Translate this page into:
Clinical profile & long-term natural history of symptomatic coronary artery disease in young patients (<30 yr)
For correspondence: Dr Harikrishnan Sivadasanpillai, Department of Cardiology, Sree Chitra Tirunal Institute for Medical Sciences & Technology, Thiruvananthapuram 695 011, Kerala, India e-mail: drharikrishnan@gmail.com
-
Received: ,
This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
This article was originally published by Wolters Kluwer - Medknow and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Background & objectives:
Several studies have shown a high prevalence of cardiovascular risk factors in patients in the age group of 30-74 yr, but there is a paucity of data in young patients below 30 yr. We analyzed the clinical and coronary angiographic profile of patients <30 yr of age with symptomatic coronary artery disease (CAD) and also assessed their intermediate and long-term outcomes.
Methods:
All patients less than 30 yr of age who presented with symptomatic CAD from 1978 to 2017 in the department of Cardiology of a tertiary care hospital in south India, were studied for coronary risk factors and angiographic and treatment patterns, and the follow up data were collected.
Results:
The mean age of the 159 patients <30 yr of age was 26.7±3.29 yr. Male preponderance was observed (91.8%), 63.5 per cent patients were smokers and 88.3 per cent were dyslipidaemic. Acute myocardial infarction was the most common mode of presentation. Forty one per cent patients were non-adherent to medications. Risk factor control was inadequate with respect to smoking cessation, alcoholism, physical activity and dietary regulation. The predictors of long-term mortality were multivessel CAD [hazard ratio (HR): 1.927, 95% confidence interval (CI): 1.003-3.701] and reduction in ejection fraction (EF) (10% decrease in EF; HR: 1.349, 95% CI: 1.096-1.662). Overall mortality was 30 per cent at 10 yr and 48 per cent at 20 yr.
Interpretation & conclusions:
Decreasing EF and multivessel involvement were found to be the strong correlates for long-term mortality in young patients below 30 yr of age with CAD. High long-term mortality rates and poor risk factor control suggest the vast scope for the improvement of outcomes in these patients with aggressive risk factor control.
Keywords
Coronary artery disease
epidemiology
ischaemic heart disease
long-term outcomes
mortality
myocardial infarction
risk factors
young
Coronary artery disease (CAD) is one of the leading causes of death worldwide and is becoming increasingly prevalent in the younger population1. The highest proportions of cases with first myocardial infarction (MI) occurring before the age of 40 yr were observed in the Middle East (12.6%), Africa (10.9%) and South Asia (9.7%)2. Hospital-based studies have shown that patients younger than 40 yr account for 6-16 per cent of patients presenting with acute coronary syndromes345. Data from the young patients with CAD remain scarce, particularly regarding their long-term outcomes. While mortality trends in CAD have shown improvement with time, age-specific mortality rates related to CAD in the young have been flattening67. A large-scale household survey study showed a high prevalence of cardiovascular disease (CVD) risk factors in adults aged 30-74 yr, with the highest CVD risk noted from Kerala, but with no data in those below 30 yr of age8. This study was, therefore, aimed to evaluate the clinical and coronary angiographic profile of patients with CAD <30 yr of age their treatment patterns, and to assess their intermediate and long-term outcomes.
Material & Methods
This was an observational study conducted between January 2013 and December 2017. All patients who had attended the department of Cardiology, Sree Chitra Tirunal Institute for Medical Sciences and Technology (SCTIMST), Thiruvananthapuram, India, with a diagnosis of CAD at less than 30 yr of age, were identified from the hospital database. All consecutive patients from January 1978 to December 2017 who underwent coronary angiography for symptomatic CAD were included in this study. Besides retrospective recruitment, patients were prospectively enrolled from 2013 till the end of the study. Patients who underwent coronary angiography for other indications were excluded, viz., congenital heart disease as part of cardiac catheterization before surgery, hypertrophic cardiomyopathy, restrictive heart disease or constrictive cardiomyopathy. The study was approved by the Ethics Committee of the SCTIMST.
These patients were evaluated for their demographic data and the presence of established conventional risk factors for CAD. Their coronary angiograms were analyzed. Follow up data were obtained during outpatient visits. A significant proportion of patients who had been lost to follow up over the years were traced by telephonic contact, postal enquiries and email with the patients, relatives, health workers and referring physicians. Patients were traced by enquiry with local administrative bodies (panchayats), contacting booth-level officers attached to the Election Commission of India, Integrated Child Development Services (ICDS) workers, health inspectors, junior public health nurses in nearby primary healthcare centres and accredited social health activist (ASHA) workers.
Major adverse cardiovascular and cerebrovascular events (MACCE) rate on follow up was assessed as a composite of mortality, acute coronary syndromes, hospitalization for heart failure, repeat revascularization and cerebrovascular events. Follow up data were obtained on the presence and control of risk factors such as diabetes mellitus, systemic hypertension, dyslipidaemia, smoking and/or tobacco use, obesity, physical inactivity, decreased intake of fruits and vegetables, family history of premature CAD and adherence to medications.
The presence of significant CAD was defined by the presence of 50 per cent narrowing of intraluminal diameter of at least one of the major epicardial coronary arteries on coronary angiography. The inclusion criteria of symptomatic CAD meant to include only patients who either had history of acute coronary syndrome(s) or classical history of angina or typical angina equivalents on exertion to increase specificity for significant CAD.
Statistical analysis: Statistical analysis was done with SPSS v.21.0 (IBM Corp., Armonk, NY, USA). Categorical data were displayed as proportions and continuous data as mean±standard deviation. Pearson's Chi-square test was used for comparison of discrete variables. Fisher's exact test was used for subgroup analysis of categorical data with sample sizes not suitable for Chi-square tests. The independent samples t test was used for between-group comparison of continuous variables. Survival analysis was done using the Kaplan-Meier method, with inter-group comparison by the log-rank test. Logistic regression analysis was also done. Correlates of long-term survival were determined by Cox proportional hazard model analysis. All confidence intervals were calculated to the 95th percentile.
Results
During the 40 yr period (1978-2017), 271 patients <30 yr of age attended the department of Cardiology at the SCTIMST with a diagnosis of CAD. Of these, 159 patients underwent coronary angiography and constituted the study group (Fig. 1).
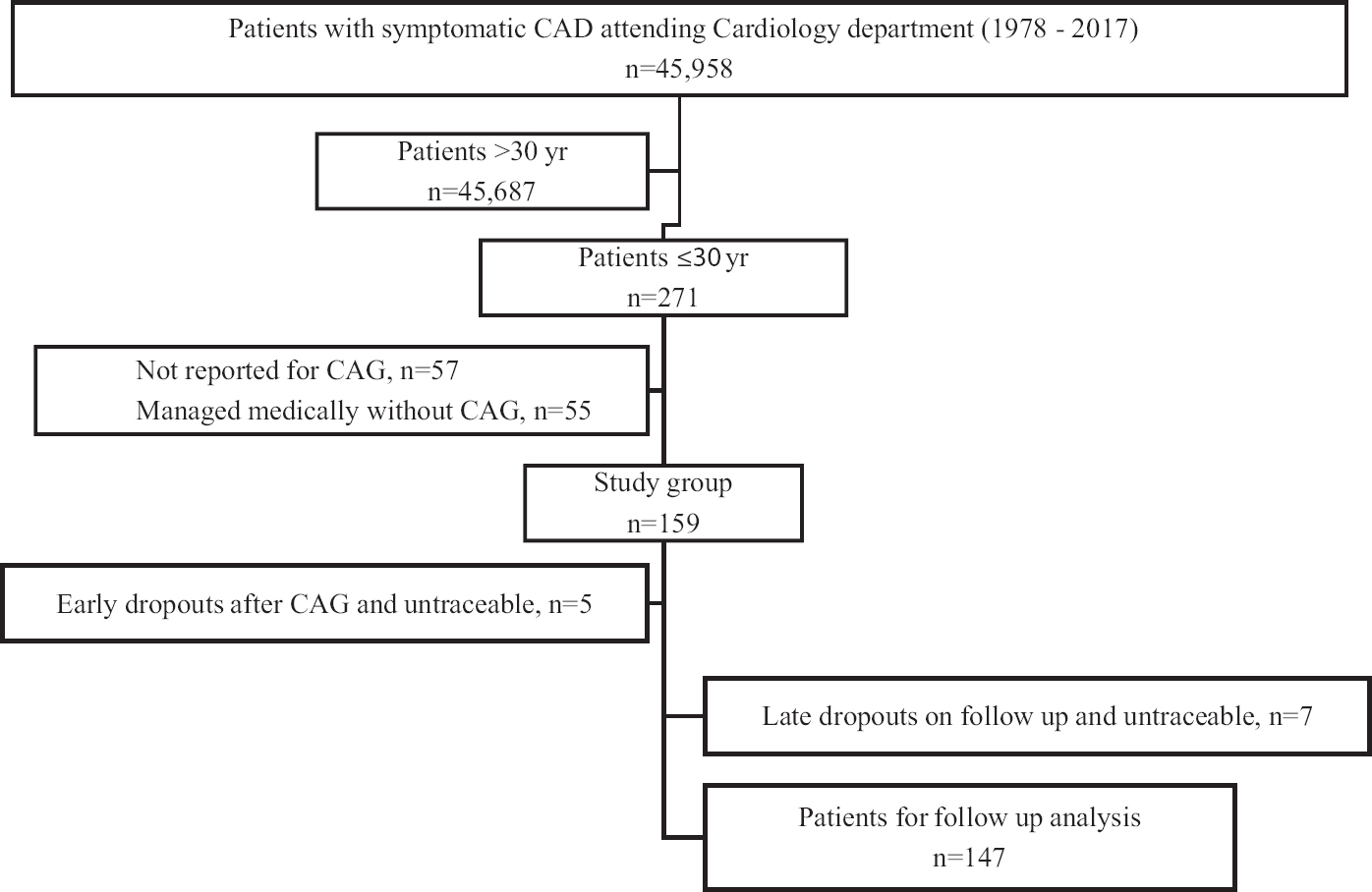
- Flowchart of the study showing inclusion of patients. CAD, coronary artery disease; CAG, coronary angiography.
The baseline clinical characteristics of patients are given in Table I. There was a male preponderance, 146 patients (91.8%). The mean age of the patients was 26.7±3.29 yr. The youngest patient was a 10 yr old boy with Duchenne muscular dystrophy who presented with non-ST elevation myocardial infarction (NSTEMI). Sixty three per cent patients (n=101) were smokers and 88.3 per cent (n=136) were dyslipidaemic. Low levels of high-density cholesterol (HDL) were noted in 79 per cent patients (n=125) and high levels of low-density cholesterol (LDL) in 60 per cent patients (n=95). The mean total cholesterol-to-HDL ratio was 5.6, and the LDL/HDL ratio was 3.76±1.89. Five patients had familial hypercholesterolaemia by Simon Broome's diagnostic criteria9. None of the patients reported a history of recreational drug abuse.
| Parameter | Overall (n=159), n (%) | Men (n=146), n (%) | Women (n=13), n (%) |
|---|---|---|---|
| Age (yr) | 26.6±3.29 | 26.7±3.26 | 26.0±3.63 |
| Current tobacco use | 101 (63.5) | 100 (68.5)*** | 1 (7.7) |
| Family history | 47 (29.6) | 42 (28.8) | 5 (38.5) |
| Dyslipidaemiaδ | 136 (88.3) | 127 (90.1) | 9 (69.2) |
| Systemic hypertension | 14 (8.8) | 12 (8.2) | 2 (15.4) |
| Type 2 diabetes mellitus | 7 (4.4) | 7 (4.8) | 0 |
| Obese | 9 (5.7) | 8 (5.5) | 1 (7.7) |
| Overweight | 39 (24.5) | 37 (25.3) | 2 (15.4) |
| Alcohol use | 33 (20.8) | 33 (22.6) | 0 |
| STEMI | 130 (81.8) | 122 (83.6) | 8 (61.5) |
| NSTEMI/UA | 11 (6.9) | 10 (6.8) | 1 (7.7) |
| Chronic stable angina | 18 (11.3) | 14 (9.6)* | 4 (30.8) |
| LV dysfunction | 46 (28.9) | 43 (29.5) | 3 (23.1) |
| Ejection fraction (%) | 56.8±13.33 | 56.9±13.2 | 55.8±14.8 |
| Heart failure | 17 (10.7) | 15 (10.3) | 2 (15.4) |
| Single-vessel disease | 112 (70.4) | 108 (74.0)** | 4 (30.8) |
| 2-vessel disease | 12 (7.5) | 11 (7.5) | 1 (7.7) |
| 3-vessel disease | 19 (11.9) | 14 (9.6)** | 5 (38.5) |
| Left main disease | 11 (6.9) | 7 (4.8)** | 4 (30.8) |
| PTCA (done/advised)† | 34/35 | 33/34 | 1/1 |
| CABG (done/advised)† | 10/19 | 7/13*** | 3/6 |
| Medical therapy | 104 (65.4) | 98 (67.1) | 6 (46.2) |
| Aspirin | 151 (95.0) | 139 (95.2) | 12 (92.3) |
| P2Y12 inhibitor | 94 (59.1) | 87 (59.6) | 7 (53.8) |
| Statin | 127 (79.9) | 118 (80.8) | 9 (69.2) |
| Beta blocker | 138 (86.8) | 127 (87) | 11 (84.6) |
| ACEI/ARB | 87 (54.7) | 82 (56.2) | 5 (38.5) |
| Nitrate | 112 (70.4) | 103 (70.5) | 9 (69.2) |
| Calcium channel blocker | 20 (12.6) | 17 (11.6) | 3 (23.1) |
| Mineralocorticoid antagonist | 12 (7.5) | 11 (7.5) | 1 (7.7) |
| Digoxin | 9 (5.7) | 9 (6.2) | 0 |
| Oral anticoagulation | 13 (8.2) | 12 (8.2) | 1 (7.7) |
P*<0.05, **<0.01, ***<0.001 compared to women. δLipid levels were not available in 5 of 146 men; †Analysis done based on the number of patients advised the corresponding treatment modality. ACEI, angiotensin-converting enzyme inhibitor; ARB, angiotensin receptor blocker; CABG, coronary artery bypass graft; LV, left ventricle; STEMI, ST segment elevation myocardial infarction; NSTEMI, Non-STEMI; PTCA, percutaneous transluminal coronary angioplasty; UA, unstable angina
The baseline ejection fraction (EF) was 56.8±13.3 per cent. Forty six (28.9%) patients had left ventricular (LV) dysfunction at presentation. ST-elevation myocardial infarction (STEMI) was the most common mode of presentation in young CAD patients below 30 yr of age. Of the 130 (81.8%) patients who presented with STEMI, 99 had anterior wall STEMI and 31 patients had inferior wall (and/or posterior wall) STEMI. Sixty four per cent patients (n=83) underwent thrombolysis at the hospital of first contact, making it the most common mode of revascularization. Only five patients with STEMI had undergone primary angioplasty. Twenty nine (22.3%) patients underwent elective percutaneous coronary angioplasty (PTCA). Thirty eight per cent patients presented outside the window period for thrombolysis or primary angioplasty. Twelve and two patients had Killip class II and class III presentation, respectively. One patient presented with cardiogenic shock. Left anterior descending artery was the culprit vessel in 78 per cent, whereas the right coronary artery was involved in 18.6 per cent patients. Thirty one (19.5%) patients had multivessel disease. Six patients had ectatic coronaries and one had spontaneous coronary artery dissection. While nine patients with STEMI were advised coronary artery bypass graft surgery (CABG), only seven of them underwent the same. Fourteen patients had normal coronaries.
The youngest patient to undergo CABG was a 15 yr old boy with familial hypercholesterolaemia who presented with effort angina and had two-vessel disease. Only 10 of the 19 patients advised CABG underwent the procedure. Two patients did not turn up for review and died of cardiac events, and two others were untraceable. There were no early deaths in those who underwent CABG, while there were two late deaths, at 7 and 20 yr after surgery. There was one inpatient death due to cardiogenic shock in a patient awaiting revascularization.
Latest follow up data were available in 92 per cent patients (n=147). Twelve patients remained untraceable. The mean duration of follow up was 9.1 yr (1402 patient-years). The last recruited patient had a follow up of seven months. Forty one patients died during follow up. While one patient developed major depressive disorder and committed suicide, all other deaths were out of hospital cardiac arrests. No autopsy data were available. Among those who were alive on follow up, 16 recurrent acute coronary events were documented in 14 patients, including two instances of STEMI. Eighteen (12%) patients developed heart failure on follow up, 16 of whom expired.
Four patients had major cerebrovascular accidents (CVAs) on follow up and one had a haemorrhagic CVA. Six ischaemic cerebrovascular events were recorded on follow up. Two patients developed severe peripheral occlusive vascular disease. One patient had an implantable cardioverter defibrillator (ICD) implanted for secondary prophylaxis.
Only seven patients (4.4%) did not have any of the major potentially modifiable risk factors at presentation, viz., smoking, systemic hypertension, diabetes mellitus, dyslipidaemia, alcohol use or obesity. Five of them presented with STEMI. Only one of them had a family history of premature CAD. One female patient with antiphospholipid antibody syndrome had significant left main coronary involvement with triple-vessel disease and underwent CABG, whereas the others had single-vessel disease. A subset analysis showed that those who had normal coronaries were less likely to be habituated to alcohol (P<0.05) compared to those with diseased coronaries. However, the other risk factors were similar.
Follow up data showed that 34 (33.7% of earlier smokers) patients continued to smoke even after their index event. While eight of them expired, the others remained current smokers and many were lost from routine outpatient follow up and traced up during the study. Twenty six (16.8%) patients were alcohol users on follow up. Twenty men continued their drinking habits and only seven prior alcoholic patients managed to abstain from drinking. On follow up, it was observed that five patients who were not alcoholics before their index events had taken up alcoholism, one of whom turned a binge drinker. Eighty (50.3%) patients were physically inactive on follow up. Only three overweight patients achieved a 10 per cent weight reduction on follow up. Poor dietary regulation was a major uncontrolled risk factor noted on follow up. One hundred and thirty four (78.6%) patients for whom the dietary data could be obtained had inadequate intake of fruits and vegetables.
Non-adherence to medications was seen in 41 per cent patients (n=134) with available follow up data regarding the same. Ten of these non-compliant patients died on follow up. Seven of them had documented recurrent acute coronary events. Forty two patients who had irregular outpatient reviews were found to be not taking any medications for several years. The most common cited reason for non-adherence was the absence of symptoms. However, statistical analysis did not identify a higher MACCE rate in patients documented to be non-adherent to medications, probably because medication compliance status could not be ascertained in a significant number of patients who had died.
Survival analysis showed survival rates of 84, 70, 58 and 52 per cent at 5, 10, 15 and 20 yr, respectively. The one and three-year mortality rates were 3.2 and seven per cent, respectively. Overall MACCE rate in our patients was 39 per cent at 10-yr follow up. Long-term survival was comparable in young men and women with CAD. However, patients with LV dysfunction at presentation had significantly poorer long-term survival (binary logistic regression P=0.002) and the curves diverged more from five years after presentation (log-rank Chi-square: 9.120, P=0.003). The long-term mortality rates were proportionate to the degree of LV dysfunction as shown in Figure 2A, B (log-rank Chi-square: 45.520, P<0.001). Patients who were advised CABG had poorer long-term outcomes compared to those who had underwent PTCA or were kept on medical management (log-rank Chi-square: 9.033, P=0.011) (Fig. 2C). Patients who underwent PTCA showed a non-significant trend toward better survival than those who were kept on medical management (log-rank Chi-square: 1.227, P=0.268). There was no significant difference in long-term mortality in patients who presented with STEMI as compared to NSTEMI. There was no significant difference in survival of patients with LDL ≥190 mg/dl and those with lower values (log-rank Chi-square: 0.042, P=0.837).
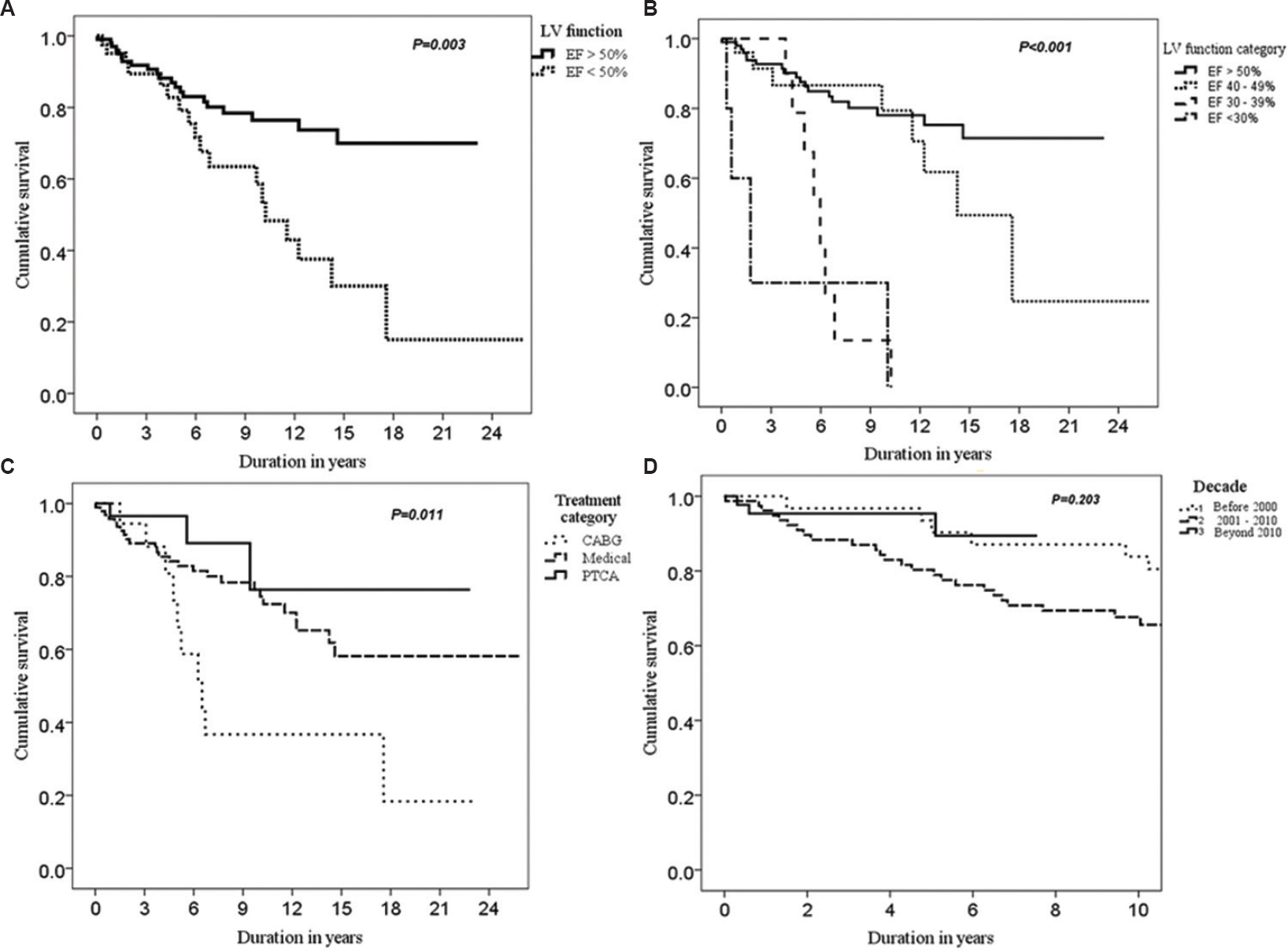
- Long-term Kaplan-Meier survival curves of young coronary artery disease patients. Survival curves of patients with preserved left ventricular function (A) and those with left ventricular dysfunction (B) in varying degrees. (C) Survival based on the modes of therapy. (D) Survival curves of patients who presented before 2000, between 2000 and 2010 and those who presented beyond 2010.
Considering the long study period, with significant variations in the guideline-directed management, patient outcomes over varying decades of presentation were analysed. Kaplan–Meier analysis showed insignificant difference in the long-term survival on a decade-based analysis (P=0.203) (Fig. 2D). However, those who presented between 2000 and 2010 tended to have lower mid-term survival as compared to those who presented later (P=0.086). Subset analysis showed no significant difference in the decade-based survival among females. However, the survival curves of males were significantly improved in the current decade as compared to those who presented between 2000 and 2010 (log-rank P=0.026). Cox regression suggested no age-related trends in survival over the various decades. The use of dual antiplatelets and statins expectedly increased over time. 89.1 per cent (n=40) of those who presented in the current decade were on dual antiplatelets and 95.7 per cent (n=44) were on statins.
A Cox proportional hazard model was developed to evaluate the individual hazards associated with long-term mortality. All clinical characteristics were included in the univariate analysis as covariates for long-term mortality. The univariate model showed the presence of LV dysfunction and multivessel involvement as predictors of long-term mortality (Table II). This model was more robust in the male subset. A 10 per cent decrease in LVEF had a hazard ratio (HR) of 1.433 [95% confidence interval (CI): 1.174-1.749] for mortality. Alcohol intake showed a trend toward long-term mortality benefit on univariate analysis, but was deemed otherwise upon multivariate analysis (HR: 0.596, 95% CI: 0.230-1.543). On multivariate analysis, the predictors of long-term mortality were multivessel involvement and reduced EF (Table II). Overweight and/or obesity was protective for long-term mortality. A similar analysis in this subset of patients with STEMI (univariate followed by multivariate), showed that LV dysfunction (P<0.05) remained predictive of long-term mortality while the obesity paradox persisted (P<0.05).
| Parameter# | HR | 95% CI | P |
|---|---|---|---|
| Univariate analysis | |||
| Age | 0.968 | 0.876-1.069 | 0.520 |
| Female sex (as compared to males) | 1.128 | 0.346-3.680 | 0.841 |
| Smoking | 1.068 | 0.540-2.112 | 0.851 |
| Systemic hypertension | 0.709 | 0.170-2.954 | 0.637 |
| Type 2 diabetes mellitus | 0.048 | 0.000-2041.820 | 0.576 |
| Dyslipidaemia | 0.597 | 0.206-1.732 | 0.343 |
| Alcohol | 0.452 | 0.176-1.155 | 0.097 |
| Overweight or obese | 0.235 | 0.0720.765 | 0.016 |
| Physical inactivity | 1.629 | 0.637-4.167 | 0.308 |
| LV dysfunction | 2.403 | 1.283-4.501 | 0.006 |
| Ejection fraction (10% decrease) | 1.433 | 1.174-1.749 | <0.001 |
| Presentation as STEMI | 0.863 | 0.381-1.956 | 0.724 |
| Multivessel involvement | 2.086 | 1.084-4.016 | 0.028 |
| Multivariate analysis | |||
| Ejection fraction (10% decrease) | 1.349 | 1.096-1.662 | 0.005 |
| Multivessel involvement | 1.927 | 1.003-3.701 | 0.049 |
| Overweight or obese | 0.298 | 0.090-0.983 | 0.047 |
| Alcohol | 0.596 | 0.230-1.543 | 0.286 |
#Each listed parameter was tested against the absence of the same for analysis. CI, confidence interval; HR, hazard ratio
A similar analysis was done for the composite outcome of long-term mortality and recurrent cardiac events (Table III). Multivessel involvement was the sole strong predictor of the composite outcome (HR: 2.083, 95% CI: 1.174-3.697). Obesity paradox was not seen with regard to the composite outcome, unlike the long-term mortality outcome.
| Parameter# | HR | 95% CI | P |
|---|---|---|---|
| Age | 1.031 | 0.935-1.137 | 0.535 |
| Female sex (as compared to males) | 0.519 | 0.126-2.142 | 0.365 |
| Smoking | 0.813 | 0.456-1.450 | 0.484 |
| Hypertension | 1.190 | 0.426-3.322 | 0.740 |
| Type 2 diabetes mellitus | 2.831 | 0.672-11.921 | 0.156 |
| Dyslipidaemia | 1.129 | 0.485-2.627 | 0.779 |
| Alcohol | 1.202 | 0.648-2.229 | 0.560 |
| Overweight or obese | 0.678 | 0.339-1.355 | 0.271 |
| Physical inactivity | 1.088 | 0.578-2.047 | 0.795 |
| LV dysfunction | 1.713 | 0.962-3.050 | 0.067 |
| Ejection fraction (10% decrease) | 1.210 | 0.985-1.486 | 0.070 |
| Presentation as STEMI | 0.606 | 0.323-1.138 | 0.119 |
| Multivessel involvement | 2.083 | 1.174-3.697 | 0.012 |
#Each listed parameter was tested against the absence of the same for analysis
Discussion
The mean age of patients in our study was considerably lower than other similar published series on young CAD36. Our study showed that the potentially modifiable major cardiovascular risk factors were associated with the vast majority (95%) of patients with symptomatic CAD even in the very young, similar to data from older adults from South Asia10. Dyslipidaemia and smoking were the most prevalent risk factors in our study similar to data from other studies on slightly older patients111213. While these patients constituted a heterogeneous group, the overwhelming presence of modifiable risk factors was disconcerting and suggested the need for heightened efforts for preventive strategies in the community at large in the school going age itself. The proposed seven-pronged strategy for improving STEMI care in the Indian scenario14 should target the population in the initial decades of life.
A low number of patients with STEMI who received primary PTCA suggested the delay in the diagnosis of obstructive CAD in these youths. More than a third of patients had evolved myocardial infarction. Although an accurate analysis of the factors related to delayed presentation of these patients was not possible due to the retrospective study design, data obtained by interviews on follow up visits suggested that delay in seeking hospital attention was the primary cause for delayed presentation in the majority.
While all patients who were offered PTCA underwent the same, the option of CABG was not well taken by some patients in the study. This was reflected in the significant early attrition rate in the CABG arm. However, patients who underwent CABG had reasonable early survival as shown earlier15. Long-term survival was significantly worse in the CABG arm compared to those who had milder CAD and were managed medically or with PTCA. This could be because of more extensive CAD in patients who were advised CABG as compared to those who underwent PTCA. There was no significant difference in the adherence to medications in either subset. However, more patients who underwent CABG had family history of premature CAD (P=0.040) as compared to those who underwent PTCA.
The non-significant trend toward better long-term survival in patients who underwent PTCA compared to those who were kept on medical management was probably reflective of the better adherence to medications in the PTCA subgroup. While nearly half of the medically managed patients had discontinued all medications, non-adherence was less than one-third in those who had undergone PTCA.
A 10-yr mortality of 30 and 48 per cent over 20 yr in patients with symptomatic CAD younger than 30 yr is a cause for concern. These numbers fare unfavourably compared to 10-yr survival rates of 82 and 88 per cent in patients between 47 and 53 yr with medical management and CABG, respectively, from the CASS (Coronary Artery Surgery Study) registry16. Cole et al17 reported a mortality of 30 per cent at 15 yr in patients younger than 40 yr of age with myocardial infarction. Nauta et al18 reported a mortality of 29 per cent at 16 yr in patients below 55 yr of age with myocardial infarction.
The increased long-term mortality with LV dysfunction in our patients was on expected lines, and so was its proportionate relationship to the degree of LV dysfunction1920. None of the patients in the study had undergone implantable cardioverter defibrillator implantation for primary prevention considering financial reasons.
Overweight and/or obesity was associated with better long-term survival, but did not protect against the composite outcome of long-term mortality and recurrent cardiac events. This association has been described in various studies, but the exact mechanism remains speculative2122. Neither did these patients present earlier relative to others, nor did they have worse LV function, thus contradicting some of the postulated explanations for obesity paradox. Medication adherence was marginally better in the overweight patients. The postulated explanation could be that obese patients with their higher total body water content, possibly lower plasma renin activity and higher levels of blood pressure could tolerate more proven medications at higher doses than lean patients.
One of the major findings of our study was the suboptimal risk factor control on follow up in these patients. While adherence to individual medications could not be assessed due to the large number of patients who had earlier been lost to follow up, total non-compliance in 28 per cent of patients was a cause for concern. This was higher compared to those reported in the CRUSADE and ACTION registries23. The implications of non-adherence in the young population could be catastrophic24. The use of customized algorithms for resource-limited settings and universal insurance cover may be required to reduce the burden of CAD in the community2526.
While multivessel disease and LV dysfunction were associated with poor outcomes, the overall poor outcomes could also be related to poor awareness of CAD in this age group. This is indicated by the delayed presentation in a large proportion of patients with acute MI and low rates of primary angioplasty. High rates of non-adherence in these patients who had MI suggested that this was a vulnerable group with poor awareness of the long-term implications of developing CAD at a very young age. This aspect could not be studied more extensively in this study, as we did not compare them with older patients.
One of the limitations of our study was that it was a single-centre study conducted at a tertiary care hospital, with issues of referral bias. Although this could result in lower external validity, more than half of the patients with STEMI had undergone thrombolysis elsewhere and were subsequently referred to our centre. This factor, along with the standard definitions used in our study, should not significantly limit generalizability. Because this was an observational study over a long time period, the accuracy of documentation of risk factors, treatment and outcomes would remain questionable. The varying length of patients follow up was unavoidable, with the inherent risks of recall and reporting bias. The follow up data on risk factor control obtained in patients based on telephonic interviews could have accuracy limitations in the absence of recent hospital review. We could not obtain recent lipid profiles and LV function indices on echocardiography on all patients. Baseline lipid profiles in our study might not be representative of the community as some of the earlier patients had already been initiated on statin before lipid level analysis.
In conclusion, the potentially reversible risk factors accounted for the vast majority of CAD in young patients below 30 yr of age. Dyslipidaemia and smoking were the most prevalent risk factors in this study. The long-term mortality rates were high in these patients. Decreasing EF and multivessel involvement were the strong correlates for long-term mortality in these patients. Obesity paradox was seen with long-term survival benefit. Risk factor control and adherence to medications were inadequate in a substantial proportion of these patients even after major coronary events. Follow up data suggest the vast scope for improvement of outcomes in these patients with more aggressive risk factor control and community level interventions targeting risk reduction.
Acknowledgment
Authors acknowledge Servshri C.P. Vineeth and V. Suresh Babu who were part of the data collection team, and thank Dr Sankara Sarma for helping in statistical analysis.
Financial support & sponsorship: None.
Conflicts of Interest: None.
References
- Cardiovascular diseases (CVDs). Available from: https://wwwwhoint/news-room/fact-sheets/detail/cardiovascular-diseases-(cvds)
- Effect of potentially modifiable risk factors associated with myocardial infarction in 52 countries (the INTERHEART study): Case-control study. Lancet. 2004;364:937-52.
- [Google Scholar]
- Premature coronary artery disease in India: Coronary artery disease in the young (CADY) registry. Indian Heart J. 2017;69:211-6.
- [Google Scholar]
- Coronary heart disease and risk factors in India - on the brink of an epidemic? Indian Heart J. 2012;64:364-7.
- [Google Scholar]
- Presentation, management, and outcomes of 25748 acute coronary syndrome admissions in Kerala, India: Results from the Kerala ACS Registry. Eur Heart J. 2013;34:121-9.
- [Google Scholar]
- Coronary heart disease mortality among young adults in the U.S. from 1980 through 2002: Concealed leveling of mortality rates. J Am Coll Cardiol. 2007;50:2128-32.
- [Google Scholar]
- Coronary heart disease mortality among young adults in Scotland in relation to social inequalities: Time trend study. BMJ. 2009;339:B2613.
- [Google Scholar]
- Geographic and sociodemographic variation of cardiovascular disease risk in India: A cross-sectional study of 797,540 adults. PLoS Med. 2018;15:E1002581.
- [Google Scholar]
- Scientific Steering Committee on behalf of the Simon Broome Register Group. BMJ. 1991;303:893-6.
- [Google Scholar]
- Overview of coronary heart disease risk initiatives in South Asia. Curr Atheroscler Rep. 2017;19:25.
- [Google Scholar]
- Coronary artery disease in patients aged 35 or less - a different beast? Heart Views. 2011;12:7-11.
- [Google Scholar]
- Myocardial infarction in young adults: Angiographic characterization, risk factors and prognosis (Coronary Artery Surgery Study Registry) J Am Coll Cardiol. 1995;26:654-61.
- [Google Scholar]
- Clinical factors and angiographic features associated with premature coronary artery disease. Chest. 1995;108:364-9.
- [Google Scholar]
- Confronting system barriers for ST-elevation MI in low and middle income countries with a focus on India. Indian Heart J. 2018;70:185-90.
- [Google Scholar]
- Coronary bypass surgery in young adults. A long-term survey. Interact Cardiovasc Thorac Surg. 2008;7:126-9.
- [Google Scholar]
- Ten-year follow-up of survival and myocardial infarction in the randomized Coronary Artery Surgery Study. Circulation. 1990;82:1629-46.
- [Google Scholar]
- Long-term follow-up of coronary artery disease presenting in young adults. J Am Coll Cardiol. 2003;41:521-8.
- [Google Scholar]
- Age-dependent care and long-term (20 year) mortality of 14,434 myocardial infarction patients: Changes from 1985 to 2008. Int J Cardiol. 2013;167:693-7.
- [Google Scholar]
- Risk stratification and survival after myocardial infarction. N Engl J Med. 1983;309:331-6.
- [Google Scholar]
- The relationships of left ventricular ejection fraction, end-systolic volume index and infarct size to six-month mortality after hospital discharge following myocardial infarction treated by thrombolysis. J Am Coll Cardiol. 2002;39:30-6.
- [Google Scholar]
- Body mass index and mortality in acute myocardial infarction patients. Am J Med. 2012;125:796-803.
- [Google Scholar]
- The impact of obesity on the short-term and long-term outcomes after percutaneous coronary intervention: The obesity paradox? J Am Coll Cardiol. 2002;39:578-84.
- [Google Scholar]
- Predictors of early discontinuation of evidence-based medicine after acute coronary syndrome. Am J Cardiol. 2009;104:175-81.
- [Google Scholar]
- Management algorithms for acute ST elevation myocardial infarction in less industrialized world. Indian Heart J. 2017;69(Suppl 1):S98-103.
- [Google Scholar]
- Reducing system delays in treatment of ST elevation myocardial infarction and confronting the challenges of late presentation in low and middle-income countries. Indian Heart J. 2017;69(Suppl 1):S1-5.
- [Google Scholar]






