy associated with SARS-CoV-2 infection. Cells. 2020;9:1583.
- [Google Scholar]
- Clinical and immunological features of severe and moderate coronavirus disease 2019. J Clin Invest. 2020;130:2620-9.
- [Google Scholar]
- More on COVID-19 coagulopathy in Caucasian patients. Br J Haematol. 2020;189:1060-1.
- [Google Scholar]
- Unraveling the mystery of COVID-19 cytokine storm: From skin to organ systems. Dermatol Ther. 2020;33:e13859.
- [Google Scholar]
- The pathogenesis and treatment of the 'Cytokine Storm'in COVID-19. J Infect. 2020;80:607-13.
- [Google Scholar]
- Clinical predictors of mortality due to COVID-19 based on an analysis of data of 150 patients from Wuhan, China. Intensive Care Med. 2020;46:846-8.
- [Google Scholar]
- Aetiology, outcomes and predictors of mortality in acute respiratory distress syndrome from a tertiary care centre in north India. Indian J Med Res. 2016;143:782-92.
- [Google Scholar]
- Endotheliopathy in COVID-19-associated coagulopathy: Evidence from a single-centre, cross-sectional study. Lancet Haematol. 2020;7:e575-82.
- [Google Scholar]
- Coagulopathy, endothelial dysfunction, thrombotic microangiopathy and complement activation: Potential role of complement system inhibition in COVID-19. J Thromb Thrombolysis. 2021;51:657-62.
- [Google Scholar]
- Exploring traditional and nontraditional roles for thrombomodulin. Blood. 2018;132:148-58.
- [Google Scholar]
- Prevention, diagnosis and treatment of venous thromboembolism in patients with COVID-19: CHEST Guideline and Expert Panel Report. Chest. 2020;158:1143-63.
- [Google Scholar]
- Scientific and Standardization Committee communication: Clinical guidance on the diagnosis, prevention, and treatment of venous thromboembolism in hospitalized patients with COVID-19. J Thromb Haemost. 2020;18:1859-65.
- [Google Scholar]
- Ministry of Health and Family Welfare (Government of India). Available from: https://www.mohfw.gov.in/pdf/UpdatedClinicalManagementProtocolforCOV ID19dated03072020.pdf
- Blood coagulation in immunothrombosis-At the frontline of intravascular immunity. Semin Immunol. 2016;28:561-9.
- [Google Scholar]
- Herpesviruses and heparan sulfate: An intimate relationship in aid of viral entry. J Clin Invest. 2001;108:503-10.
- [Google Scholar]
- Heparin prevents Zika virus induced-cytopathic effects in human neural progenitor cells. Antiviral Res. 2017;140:13-7.
- [Google Scholar]
- Anti-inflammatory effects of heparin and its derivatives: A systematic review. Adv Pharmacol Sci 2015 2015 507151
- [Google Scholar]
- The anti-inflammatory effects of heparin and related compounds. Thromb Res. 2008;122:743-52.
- [Google Scholar]
- Heparin, heparan sulfate and heparanase in inflammatory reactions. Thromb Haemost. 2009;102:823-8.
- [Google Scholar]
- More than an anticoagulant: Do heparins have direct anti-inflammatory effects? Thromb Haemost. 2017;117:437-44.
- [Google Scholar]
- Characterization of the heparin-binding properties of IL-6. J Immunol. 2000;165:5671-9.
- [Google Scholar]
- Extracellular histones are major mediators of death in sepsis. Nat Med. 2009;15:1318-21.
- [Google Scholar]
- Protective effects of heparin on endothelial cells in sepsis. Int J Clin Exp Med. 2015;8:5547-52.
- [Google Scholar]
- Cardiovascular considerations for patients, health care workers, and health systems during the COVID-19 pandemic. J Am Coll Cardiol. 2020;75:2352-71.
- [Google Scholar]
- COVID-19 presented with deep vein thrombosis: An unusual presenting. J Investig Med High Impact Case Rep. 2020;8 2324709620931239
- [Google Scholar]
- Cerebral venous sinus thrombosis as a presentation of COVID-19. Eur J Case Rep Intern Med. 2020;7:001691.
- [Google Scholar]
- Prevention of VTE in nonsurgical patients: Antithrombotic Therapy and Prevention of Thrombosis, 9th ed: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines. Chest. 2012;141:S195-226.
- [Google Scholar]
- American Society of Hematology 2018 guidelines for management of venous thromboembolism: Prophylaxis for hospitalized and nonhospitalized medical patients. Blood Adv. 2018;2:3198-225.
- [Google Scholar]
- Clinical characteristics of coronavirus disease 2019 (COVID-19) in China: A systematic review and meta-analysis. J Infect. 2020;80:656-65.
- [Google Scholar]
- Attention should be paid to venous thromboembolism prophylaxis in the management of COVID-19. Lancet Haematol. 2020;7:e362-3.
- [Google Scholar]
- Postdischarge thrombosis and hemorrhage in patients with COVID-19. Blood. 2020;136:1342-6.
- [Google Scholar]
- A risk assessment model for the identification of hospitalized medical patients at risk for venous thromboembolism: the Padua Prediction Score. JTH. 2010;8:2450-7.
- [Google Scholar]
- A proposal for staging COVID-19 coagulopathy. Res Pract Thromb Haemost. 2020;4:731-6.
- [Google Scholar]
- Fibrinolytic therapy for refractory COVID-19 acute respiratory distress syndrome: Scientific rationale and review. Res Pract Thromb Haemost. 2020;4:524-31.
- [Google Scholar]
- Practical diagnosis and treatment of suspected venous thromboembolism during COVID-19 pandemic. J Vasc Surg Venous Lymphat Disord. 2020;8:526-34.
- [Google Scholar]
- Arterial thrombosis in coronavirus disease 2019 patients: A rapid systematic review. Ann Vasc Surg. 2021;70:273-81.
- [Google Scholar]
- Concomitant acute aortic thrombosis and pulmonary embolism complicating COVID-19 pneumonia. Diagn Interv Imaging. 2020;101:321-2.
- [Google Scholar]
- 4 cases of aortic thrombosis in patients with COVID-19. JACC Case Rep. 2020;2:1397-401.
- [Google Scholar]
- Unusual arterial thrombotic events in Covid-19 patients. Int J Cardiol. 2021;323:281-4.
- [Google Scholar]
- Abdominal aortic thrombosis complicating COVID-19 pneumonia. Ann Vasc Surg. 2020;67:8-9.
- [Google Scholar]
- Aspirin use is associated with decreased mechanical ventilation, ICU admission, and in-hospital mortality in hospitalized patients with COVID-19. Anesth Analg. 2021;132:930-41.
- [Google Scholar]
- Childhood multisystem inflammatory syndrome: An emerging disease with prominent cardiovascular involvement –A scoping review. SN Compr Clin Med 2021 doi: 10.1007/s42399-020-00650-0
- [Google Scholar]






