Translate this page into:
Clinical significance of magnetic resonance imaging findings in chronic low backache
Reprint requests: Dr. Jayantee Kalita, Department of Neurology, Sanjay Gandhi Post Graduate Institute of Medical Sciences, Raebareily Road, Lucknow 226 014, Uttar Pradesh, India e-mail: jayanteek@yahoo.com
-
Received: ,
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Background & objectives:
Magnetic resonance imaging (MRI) is frequently done for the evaluation of chronic low backache (CLBA), however, its significance in Indian patients has not been evaluated. We report here the MRI findings in patients with CLBA and their sensitivity and specificity with clinical evidence of radiculopathy and localized CLBA as well as correlate these with pain severity and disability.
Methods:
Seventy two patients with CLBA aged 20-70 yr without trauma, infection, tumour, metastasis and vascular malformation were included in the study. Their demographic characteristics, lifestyle, education and employment were noted. Lumbosacral MRI was carried out and 19 MRI parameters at six levels (D12-L1-L5-S1) were noted. The severity of pain was assessed by Numeric Rating Scale (NRS, 0-10) and disability by Oswestry Disability Index (ODI).
Results:
MRI was abnormal in all patients, the most common being disc desiccation (90.3%) followed by facet joint arthropathy (FJA; 75%) and nerve root compression (NRC; 72.2%). Endplate changes and high-intensity zone were noted in 58 and 50 per cent of patients, respectively. One-third patients with FJA, however, were below 30 yr of age. NRC on MRI had 61.3 per cent sensitivity and 10 per cent specificity with clinical radiculopathy. FJA had 60.7 per cent sensitivity and 15.9 per cent specificity with localized CLBA. None of the MRI parameters and MRI sum score correlated with NRS and ODI. On multivariate analysis, NRS was independent predictor of ODI (odds ratio 0.58, 95% confidence interval 0.35-0.98, P=0.04).
Interpretation & conclusions:
In patients with CLBA, NRC on MRI showed poor specificity with corresponding clinical radiculopathy and FJA with localized backache. None of the MRI abnormality correlated with the severity of pain or disability.
Keywords
Disability
facet joint arthropathy
high-intensity zone
low backache
magnetic resonance imaging
nerve root compression
Oswestry disability index
radiculopathy
Low backache (LBA) is a common morbidity in the population, and it is the fifth common cause of visiting a physician in the USA1. About 25 per cent adults in the USA report LBA for one day in three months. One-third of them have persistent LBA for one year, and 1-5 per cent report persistent limitation in activity. LBA results in loss of productivity, absence from work and expenditure related to treatment. The severe LBA limits work performance or self-care resulting in disability in 11-76 per cent patients2. The wide variability in disability is due to use of different patient population and use of different scale for the measurement of disability.
Computed tomography, discography and magnetic resonance imaging (MRI) have been used for correlating the clinical symptoms and signs in chronic LBA (CLBA). Corresponding radiological findings explaining the clinical symptoms and signs help in the treatment decision. There is however, a poor correlation of MRI findings with clinical signs in the patients with LBA, and similar MRI changes may also be present in asymptomatic individuals34. The presence of high-intensity zone (HIZ) on MRI has been reported to correlate with pain severity in the patients with CLBA5. In these patients, MRI reveals various findings such as disc desiccation, disc bulge, nerve root compression (NRC), facet joint arthropathy (FJA) and ligamentum flavum hypertrophy. About 95 per cent of disc lesions are at L4-L5 or L5-S1 level6, and the most common site of FJA is at L4-L5 level7. Disc disease and FJA have been reported in CLBA, but conglomeration of various MRI findings may determine the severity and disability which have not been reported. Moreover, the demographic and MRI findings in CLBA may be different in Indian patients because of geocultural and genetic reasons. Therefore, we report here the MRI findings in patients with CLBA and correlate these with neurological findings, pain severity and disability.
Material & Methods
This study was conducted in the department of Neurology, Sanjay Gandhi Post Graduate Institute of Medical Sciences, Lucknow, India, during March 2012 to April 2013 and the patients were recruited from the out-patient service. Seventy two consecutive patients with CLBA were included in this study who participated in a randomized control trial on efficacy of amitriptyline versus pregabalin in CLBA in the same department8. The CLBA was considered if the pain lasted for three months or more in the absence of infection, autoimmune, trauma and malignancy9. The study was approved by the Ethical Committee of the institute (PGI/BE/193/2012).
The patients with CLBA due to specific cause such are trauma, malignancy, collagen vascular disease, rheumatoid or seronegative arthritis, vascular malformation and spinal tumours were excluded. Patients on corticosteroid were also excluded from the study. In total, 17 patients were excluded; due to malignancy in five, Pott's spine in four, seronegative arthritis in two, knee joint osteoarthritis in two and rheumatoid arthritis, Parkinson's disease, osteoporotic collapse and chronic liver disease in one patient each.
Clinical evaluation: The demographic details of the patients including age, gender and area of residence, lifestyle, smoking, alcohol, tobacco and dietary habit were collected. Education (number of years) and occupation of the individual were noted. The duration of CLBA, its location, radiation to particular nerve root and its aggravating and relieving factors were also noted. The presence of sensory motor deficit in the lower limbs as well as any change in bowel and genitourinary functions were also enquired. A detailed medical examination including anaemia, oedema, skeletal deformity, lymphadenopathy and hepatosplenomegaly was done. A detailed neurological examination was also done. Presence of muscle wasting, fasciculation, muscle power, tendon reflexes and impairment of pinprick, touch, joint position and vibration was recorded. Straight leg raising (SLR) test was done and considered positive if there was pain between 30° and 70° elevation10. On the basis of clinical history and examination, the patients were categorized into three categories: (i) Localized LBA; (ii) LBA with radiculopathy; and (iii) Lumbar canal stenosis.
Assessment of pain severity and disability: The severity of pain was assessed by Numeric Rating Scale (NRS) which is a 0-10 scale, 0 being no pain and 10 worst pain. This was categorized into mild (1-3), moderate (4-6) and severe (7-10)11. For measuring disability, Oswestry Disability Index (ODI) was used12. Based on the ODI score, the disability of the patients was categorized into minimal (0-20%), moderate (21-40%), severe (41-60%), crippled (61-80%) and bed bound (81-100%).
Investigations: Blood counts, erythrocyte sedimentation rate at first hour, haemoglobin, fasting blood sugar, serum creatinine, sodium, potassium, calcium, phosphorous, alkaline phosphatase, serum bilirubin, transaminases, protein and albumin were done in all the patients. Hydroxy vitamin D and thyroid function test were carried out in the patients in whom osteomalacia and hypothyroidism, respectively, were clinically suspected13.
Spinal magnetic resonance imaging (MRI): Spinal MRI of the lumbosacral region was performed using the 3TMRI machine (GE medical system, Wisconsin, USA). Sagittal images were obtained in both T1 FSE (TE 20-40 TR 400-600) and T2 FSE (TE-96, TR 4000, Flip angle 25) sequence. Axial images were obtained in T2 sequence parallel to intervertebral disc. Sagittal images were obtained at 4 mm slice thickness with 0.3 mm interslice gap. Coronal STIR images were used for the evaluation of sacroiliac joints. Six vertebral segments including D12-L1 to L5-S1 were evaluated for documenting the following parameters of anterior and posterior elements according to Milette et al14.
Anterior elements:
-
(i)
Normal disc hyperintensity: Brightest signal intensity on T2WI in the central four-fifths of D12-L1 and L1-L2 disc was considered normal standard for each patient4.
-
(ii)
Disc desiccation: Complete loss of central hyperintensity was considered Grade II and some residual hyperintensity as Grade I.
-
(iii)
Reduction in disc height in comparison of adjacent normal appearing disc height.
-
(iv)
Diffuse annular bulge was considered if circumferential disc extended beyond the adjacent vertebral body margin.
-
(v)
Disc protrusion was considered if there was displacement of nucleus pulposus through annulus fibrosus with a narrow edge and broad base.
-
(vi)
Disc extrusion was considered if the disc had extended through all layers of the annulus with a broader edge than the base which was attached to the parent disc.
-
(vii)
Disc sequestration was considered if the disc fragment was no longer in continuity with the parent disc material.
-
(viii)
HIZ: High-intensity signal that was located in the substance of the posterior annulus fibrosus which was clearly dissociated from the nucleus pulposus.
Posterior element:
-
(i)
FJA was considered if there was reduced joint space, loss of T2 hyperintensity or hyperarticular marginal hypertrophy.
-
(ii)
NRC was considered if there was reduced neural foramen (normal measurement for neural foramina is taken as 4 mm). NRC was categorized as Grade I (loss of available space), Grade II (abutment of adjacent neural elements) and Grade III (compression, altered signal of the neural element)15.
-
(iii)
Anterior and posterior marginal osteophytes.
-
(iv)
Ligamentum flavum hypertrophy: If the thickness of ligamentum flavum was >5 mm4.
-
(v)
Spondylolysis: Abnormal signal changes or discontinuity in the pars inter-articularis was looked for evaluating spondylolysis.
-
(vi)
Spondylolisthesis: Meyerding classification was used for spondylolisthesis16.
-
(vii)
Anterior-posterior diameter: This was measured from the posterior margin of the intervertebral disc to the spinolaminar junction at each level. Considered stenosed when it was <11.5 mm17.
Endplate changes: These were evaluated as per Modic et al18 classification and Schmrol nodes were also noted.
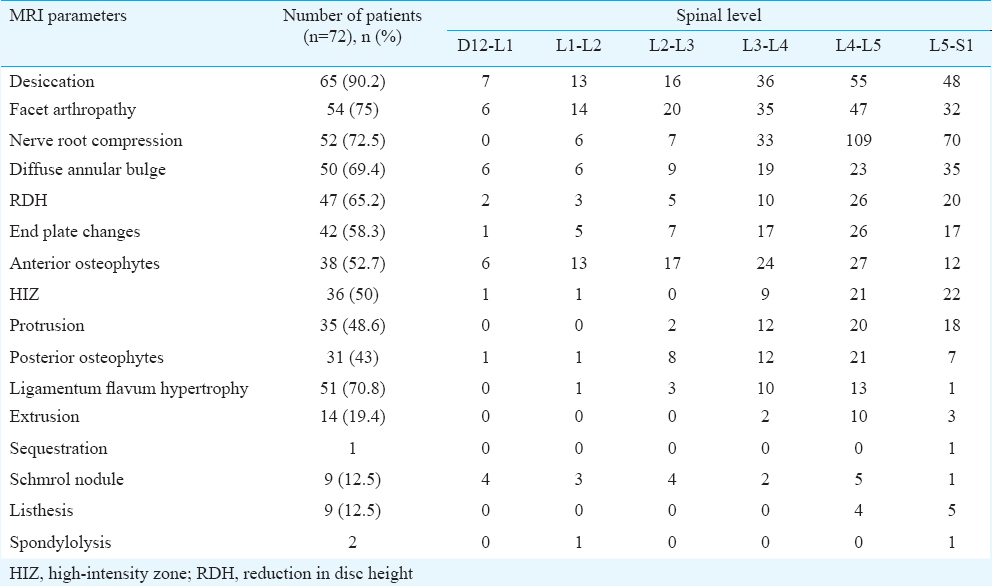
A total of 114 (19×6, including facet joint, NRC of both the sides) parameters in each patient were evaluated. Subsequently, the number of FJA, disc protrusion and HIZ in an individual patient was noted (Fig. 1). A total sum score including the above-mentioned MRI abnormalities in an individual patient was calculated for correlating MRI burden with severity of pain and disability.

- (A) T2W sagittal section shows L5-S1 disc bulge (arrow), (B) T2W axial section shows L5-S1 level disc extrusion (arrow), (C) T2W axial section shows narrowing of spinal canal at multiple levels (arrow), (D) T2W sagittal section shows L3-L4 disc protrusion and high intensity zone (arrow), (E) T2W sagittal section shows L5-S1 listhesis (arrow), (F) T1W sagittal section shows Schmrol nodule at L3-L4 (arrow), (G) T2W sagittal section shows right nerve root compression at L3-L4 level (arrow), (H) T2W axial section shows L4-L5 ligamentum flavum hypertrophy and facet joint arthropathy (arrow).
The clinical categorization of the CLBA (radiculopathy and localized) and MRI findings were correlated in the individual patient and grouped as corresponding and non-corresponding radiological findings in relation to clinical categorization. Patients were treated with amitriptyline (25-50 mg) daily or pregabalin 150 mg to 300 mg twice daily. Reduction in pain severity by 50 per cent on NRS and disability by 20 per cent on ODI was considered improvement.
Statistical analysis: The sensitivity and specificity of NRC on MRI with corresponding clinical radiculopathy was evaluated. The baseline and follow up NRS and ODI scores were correlated with various MRI parameters using Karl-Pearson correlation test. Improvement following different treatment protocol was evaluated by Chi-square test. All tests were done using SPSS version 12 software (SPSS Inc, Chicago, USA).
Results
The median age of the 72 patients with CLBA was 41 (22-70) yr and 39 (54.2%) were females. Majority of the patients were in the third and fourth decades of their life (28; 39%) and 41 (57%) were from rural areas of Uttar Pradesh and Bihar. Thirty five (48.6%) patients were sedentary, 30 (41.7%) light and seven (9.7%) were heavy workers; 16 (22.2%) patients were smoker and 27 (37.5%) were tobacco chewer. Fifteen patients were lactovegetarian. The median duration of backache was 24 (3.5-360) months. Pain occurred after standing or walking for some time in eight patients suggesting lumbar canal stenosis. Backache radiating to heel or sole was present in 38 patients. On examination, SLR test was positive in 17 (23.6%) patients and localized tenderness in the lumbosacral region in 10 patients. L5 and S1 radicular sensory deficit was present in five patients and 13 had paresthesia. Thirty patients had radiation of pain to L5S1 distribution, 12 patients had more than two dermatomal involvement and two patients had L4-L5 distribution pain. Motor deficit in the form of mild weakness of extensor halluces longus and tibialis posterior and ankle reflex loss was present in 10 patients. On the basis of clinical history and examination, the patients were categorized into localized CLBA (n=28) and CLBA with radiculopathy (including lumbar canal stenosis, n=44). The severity of pain was mild in two, moderate in 37 and severe in 33 patients. The median NRS score was 6 (2-10). The median ODI score was 38 (16-80). CLBA resulted in mild disability in two, moderate in 37, severe in 26 and seven patients were crippled. Females had more disability compared to males (P=0.001). Nine patients were diabetic, 15 hypertensive and 33 anaemic (<12 g/dl Hb). One patient had hypocalcaemia (8.5 mg/dl) and 34 had elevated alkaline phosphatase (>150 U/l).
Magnetic resonance imaging (MRI) findings: MRI abnormalities were detected in all the patients. The most common MRI abnormality was disc desiccation (n=65, 90.2%) followed by FJA (n=54, 75%) and NRC (n=52, 72.5%). The details are summarized in Table I. The anterior segment abnormalities were more common than posterior segment. Majority of the patients had MRI lesions at multiple sites. The number of NRC in a patient ranged between 0-9 (median 2) and FJA 0-11 (median 3). The frequency of FJA increased with increasing age. The most common site of disc desiccation, NRC and FJA was at L4/5 level. The association of age and frequency of various MRI findings is presented in Table II.

Clinico-radiological correlation: The sensitivity of MRI evidence of NRC with corresponding clinical evidence of radiculopathy was 61.3 per cent and specificity 10 per cent. Of the 44 patients with clinical radiculopathy, 27 had NRC on MRI. The sensitivity of FJA with localized CLBA was 60.7 per cent and specificity 15.9 per cent. Of the 28 localized LBA, only 17 had MRI evidence of FJA.
The severity of pain (NRS score) did not correlate with number of disc lesion (r=0.12, P=0.32), number of NRC (r=0.01, P=0.95), HIZ (r=0.05, P=0.67) and total number of MRI lesions (r=−0.1, P=0.40). The severity of pain also did not correlate with age (r=−0.021, P=0.85) and duration of illness (r=0.009, P=0.93). The ODI score did not correlate with number of disc lesion (r=0.10, P=0.43), NRC (r=0.08, P=0.48), HIZ (r=0.17, P=0.14) and total MRI lesions (r=−0.13, P=0.32). The ODI score also did not correlate with duration illness (r=0.22, P=0.07) and age of the patients (r=0.12, P=0.33). ODI however, correlated with severity of pain (r=0.35, P=0.005) and gender (r=0.42; P<0.001; Fig. 2). On multivariate analysis, the severity of pain was independent predictor of disability (odds ratio 0.58, 95% confidence interval 0.35-0.98; P=0.04).
![(A) Regression curve shows significant correlation of severity of pain [Numeric Rating Scale (NRS) score] and Oswestry Disability Index (ODI) score. (B) Error bar diagram shows Oswestry Disability Index (ODI) score in males and females (***P<0.001).](/content/175/2017/145/6/img/IJMR-145-796-g004.png)
- (A) Regression curve shows significant correlation of severity of pain [Numeric Rating Scale (NRS) score] and Oswestry Disability Index (ODI) score. (B) Error bar diagram shows Oswestry Disability Index (ODI) score in males and females (***P<0.001).
Thirty eight patients received amitriptyline (35-50 mg/day) and 34 pregabalin (300-600 mg/day). At three months, the improvement in pain severity (22 vs. 16; P=0.48) and disability (28 vs. 21; P=0.32) was not significantly different between amitriptyline and pregabalin groups. The improvement in pain did not correlate significantly with MRI evidence of NRC (r=0.23; P=0.07), HIZ (r=0.06; P=0.60) and endplate changes (r=0.19; P=0.11). Improvement in disability also did not correlate with NRC (r=0.13; P=0.29), HIZ (r=0.19; P=0.60) and endplate changes (r=0.13; P=0.29). FJA correlated significantly with improvement in pain (r=0.32; P=0.007) and disability (r=0.33; P=0.004). Disc desiccation correlated with improvement in pain (r=0.29; P=0.01) and disability (r=0.23; P=0.05).
Discussion
The most common MRI changes in our patients with CLBA were disc desiccation occurring in 90.3 per cent followed by FJA (75%) and NRC (72.2%). The MRI evidence of disc desiccation, FJA and NRC were most common at L4-L5 level compared to other levels and the frequency of MRI changes increased with age. None of the demographic, clinical and MRI parameters correlated with pain severity and disability, but gender and severity of pain correlated with disabilities. The L4-L5 level was found to be the most common site of disc changes, FJA and NRC. In the study by Deyo et al6, 95 per cent of lumbar disc herniations were in L4-L5 and L5-S1 levels. We have found early development of FJA and disc disease occurring from third decade onward although the frequency of radiological changes increased with increasing age suggesting degenerative pathology. In a study from the USA, the MRI evidence of disc protrusion and bulges was highest in the fifth and sixth decades3. The importance of FJA was evaluated in a study on 188 patients who had MRI evidence of FJA, and their self-reported occurrence of LBA in next 12 months was collected. In this study, there was no association of LBA with FJA. The frequency of FJA was highest (89.2%) in 60-69 yr and lowest (24%) below 40 yr of age. The overall FJA in male was 59.6 per cent and in female was 66.7 per cent7. In our study evidence of FJA was found in 75 per cent patients and of these, 37.5 per cent were <30 yr of age. The high frequency of FJA in our study might be due to inclusion of patients with CLBA whereas the above-mentioned study evaluated the FJA without occurrence of backache. An autopsy study of lumbar spine on 647 cadavers revealed evidence of FJA in 50 per cent who were less than 30 yr of age and the most common site was L4-L519. In the present study, patient with FJA and disc desiccation had significant improvement in the pain after treatment with pregabalin and amitriptyline which could be due to attenuation of mechanical hyperalgesia and reduction of frequency of evoked neuronal firing. In the central nervous system, pregabalin exhibits potent anticonvulsant, analgesic and anxiolytic activity. Potent binding to the α2-δ ligand site reduces depolarization-induced calcium influx with a consequential modulation in excitatory neurotransmitter release20.
Modic et al18 evaluated degenerative disc disease and its correlation with vertebral marrow changes in 474 patients referred for lumbar MRI. Four per cent patients had type 1 (decreased T1 and increased T2 signal intensity) and 16 per cent type 2 (increased T1 and decreased T2 signal intensity) endplate changes. MRI was repeated after 14 months to three years in 16 patients and revealed change of type 1 endplate changes to type 2 in majority whereas type 2 endplate changes remained stable. In our study, higher frequency of endplate changes (58.3%) may be due to inclusion of patients with CLBA and use of higher tesla MRI. The end plate changes described by Modic are the markers of segmental hypermobility and dynamic process21. The dynamic changes of Modic type I endplate changes have been reported in a longitudinal study, which converted to type II or more extensive type I changes over a period of 12-72 months. Deterioration in type I changes correlated with higher visual analogue scale and ODI scores whereas conversion to type II change with lower score22. In another study, lumbar spinal MRI changes were evaluated in individuals exposed to whole body vibration. Individuals with L5-S1 Modic changes were associated with LBA, and the pain was more severe in those with more extensive changes21. In our study, 58 per cent patients had endplate changes which were more prominent at L4-L5 and L5-S1 level and were not correlating with the severity of pain and disability. Berg et al23 also did not find correlation of total MRI score with severity of pain and disability. Disc disease has been reported to correlate poorly with LBA. In a seven-year follow up study, MRI findings did not correlate with the duration of LBA and had poor correlation with clinical parameters24. We found disc desiccation as the most common disc lesion; however, in another study, disc extrusion was common25. This study however, did not evaluate FJA. The initial report on HIZ showed significant correlation with LBA, but later study did not confirm this association26. In the present study also, there was no correlation of MRI findings with NRS and ODI scores. This may be due to chronicity of illness and different characteristics of patient population. We however, have not done longitudinal study to evaluate the later changes.
In our study, clinical evidence of radiculopathy correlated with NRC on MRI highlighting the role of MRI in treatment decision. The disability also correlated with pain severity and gender. Female patients had higher disability compared to males. The reported prevalence of disability in CLBA is a complex and multifactorial phenomenon. One study from Norway reported correlation of disability with severity of pain and other with psychosocial factors, unemployment, low income, depression, fatigue, self-efficacy; high level of fear of pain and more than six hours sitting work27. Lifestyle also has a role in LBA and its disability. In a study on LBA28, 58.5 per cent patients did mild activity, 17.5 per cent moderate activity and 24 per cent strenuous activity. Mild activity and sitting more than six hours/day had 1.9-fold higher risk of CLBA. Patient with LBA had 0.5-fold higher risk of getting disable at one year compared to the normal controls. Overweight individuals had 5.7 times higher risk of developing LBA as compared to normal body mass index28. The higher disability in females may be attributed to prevalence of osteoporosis and nutritional factors which is common in India29. Role of osteoporosis in females with LBA have been reported30.
The major limitation of the present study was less number of patients. Also, BMI, depression, anxiety, inter-rater variability and normal controls were not evaluated. The burden of degenerative disc disease in our study was evaluated by sum score on MRI by adding various changes at different levels in an individual to correlate with pain severity and disability. The sum score on MRI however was not validated.
In conclusion, our study showed that degenerative changes of lumbosacral spine were frequent in patients with CLBA. The most common site was L4-L5 level both for disc disease and FJA. MRI evidence of NRC had poor specificity with corresponding clinical radiculopathy and FJA with localized backache. Disability was higher in females and correlated with severity of pain. Abnormalities detected in MRI were not correlated with either severity of pain or disability. Further study is needed to evaluate the underlying cause of CLBA in females for possible therapeutic strategy.
Conflicts of Interest: None.
References
- Back pain prevalence and visit rates: Estimates from U.S. national surveys, 2002. Spine (Phila Pa 1976). 2006;31:2724-7.
- [Google Scholar]
- Disability related to chronic low back pain: Prevalence and associated factors. Rev Esc Enferm USP. 2012;46:16-23.
- [Google Scholar]
- Magnetic resonance imaging of the lumbar spine in people without back pain. N Engl J Med. 1994;331:69-73.
- [Google Scholar]
- Correlation of clinical presentation, radiography, and magnetic resonance imaging for low back pain – A preliminary survey. J HK Coll Radiol. 2003;6:141-51.
- [Google Scholar]
- High-intensity zone: A diagnostic sign of painful lumbar disc on magnetic resonance imaging. Br J Radiol. 1992;65:361-9.
- [Google Scholar]
- Facet joint osteoarthritis and low back pain in the community-based population. Spine (Phila Pa 1976). 2008;33:2560-5.
- [Google Scholar]
- An open labeled randomized controlled trial of pregabalin versus amitriptyline in chronic low backache. J Neurol Sci. 2014;342:127-32.
- [Google Scholar]
- Chronic low back pain: Evaluation and management. Am Fam Physician. 2009;79:1067-74.
- [Google Scholar]
- Pain: Clinical manual for nursing practice. Baltimore: V.V. Mosby Company; 1993.
- Differentiating lumbar disc protrusions, disc bulges, and discs with normal contour but abnormal signal intensity. Magnetic resonance imaging with discographic correlations. Spine (Phila Pa 1976). 1999;24:44-53.
- [Google Scholar]
- Normal and degenerative posterior spinal structures: MR imaging. Radiology. 1987;165:517-25.
- [Google Scholar]
- MRI of the brain and spine. New York: Lippincott Raven; 1996.
- Degenerative disk disease: Assessment of changes in vertebral body marrow with MR imaging. Radiology. 1988;166(1 Pt 1):193-9.
- [Google Scholar]
- Prevalence of lumbar facet arthrosis and its relationship to age, sex, and race: An anatomic study of cadaveric specimens. Spine (Phila Pa 1976). 2007;32:2058-62.
- [Google Scholar]
- Pregabalin: A novel gamma-aminobutyric acid analogue in the treatment of neuropathic pain, partial-onset seizures, and anxiety disorders. Clin Ther. 2007;29:26-48.
- [Google Scholar]
- Modic changes in endplates of lumbar vertebral bodies: Prevalence and association with low back and sciatic pain among middle-aged male workers. Spine (Phila Pa 1976). 2007;32:1116-22.
- [Google Scholar]
- Longitudinal study of vertebral type-1 end-plate changes on MR of the lumbar spine. Eur Radiol. 2004;14:1574-81.
- [Google Scholar]
- Do more MRI findings imply worse disability or more intense low back pain? A cross-sectional study of candidates for lumbar disc prosthesis. Skeletal Radiol. 2013;42:1593-602.
- [Google Scholar]
- The value of magnetic resonance imaging of the lumbar spine to predict low-back pain in asymptomatic subjects: A seven-year follow-up study. J Bone Joint Surg Am. 2001;83-A:1306-11.
- [Google Scholar]
- Relationship between severity of lumbar disc disease and disability scores in sciatica patients. Neurosurgery. 2002;50:1253-9.
- [Google Scholar]
- Quantitative estimation of the high-intensity zone in the lumbar spine: Comparison between the symptomatic and asymptomatic population. Spine J. 2014;14:391-6.
- [Google Scholar]
- Work-related psychosocial and mechanical risk factors for low back pain: A 3-year follow-up study of the general working population in Norway. Occup Environ Med. 2013;70:296-302.
- [Google Scholar]
- Association between strenuous occupational activity and low back pain. Acta Ortop Mex. 2012;26:21-9.
- [Google Scholar]
- Vitamin D deficiency in rural girls and pregnant women despite abundant sunshine in northern India. Clin Endocrinol (Oxf). 2009;70:680-4.
- [Google Scholar]
- Low back pain associated with sociodemographic factors, lifestyle and osteoporosis: A population-based study. J Rehabil Med. 2013;45:76-80.
- [Google Scholar]






