Translate this page into:
Changes in olfaction & quality of life following standard medical therapy in patients with intermittent & persistent allergic rhinitis
For correspondence: Dr V. Rupa, Department of ENT & Clinical Epidemiology Unit 3, Christian Medical College, Vellore 632 004, Tamil Nadu, India e-mail: rupavedantam@cmcvellore.ac.in
-
Received: ,
This article was originally published by Wolters Kluwer - Medknow and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Background & objectives:
Allergic rhinitis (AR) is an inflammatory disease prevalent worldwide which can affect both olfaction and quality of life (QoL). The objective of the present study was to assess olfaction and QoL changes in patients with AR before and after medical therapy.
Methods:
Adult participants (>18 yr) with AR were recruited for this study. These patients prospectively underwent olfaction testing using the modified Connecticut Chemosensory Clinical Research Centre Test and QoL assessment using Rhinoconjunctivitis QoL Questionnaire (RQLQ) before and after standard medical therapy with topical steroids and/antihistaminics.
Results:
Of the 150 patients recruited, 72 per cent had intermittent AR. The symptom of hyposmia was present in 34 patients (22.7%) and was more prevalent in patients with moderate-to-severe type of AR (P<0.001). However, olfaction testing revealed hyposmia/anosmia in 44 patients (29.3%). Mean composite olfaction scores were significantly higher in patients with mild AR compared to moderate/severe AR (P=0.026). The pre-therapy mean composite olfaction score in the 34 patients with olfaction disturbances was 3.1 standard deviation (±1.06 SD). Following therapy, the mean composite olfaction score rose to 4.3 (±1.34 SD) and this change was found to be significant (P<0.001). Mean pre-therapy RQLQ scores were 2.87 (0.06-5.33) overall. Significant improvement was also found in RQLQ scores following therapy (P<0.001). Mean RQLQ scores were significantly lower in those with moderate-to-severe AR (P<0.001) as well as those with intermittent AR (P=0.004). Nine patients had persistently high RQLQ scores after medical therapy.
Interpretation & conclusions:
Both olfaction and QoL showed significant improvement after medical therapy in Indian adults with AR. In those patients who do not improve, other causes must be sought for the persistent symptoms.
Keywords
Allergic rhinitis
hyposmia
quality of life
Allergic rhinitis (AR) is prevalent worldwide and affects an estimated 400 million of the world’s population12. Data from Western studies suggest that this disease is more common in urban areas3. However, data regarding the prevalence of AR in the Indian population are limited. One community-based study reported the prevalence in adults as being 11 per cent4. A study from China reported that the prevalence of AR is 14.9 per cent with more people in urban areas (19.5%) being affected than those in rural areas (10.8%)5.
Allergic rhinitis is known to affect olfaction in many individuals678910111213. The overall prevalence of olfactory dysfunction due to AR has been reported to be 21.5 to 23 per cent68. Studies on children have shown a high prevalence of hyposmia in AR11. Olfactory dysfunction has been shown to be worse in patients with seasonal AR during the season than in patients with perennial rhinitis612. In more recent studies where the newer AR Impact on Asthma (ARIA) classification has been used, patients with moderate/severe persistent AR were found to have a higher prevalence of hyposmia1314.
Another important effect of AR is its impact on the quality of life (QoL) in an individual151617. Several QoL instruments have been used in Western studies to highlight changes in QoL in various domains in AR7,15-19. The aspects of QoL that can get affected include sleep, alertness, feeling of wellness, cognitive and emotional functioning and psychomotor performance. Any affectation of these features has been shown to be strongly associated with the severity of symptoms in AR15. The Rhinoconjunctivitis QoL Questionnaire (RQLQ), first introduced by Juniper et al18 is one of the most widely used rhinitis-specific questionnaires for the evaluation of QoL in AR. It covers nasal and non-nasal symptoms, sleep, limitation of specific activities and emotional function. Studies have shown that RQLQ scores are significantly affected in those patients with AR who experience a total of at least 31 days of allergic symptoms19.
Although AR is common in the Indian subcontinent, there are only a few studies that have provided any data on the prevalence and effect on smell and QoL of AR in these patients420. However, none of these studies provide any data on the use of the skin allergy test to make a definitive diagnosis of AR or a standardized olfaction test to assess the effect of AR on olfaction. Furthermore, there is no information in literature on the effectiveness of first-line allergy therapy on olfaction or QoL in Indian patients using these tools.
Even in world literature, although a new classification system was introduced in 2001 for effective diagnosis and management of AR patients21, only a few studies have so far applied this classification, making comparisons between studies difficult. The present study was, therefore, designed to study the effect on olfaction and QoL in an adult Indian population with AR using the new ARIA classification. The effect of first-line therapy on the patient’s olfaction and QoL scores was also sought.
Material & Methods
Participants: A total of 550 patients aged >18 yr who presented with symptoms of AR such as sneezing, nasal obstruction, nasal discharge, epiphora and itching to the outpatient clinic of the department of Otorhinolaryngology, Christian Medical College Hospital, Vellore, India, between November 2014 and March 2016 were initially screened for recruitment to the study. Only 150 patients who had a positive skin allergen test and were diagnosed with AR and who gave informed consent were included in the study. Patients who had a negative skin allergen test result, who used oral or inhaled steroids for at least two weeks prior and patients with any other nasal disease including polyposis and malignancy were excluded from the study. Also patients who refused to participate in the study were excluded from the study. Note was made of any co-morbidities and history of smoking. The study design was approved by the Institutional Review Board and Ethics Committee of the hospital (IRB number: 9094).
Pre-treatment assessment: All patients underwent detailed otorhinolaryngological evaluation and were diagnosed with intermittent or persistent AR along with mild or moderate/severe disease as per ARIA guidelines21. QoL assessment was performed using the RQLQ which is a validated instrument and has been widely used across the world. The questionnaire was validated in Tamil, Hindi and Bengali, the three languages which were understood by the study population. The RQLQ has 28 questions covered under seven domains (activity limitation, sleep problems, nose symptoms, eye symptoms, non-nose/eye symptoms, practical problems and emotional function). There are three patient-specific questions in the activity domain which allow patients to select any three activities in which they feel inhibited due to AR. Each question is self-evaluated by the patient on a 7-point scale (0-6). The mean of all 28 questions is the RQLQ score. Individual domain scores are also calculated.
Rigid nasal endoscopy, skin allergy testing and IgE level estimation was performed in all patients before starting therapy. Olfaction testing was performed using the modified Connecticut Chemosensory Clinical Research Centre (CCCRC) test22 which consists of two parts, the butanol threshold test and the smell identification test. The basis of the butanol threshold test is the ability of the patient to distinguish between the odour of butanol at different concentrations. The smell identification test was designed using a fixed number of commonly perceived odours like rose, jasmine, coffee, talcum powder etc. and using a forced choice method for the patient to identify the odour. A detailed description of the test is provided by Cain et al22. A sum of the two test results provided the composite olfaction score. Normal values for the composite olfaction score obtained by testing 40 age- and sex-matched controls were found to range from 4.25 to 7.
The scores were then analyzed as follows: (i) normosmia: 4.25-7; (ii) hyposmia: 2 to 4; and (iii) anosmia <2.
Treatment given: All recruited patients received 12 wk of medical therapy which included steroid nasal sprays and normal saline drops. Fifteen patients received a short course of antihistamines and leukotriene antagonists also in the first two weeks of commencing therapy.
Post-treatment assessment: Following a three-month course of therapy, patients were administered the RQLQ questionnaire again. So, those patients who were found to have olfactory dysfunction at the first instance underwent reassessment. A comparison of pre- and post-treatment parameters was made to see if there was the improvement in QoL as well as reversal of hyposmia following therapy. Written informed consent was obtained from all subjects before starting the study.
Statistical methods:
Sample size calculation: Based on the prevalence of 23 per cent for hyposmia in patients with AR as per the study by Cowart et al8, we used the formula, sample size = n = {4 p (1 – p)} / d2, where ‘p’ is the prevalence and ‘d’ is the precision. With a precision of seven with 95 per cent confidence interval, the sample size was determined to be 135 subjects. Assuming that there would be about 10 per cent dropouts, it was decided to study 150 subjects in all.
Adequacy of sample size for looking at change in mean olfaction score following therapy: A power analysis was performed to assess the adequacy of sample size23. Our hypothesis was that the post-therapy composite olfaction score would be significantly different from the pre-therapy score. Based on our data, the pre-therapy composite olfaction score was about 3 standard deviation (S.D.=1). Expecting a one unit increase in post-therapy mean composite olfaction score with a similar SD, alpha error of one per cent and power of 99 per cent, a minimum of 30 subjects needed to be studied. The sample size studied was thus deemed to be adequate to show this difference.
Statistical analysis: The data were analyzed using SPSS 16.0 software (SPSS Inc., Chicago, IL, USA). Frequencies and percentages of categorical variables were calculated. Means with SD of continuous variables were calculated. Association between categorical variables was assessed using the Chi-square test with Yate’s correction. Pre- and post-therapy means were compared by paired t test. Independent two-sample t test was done to compare means of RQLQ scores and composite olfaction scores for patients with intermittent and persistent rhinitis as well as between mild and moderate/severe rhinitis. A P<0.05 was considered statistically significant.
Results
Demography: A total of 150 patients were included based on the diagnostic criteria set out in the study protocol. Eleven patients who were lost to follow up were excluded from the analysis. There were 84 males and 66 females with a mean age of 32.3±9.4 yr. Intermittent rhinitis (72%) was more common than persistent rhinitis (28%). Mild rhinitis occurred in 48 per cent of patients and moderate/severe in 52 per cent.
Symptoms: The most common symptom reported among the study participants was watery nasal discharge (91.3%), followed by sneezing (92.7%). Ocular symptoms were also experienced (68%), although to a lesser extent. Thirty four (22.7%) patients alone complained of reduced sensation of smell. When symptoms were compared between patients with mild AR and those with moderate/severe AR, it was found that while nasal obstruction, watery nasal discharge and sneezing were equally prevalent in both categories, nasal itching, watering of eyes and reduced sensation of smell were significantly more in those with moderate/severe AR (Table I).
Olfaction analysis:
Baseline olfaction assessment: In this cohort, 44 patients (29.3%) were found to have hyposmia/anosmia on testing. The composite olfaction score was found to range from 4.25 to 6.75 in those with normosmia and 1 to 4 in those with reduced/absent olfaction. The mean composite olfaction score was 3.1 (SD=1.06) in the cohort.
Reduced sensation of smell (79.4%) was more prevalent in patients with moderate-to-severe type of AR (P<0.001) (Table I). The mean composite olfaction score in 72 patients with mild AR was 4.9±1.29 and in 78 patients with moderate/severe AR, it was 4.4±1.42. The difference in mean composite olfaction scores between the two groups was significant (P=0.026). The mean composite olfaction score in 108 patients with intermittent AR was 4.7±1.42 and that in 42 patients with persistent rhinitis was 4.8±1.31 and the difference was not found to be significant (P=0.81).
| Symptoms | Diagnosis | |
|---|---|---|
| Mild AR (n=72), n (%) | Moderate/severe AR (n=78), n (%) | |
| Watery nasal discharge | ||
| Yes | 64 (46.7) | 73 (53.3) |
| No | 8 (61.5) | 5 (38.5) |
| Sneezing | ||
| Yes | 66 (47.5) | 73 (52.5) |
| No | 6 (54.5) | 5 (45.5) |
| Nasal obstruction | ||
| Yes | 60 (47.6) | 66 (52.4) |
| No | 12 (50.0) | 12 (50.0) |
| Nasal itching | ||
| Yes | 42 (41.6) | 59 (58.4) |
| No | 30 (61.2) | 19 (38.8) |
| Watering of eyes* | ||
| Yes | 43 (42.2) | 59 (57.8) |
| No | 29 (60.4) | 19 (39.6) |
| Reduced sensation of smell*** | ||
| Yes | 7 (20.6) | 27 (79.4) |
| No | 65 (56) | 51 (44) |
P *<0.05, ***<0.001. AR, allergic rhinitis
There were 24 (16%) smokers in the cohort, nine (7.04%) of whom had hyposmia/anosmia. No association was found between smoking and hyposmia/anosmia (P=0.48).
Post-therapy olfaction assessment: A total of 34 patients who exhibited disturbances in olfaction upon testing before commencement of therapy were found to have normal olfaction or mild hyposmia post-therapy (Figure). The pre-therapy mean composite olfaction score was 3.1±1.06 and the post-therapy mean composite olfaction score was 4.3±1.34) (Table II). When the composite olfaction scores were compared pre- and post-therapy in the 34 patients (follow up was available in these patients), it was found that there was a significant improvement in mean scores (P<0.001).
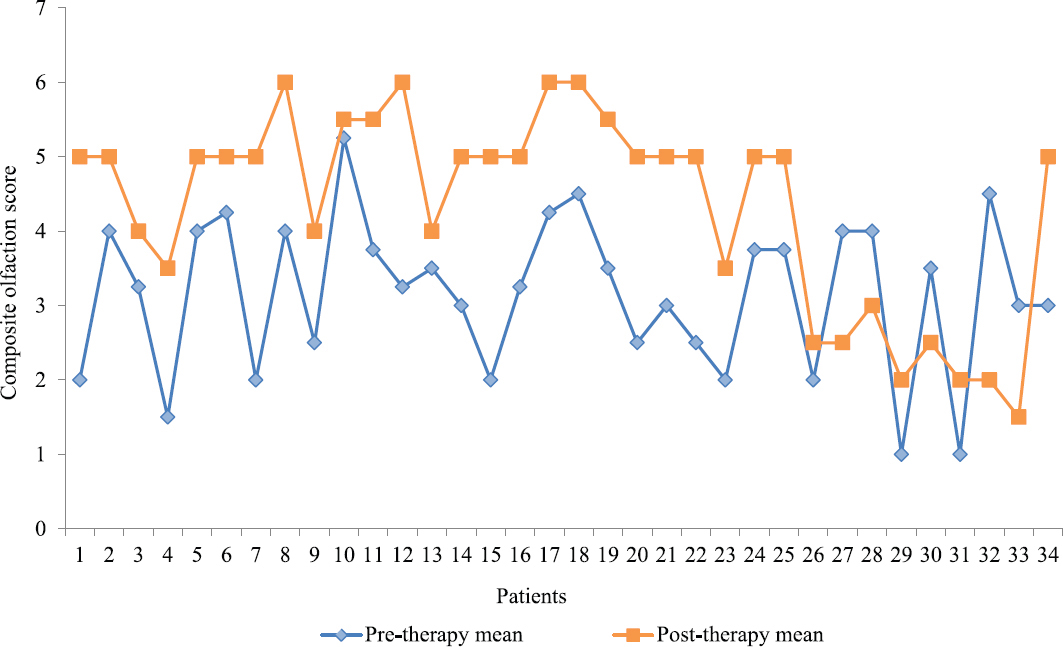
- Pre- and post-therapy composite olfaction scores in patients who reported for follow up assessment (n=34).
| Results of olfaction tests | Pre-therapy olfaction status (n=150) | Pre-therapy olfaction status in those with smell disturbances (n=34) | Post-therapy olfaction status (n=34) |
|---|---|---|---|
| Normosmia, n (%) | 106 (70.7) | 5 (14.7) | 21 (61.8) |
| Hyposmia/anosmia, n (%) | 44 (29.3) | 29 (85.3) | 13 (38.2) |
| Mean olfaction score±SD | 4.72±1.06 | 3.1±1.06 | 4.3±1.34 |
SD, standard deviation
Skin allergy test results: Dust mite (Dermatophagoides pteronnysinus and D. farinae) was by far the most common type of allergen (78%) with 64 per cent of patients testing positive to both the species followed by house dust (60%) and cockroach (28%). Ingested allergens were less frequently reported, but patients who did report, the most common allergen was brinjal (12%).
Quality of life (QoL) analysis:
Baseline data: Pre-therapy RQLQ scores were 2.87 (0.06-5.33) overall, and were particularly elevated for nasal, non-nasal and emotional symptoms. When RQLQ scores between mild and moderate/severe rhinitis were compared, it was found that patients with the latter had significantly higher scores than those with mild rhinitis (P<0.001). When RQLQ scores were compared between patients with intermittent (mean, 2.69±1.11) and persistent (mean, 3.30±0.19) rhinitis, it was found that patients with intermittent AR had worse QoL and this difference was significant (P=0.004).
Post-therapy rhinoconjunctivitis quality of life questionnaire (RQLQ) scores: Upon comparing the RQLQ scores pre- and post-therapy in patients with available follow up (n=139), a significant improvement was found in the mean scores for all domains (Table III), with the least change being in the emotional domain.
| QoL domains using RQLQ | Mean±SD | |
|---|---|---|
| Pre-therapy | Post-therapy | |
| Activities | 2.64±1.66 | 1.76±0.82*** |
| Sleep | 1.89±1.74 | 0.98±0.64*** |
| Non-nasal | 2.85±1.46 | 1.58±0.79*** |
| Practical | 2.78±1.83 | 1.67±0.82*** |
| Nasal | 3.66±1.31 | 1.48±0.50*** |
| Eye | 2.46±1.53 | 0.77±0.44*** |
| Emotional | 3.3±1.73 | 2.85±1.18* |
P *<0.05, ***<0.001. RQLQ, rhinoconjunctivitis QoL questionnaire; SD, standard deviation
Persistent reduction in RQLQ scores: Although there was an overall improvement in QoL, nine patients had reduced RQLQ scores post-therapy. An analysis of this subset suggested definite causes for the persistently low scores among these nine patients. In five patients, a posterior deviation of the nasal septum was present and hence these patients did not show complete reduction of symptoms of nasal obstruction following therapy. In four other patients with no apparent anatomical abnormalities, sleep, non-nasal and emotional domains scored higher and hence, the overall score was high. These patients subsequently received psychiatric evaluation for depression.
Discussion
Despite the introduction of the ARIA classification in 20011, the reporting of studies on patients with AR has not changed significantly. In the present study intermittent AR (72%) was found to be more common than persistent AR (28%). The results of this study were similar to the findings by Valero et al15 who also reported intermittent rhinitis (61.5%) as the most common type. Similarly, Becker et al10 reported seasonal rhinitis was more common than persistent rhinitis.
Hyposmia remains as the least investigated symptom among patients with AR. In this study, 29.3 per cent of patients who were diagnosed with AR had olfactory dysfunction on testing and 22.7 per cent complained of reduced sense of smell. Similar results have been found in a few other studies6,8,10,13. The association between AR severity and smell has been a matter of debate. Guilemany et al13 found that patients with moderate/severe persistent AR had a greater level of hyposmia. Similarly, in this study, hyposmia/anosmia was found to be significantly more prevalent in patients with moderate/severe type of AR rather than mild AR. In contrast, Kutlug et al24 found no association between odour scores and the severity of rhinitis.
The improvement of olfactory dysfunction after therapy in all patients who had hyposmia/anosmia before commencing therapy in our study was significant. However, variable results have been seen in other studies. Sivam et al25 performed a randomized, double-blinded, placebo-controlled study in which mometasone furoate was administered for two weeks and the olfactory function before and after therapy was measured. They reportedly found no significant difference in olfaction post-therapy. In another study where both intranasal and oral steroids were administered to AR patients, it was reported that patients on oral steroids showed better chances of resolution of hyposmia as compared to those on nasal steroid sprays26.
A number of western studies have looked at the impact of AR on QoL. For example, Valero et al15, using a validated questionnaire, studied the severity of AR and its impact on QoL and reported that the severity of AR was proportional to the worsening of QoL. Additionally, Katotomichaelkis et al27 who studied the impact of olfactory dysfunction on the QoL of patients with AR and chronic rhinosinusitis, found that improvement in post-therapy olfaction had a significant impact on QoL in both sets of patients.
The domains affected in QoL assessment in patients with AR also merit analysis. The analysis of Shah and Pawankar20 showed that AR caused a significant impairment in the practical emotional and activity limitation domains and patients were less troubled by lack of sleep, similar to the findings of the present study. Following therapy, there was improvement in all the symptoms in most (93.5%) patients in our study. Post-therapy improvement in nasal and non-nasal symptoms has been noted by other authors as well28.
Our analysis of the various allergens that affected patients with AR showed that dust mite (D. pteryonnisinus and D. farinae) were the predominant allergens in both types of AR. Tham et al29 who studied aeroallergen sensitivity among Asians, found that unlike in Western countries, dust mite and house dust rather than pollen are the most common allergens in this population. Interestingly, patients with dust mite allergy also showed accentuation of symptoms during change of season. In our study, even though dust mite (which was ubiquitous and present throughout the year) was the most common allergen identified, more patients had intermittent rhinitis which was largely related to change of season. This increased sensitivity to season change in patients with dust mite allergy was also noted by Coskun et al30 in a study from the eastern Black Sea region of Turkey.
Overall, the novelty of this study is the use of standardized ARIA criteria and skin allergen testing to establish the diagnosis of AR as well as the use of a validated olfaction test like the CCCRC and a validated QoL questionnaire like RQLQ to obtain pre- and post-therapy data on adult Indian patients with AR.
Financial support & sponsorship: This study was partially funded by the FLUID research fund of Christian Medical College, Vellore.
Conflicts of Interest: None.
References
- World Health Organization. Allergic rhinitis and its impact on asthma. J Allergy Clin Immunol. 2001;108(Suppl 5):S147-334.
- [Google Scholar]
- Worldwide time trends in the prevalence of symptoms of asthma, allergic rhinoconjunctivitis, and eczema in childhood:ISAAC phases one and three repeat multicountry cross-sectional surveys. Lancet. 2006;368:733-43.
- [Google Scholar]
- The Danish urban-rural gradient of allergic sensitization and disease in adults. Clin Exp Allergy. 2016;46:103-11.
- [Google Scholar]
- Allergic rhinitis:A neglected disease –A community based assessment among adults in Delhi. J Postgrad Med. 2015;61:169-75.
- [Google Scholar]
- Prevalence and associated risk factors of allergic rhinitis in preschool children in Beijing. Laryngoscope. 2013;123:28-35.
- [Google Scholar]
- Assessment of smell and taste in patients with allergic rhinitis. Acta Otolaryngol. 2000;120:323-6.
- [Google Scholar]
- Patient perceptions of allergic rhinitis and quality of life:Findings from a survey conducted in Europe and the United States. World Allergy Organ J. 2008;1:138-44.
- [Google Scholar]
- Olfactory dysfunction in seasonal and perennial allergic rhinitis. Acta Otolaryngol. 2012;132:763-8.
- [Google Scholar]
- Allergic rhinitis causes loss of smell in children:The OLFAPEDRIAL study. Pediatr Allergy Immunol. 2016;27:867-70.
- [Google Scholar]
- Comparison of olfactory function in patients with seasonal and perennial allergic rhinitis. Allergy. 1998;53:297-301.
- [Google Scholar]
- Persistent allergic rhinitis has a moderate impact on the sense of smell, depending on both nasal congestion and inflammation. Laryngoscope. 2009;119:233-8.
- [Google Scholar]
- Prevalence, risk factors and comorbidities of allergic rhinitis in South Korea:The Fifth Korea National Health and Nutrition Examination Survey. Am J Rhinol Allergy. 2014;28:e107-14.
- [Google Scholar]
- The impact of allergic rhinitis on symptoms, and quality of life using the new criterion of ARIA severity classification. Rhinology. 2012;50:33-6.
- [Google Scholar]
- Impact of allergic rhinitis in school going children. Asia Pac Allergy. 2012;2:93-100.
- [Google Scholar]
- Symptomatology patterns in children with allergic rhinitis. Med Sci Monit. 2017;23:4939-46.
- [Google Scholar]
- Validation of the standardized version of the Rhinoconjunctivitis Quality of Life Questionnaire. J Allergy Clin Immunol. 1999;104:364-9.
- [Google Scholar]
- Subjective and objective assessments in patients with seasonal allergic rhinitis:Effects of therapy with mometasone furoate nasal spray. J Allergy Clin Immunol. 1998;102:39-49.
- [Google Scholar]
- Allergic rhinitis and co-morbid asthma:Perspective from India –ARIA Asia-Pacific Workshop report. Asian Pac J Allergy Immunol. 2009;27:71-7.
- [Google Scholar]
- Characteristics of intermittent and persistent allergic rhinitis:DREAMS study group. Clin Exp Allergy. 2005;35:728-32.
- [Google Scholar]
- Evaluation of olfactory dysfunction in the Connecticut Chemosensory Clinical Research Center. Laryngoscope. 1988;98:83-8.
- [Google Scholar]
- Introduction to sample size determination and power analysis for clinical trials. Control Clin Trials. 1981;2:93-113.
- [Google Scholar]
- Evaluation of olfactory function in children with allergic rhinitis and nonallergic rhinitis. Int J Pediatr Otorhinolaryngol. 2016;86:172-6.
- [Google Scholar]
- Olfactory cleft inflammation is present in seasonal allergic rhinitis and is reduced with intranasal steroids. Am J Rhinol Allergy. 2010;24:286-90.
- [Google Scholar]
- Improvement of olfactory function for quality of life recovery. Laryngoscope. 2013;123:E10-6.
- [Google Scholar]
- Quality of life assessment in patients with moderate to severe allergic rhinitis treated with montelukast and/or intranasal steroids:A randomised, double-blind, placebo-controlled study. J Laryngol Otol. 2014;128:242-8.
- [Google Scholar]
- Aeroallergen sensitization and allergic disease phenotypes in Asia. Asian Pac J Allergy Immunol. 2016;34:181-9.
- [Google Scholar]
- High sensitization to house-dust mites in patients with allergic rhinitis in the eastern Black Sea region of Turkey:A retrospective study. Am J Rhinol Allergy. 2016;30:351-5.
- [Google Scholar]






