Translate this page into:
Certification & validation of biosafety level-2 & biosafety level-3 laboratories in Indian settings & common issues
Reprint requests: Dr Devendra T. Mourya, Indian Council for Medical Research-National Institute of Virology, Sus Road, Pashan, Pune 411 021, Maharashtra, India e-mail: directorniv@gmail.com
-
Received: ,
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
With increasing awareness regarding biorisk management worldwide, many biosafety laboratories are being setup in India. It is important for the facility users, project managers and the executing agencies to understand the process of validation and certification of such biosafety laboratories. There are some international guidelines available, but there are no national guidelines or reference standards available in India on certification and validation of biosafety laboratories. There is no accredited government/private agency available in India to undertake validation and certification of biosafety laboratories. Therefore, the reliance is mostly on indigenous experience, talent and expertise available, which is in short supply. This article elucidates the process of certification and validation of biosafety laboratories in a concise manner for the understanding of the concerned users and suggests the important parameters and criteria that should be considered and addressed during the laboratory certification and validation process.
Keywords
Biosafety
BSL-2
BSL-3
certification
safety
validation
Introduction
The increasing re-emerging infections of public health importance, particularly newly emerging highly infectious zoonotic infections cause pressure on the containment laboratories to work on the microbial agents for providing timely diagnosis and find solutions for the interventions. In most of these cases, the microbial agents are highly contagious or airborne. These highly infectious and pathogenic microbial agents carry the risk of their escape by air, water, liquid and solid waste that comes out of laboratory and also via personnel exiting the laboratory after completion of experiments. The certification and validation process becomes more important in India123 in view of existence of a large number of biosafety level-2 (BSL-2) laboratories which are involved in work on biorisk group-3 pathogens45.
There is a general misunderstanding and lack of awareness about the process of certification and validation of biosafety laboratories. Once the physical construction and installation of all the equipment, engineering systems, services and utilities are completed, it is important that the facility is properly certified and validated before handling high-risk pathogens. This process needs to be diligently carried out to ensure that the facility meets the biosafety and biosecurity requirements and is safe for the personnel working in the laboratory as well as for the surrounding environment678.
While most of the criteria explained here are applicable to BSL-3 facilities, based on the scientific programmes and design features of the respective BSL-2 laboratories, the users should selectively choose the parameters and criteria as applicable to the individual BSL-2 facilities as per risk assessment of the work being performed.
Lack of concurrence among different stakeholders regarding certification and validation processes
The major issues associated with certification and validation of a biosafety laboratory remain misunderstood by laboratory managers/principal investigators (PIs) and other stakeholders and very often even by the external experts who are invited as committee members to validate biosafety laboratories. In a majority of the documents on establishing laboratories, this process is either vaguely defined or inadequately defined.
There is a need for all the users to have the basic understanding of the following: (i) What are the objectives of the laboratory?; (ii) What is the mandate of the laboratory?; (iii) What are the scientific programmes of the laboratory?; (iv) What are the codal/regulatory/statutory and biosafety & biosecurity requirements?; and (v) What are the design and engineering features of the laboratory?
Based on the intended use, scientific work, laboratory working protocols, design features and engineering installation, it is important to understand and identify the areas where the likely breach in biosafety and biosecurity may occur and how these issues have been addressed and the associated risks are mitigated. The certification and validation process ensures that the basic minimum standards and requirements for the unique facility have been addressed and met.
This article provides information necessary to understand the meaning, concepts and critical issues related with the process of certification and validation of biosafety laboratories.
Generic definition
Certification
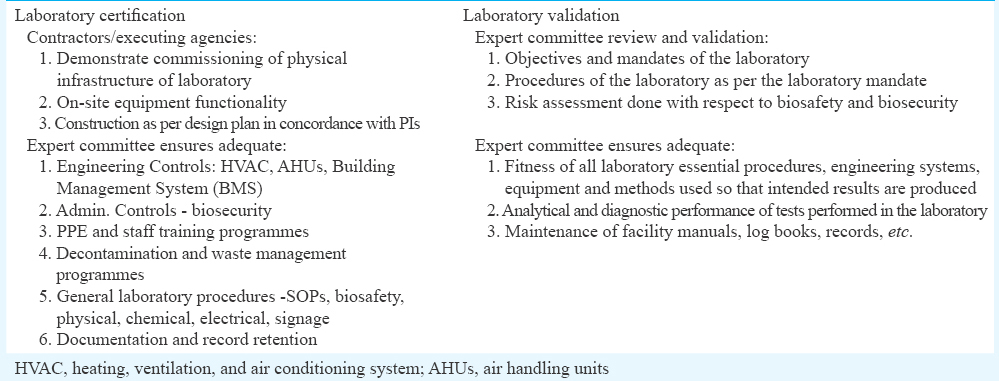
The certification process includes the processes by which it is verified that the physically built facility is as per the design and specifications provided by the PIs and meets the requirement. The certification process also includes the verification of on-site equipment and system performance that are present and have been installed in the physically built facility (Table I).
Laboratory certification is the systematic review of (i) all safety features and processes associated with the laboratory (engineering systems, controls, personal protective equipment (PPE), building and system integrity); (ii) standard operating procedures (SOPs); and (iii) administrative controls such as documentation and record retention system7. Standardization of an initial and annual certification plan for the BSL-3 facility provides accountability that ensures proper and regular maintenance and demonstrates the use of standard operating procedures (SOPs) that protect human and animal occupants, the environment and the research integrity9.
Validation
In general terms, the validation process is known as ‘the process of proving that a procedure, process, system, equipment or method used in the laboratory works as expected and achieves the intended result’10. In the context of a biosafety laboratory, the reagents, tests and equipment, the validation is a process that determines the fitness of these, which has been properly developed, optimized and standardized, for an intended purpose. Validation also includes estimates of the analytical and diagnostic performance characteristics of a test10. The validation process of a laboratory when being performed for the first time after taking over the facility from the construction company includes verification of laboratory installations and all the processes in total. The validation ensures that all appropriate facility controls and prudent practices are in place to minimize to the greatest extent possible, the risks associated with the laboratory operations and the use of biohazardous material (Table I).
In the absence of any standards/regulatory guidelines/accredited agency in the country for certification and validation of biosafety laboratories, it is recommended that the certification and validation process should be carried out by an expert team/committee, which should comprise members from scientific background, PIs of the laboratory and engineers having adequate experience and knowledge of functioning, operation, certification and validation of biosafety laboratories.
Anthology of certification and validation of containment laboratory and explanatory notes
Emphasis should be given to the following points for the certification of laboratories (BSL-2 and BSL-3 laboratories)1:
-
It should be ensured that proper engineering controls are used and function adequately as designed2.
-
Appropriate site and protocol-specific administrative controls should be in place3.
-
PPE and measures are appropriate for the tasks being performed4.
-
Decontamination of waste material has been adequately validated and proper waste management procedures are in place.
-
Proper procedures for general laboratory safety, including physical, electrical and chemical safety are in place11.
Basic laboratory safety issues and certification and validation checks
There should be proper signage indicating wherever the hazards such as ultraviolet (UV) light, laser and radioactive material, etc., exist12. The members of the committee should make sure that appropriate biosafety guidelines are available in the laboratory facility (need not be necessarily inside the laboratory) and followed by the staff. The laboratory equipment should be properly labelled13 such as biohazard, radioactive and toxic. It should also be checked that freezers, ultra-freezers and 37°C carbon dioxide incubators are identified and labelled for ‘clean and infectious material’. There should be defined secured place for storing radioactive material.
The members should also make sure that the laboratory design must conform to the mandate of the laboratory as proposed by the PIs/management. It should be designed for easy cleaning. Wherever the ultraviolet lights are installed in the pass boxes14 in the laboratory, there should be proper interlock switches and should be tested for interlocking of pass box doors and hour meter to ensure timely replacement of UV light.
Adequate storage space should be available in the laboratory as per the workflow and the mandate of the laboratory. All the shelves in the laboratory furniture and laboratory sidewalls should be properly secured. Benchtops should be waterproof and resistant to acids, alkali, organic solvents and heat. The illumination provided in the laboratory premises should be adequate, should be around 400 Lux15 and the same should be measured and checked.
If gas cylinders are used in the laboratory, then the cylinders should be properly secured in place and the reserve cylinders should be safely capped. Excess or empty cylinders should not be present in the laboratory premises and if present, must be secured in place. The inspection of gas cylinder and tubing should be conducted. The flow charts and laboratory process should define that processes involving asphyxiating and hazardous gases should be performed only in ventilated rooms, and in the case of BSL-3 laboratory, it should be performed in the rooms that have maximum negative pressure. Placement of chemicals in the laboratory should be checked and ensured that the flammables are stored in the specifically designed storage cabinet only and properly segregated. The hazardous chemicals should be stored above eye level and no chemical containers should be left open. All solutions and reagents present in the laboratory should be properly labelled16. Mercury thermometers should not be used.
Refrigerators and cold rooms should be checked and it should be ensured that no refrigerators/freezers/cold rooms are used to store food materials for human consumption. If cold rooms are present, these should have emergency release from inside so that, by mistake or due to any mechanical or electronic failure, the staff does not accidently get stuck inside these areas. There should be emergency plan available for such situations17. Certification of laboratory and operation of emergency release system of cold room doors must be examined.
For laboratory electrical equipment installation there should be no extension cords or multiplug sockets present for any purpose. The power strips should be mounted off the floor and should have proper fuses in conduits. The outlets are earthed/grounded and with proper polarity. Equipment must not have frayed or damaged wiring. Function of electrical safety devices such as miniature circuit breaker (MCB) and earth-leakage circuit breaker (ELCB) should be checked. Operation and functioning of emergency and backup power systems should be checked. The record of maintenance of electrical equipment and installation and test reports of earthings should be checked. It is important to ensure that there are no electrical outlets near water sources and if present, must meet statutory codes.
Laboratory PPE should include equipment such as gloves, gowns and goggles that are available as per the requirement. If the laboratory mandate involves dealing with biohazardous and infectious material/human or animal samples, the laboratory should be equipped with higher level of PPE and there should be documentary evidence that staff is trained to use these properly. All the PPEs must be operating properly. In BSL-2 laboratory areas where there is likely possibility of aerosol hazard for eyes, the laboratory should be equipped with proper goggles and eyewash available in right locations in the laboratory. The operation of eyewash station and shower must be checked if installed. If the hazard level is high, the safety shower should be available in the laboratory. The validation committee members must check that laboratory coats, gowns, smocks, gloves and other personal protective clothing are not worn outside the laboratory. If laboratory is using liquid nitrogen refrigerators or storage containers, the PPE for cryogenic storage should be present.
Laboratory waste management should include the disposal of all kinds of waste and should be properly documented. Logbooks should be available depicting the biomedical and non-biomedical waste log per day/week, depending on the usages of the laboratory. There must be laboratory procedures and proper SOPs for waste segregation in proper containers in place. In the laboratories using radioactive materials, the waste containers should be tagged and labelled with date and kept securely closed. There should be SOPs for various other hazardous chemical wastes dealing with radioactive material and there should be documentary evidence showing that these are appropriately handled and stored till disposed18.
The laboratories using sharps should have containers for sharps and should have documentary evidence of their proper disposal. The printed procedures should be posted in laboratory for waste disposal. There should be evidence of training of staff for communication of hazards, respiratory protection and if applicable the monitoring of formaldehyde and anaesthetic gas19. There should be no evidence of storing of food for human consumption inside the laboratory. Microwave oven(s) should not be used for food preparation and exclusively used only for laboratory work. Only mechanical pipetting devices are to be used. The protective laboratory clothing should be stored separately from street clothing.
For general laboratory housekeeping all the glass containers should be stored securely below eye level, shelves or on the floor. Clean absorbent pads should be available on the work surfaces of tables. Broken glassware should be handled by mechanical means such as brush and dustpan and tongs. There should be no open penetrations in walls, ceiling and floor. The committee members should inspect the condition of walls, flooring, ceilings and other fixtures such as drain ports and water lines. The door's minimum passage width should be at least 1 m in the laboratory so that movement of bigger equipment's is easy. However, this may be more than 1 m in certain laboratory facility depending on the usages as well as risk assessment. The heated constant temperature baths should be equipped with low water level and overheat shutoff. These should also be made of non-combustible materials and should be examined for the extreme conditions202122.
For all biological safety cabinets (BSCs) there should be printed evidence of certification within last year pasted on each of the BSCs which should not interfere with room air movement. The SOPs for BSC surface disinfection should be appropriate and available. It needs to be checked and ensured that practice of surface disinfection at the beginning and end of each procedure is followed by all the laboratory personnel. The front grill and exhaust filters are unobstructed and no open flames are used inside the cabinet, particularly the laboratories dealing with bacterial agents. If the vacuum lines are provided in the BSCs, those should have in-line high-efficiency particulate air (HEPA) filters and disinfectant traps. The locations of BSCs should not be compromised by room air outlets or location not confronted with frequent movement of laboratory persons. Risk assessment is performed based on the laboratory protocols and flowcharts and used when there is potential for creating aerosols23. For decontamination of BSCs a written policy should be available for the decontaminant and a policy specific to the organism(s) used in the laboratory. There should be documentary evidences of reports submitted to the laboratory supervisor about all the spills and accidents involving infectious material. Appropriate SOP should be available for decontaminant used during spill cleanups in the laboratory premises. The work surfaces should be decontaminated before and after each procedure, daily and after spills24. A SOP should be in place for the proper handling of contaminated waste from BSCs and there should be no visual evidence of waste containers overfilled.
Waste disposal policy for culture stocks and other regulated waste being properly decontaminated before disposal is mandatory. If the laboratory does not have autoclave, there should be written policy for materials decontaminated outside the laboratory and must be transported in closed, durable, leak-proof containers according to local rules and regulations. SOPs should be written for segregation of mixed waste and biologically disinfected prior to autoclaving.
For laboratory workers’ health surveillance and protection, written policy must be available with past records of laboratory personnel appropriately immunized for the agents handled by them in the laboratory. If laboratory deals with highly biohazardous and infectious material of high consequences, there should be evidence provided for the appropriate medical services contacted for medical evaluations, surveillance and treatment of occupational exposures. SOPs and training protocols should define proper PPE usage when personnel handle infectious material or contaminated equipment18. Face protection must be provided as per the risk assessment and agents being handled by the laboratory when working outside the BSC with infectious material. Antimicrobial agent should be available for immediate first aid.
SOPs explaining the standard practices and principles for working in the Biosafety cabinets must be developed based on the risk assessment being performed for the infectious agents to be handled within the cabinets. SOPs must also be developed for laboratory processes where there are chances of infectious aerosols/splashes being created while handling higher volumes of viral stocks. Biosafety manual must be prepared and adopted in the laboratory19. It should be ensured that personnel read and follow the instructions on practices and procedures, including safety or operations’ manual. This should be reviewed annually and based on incidences should be revised intermittently. Laboratory manual should include procedures to be followed to minimize aerosols/splashes, how and where needle-locking syringes/single-use needle syringe units to be used with infectious agents, centrifuge cups and rotors opened only in a BSC, infectious specimens transported outside a BSC in approved containers following approved transport regulations.
Laboratory access control systems should be in place. There should be visual evidence of existing access control and the facility manual should define the limited and restricted access granted to authorized personnel2225. Personnel training documents must be evident of advising about all potential hazards in the laboratory. Biohazard sign must be posted on laboratory doors as appropriate. Information on the other signage such as radioactivity, fire, electrical and other such hazards should be accurate, legible and posted on all such relevant locations. Committee members should check the access control system as well as door interlocking system of anteroom, airlocks and change rooms.
For adequate laboratory facility physical inspection should include availability of a handwashing sink available near laboratory exit. Laboratory must be separated from unrestricted traffic flow in building. There must be access to laboratory through an anteroom with self-closing doors and also availability of shower based on risk assessment. All penetrations in laboratory are sealed or sealable for decontamination. BSL-3 laboratory room/s air (HEPA filtered) shall be single pass and exhausted away from occupied areas. Physical inspection should also include verification that controlled ventilation system is unidirectional airflow system in BSL-3 laboratories. However, in case of BSL-2, it should be verified that only 70 per cent air from non-laboratory areas is recirculated, but newly commissioned BSL-2 may have 100 per cent exhaust system. Environmental parameters of laboratory area (room temperature, humidity, pressure and room air changes per hour) should be as per requirements. It should be verified that the supply and exhaust systems of the laboratory are interlocked to prevent positive pressurization of the laboratory in case of accidental or mechanical failure of the exhaust system. The decontamination procedure and handling of contaminated HEPA filters should be checked and verified. The maintenance of heating, ventilation, and air conditioning system (HVAC), and related records20 should be checked and verified.
For laboratory personal protection physical inspection should verify that closed-front gowns are worn in laboratory and protective laboratory clothing are worn only in laboratory areas. Hand-washing sink should either be automatically controlled or foot or elbow operated. Laboratory protocols, manuals and training material should be available for usage of double gloves when handling infectious material or potentially contaminated equipment and work surfaces. Based on risk assessment in the laboratory, the respiratory protection is implemented by all personnel in the laboratory when aerosols are not safely contained in a BSC. Laboratory protocols, manuals and training material should be evident of implementation of mucous membrane protection when working with infectious material outside a BSC and personnel advised of special hazards associated with the agent(s) as per the mandate of the laboratory. There should be written consents available in the records that the personnel have read and will follow all instructions on practices and procedures, including safety or operations’ manual of the laboratory. Records should also include that personnel receive annual updates/additional training for procedural changes and follow proper autoclaving procedure for decontaminating the contaminated waste prior to disposal. The autoclave vacuum lines in BSL-3 laboratories should be protected with HEPA filters. All records and operations of autoclaves should be examined. The availability, functioning and records of effluent decontamination system available in the BSL-3 should be checked and verified.
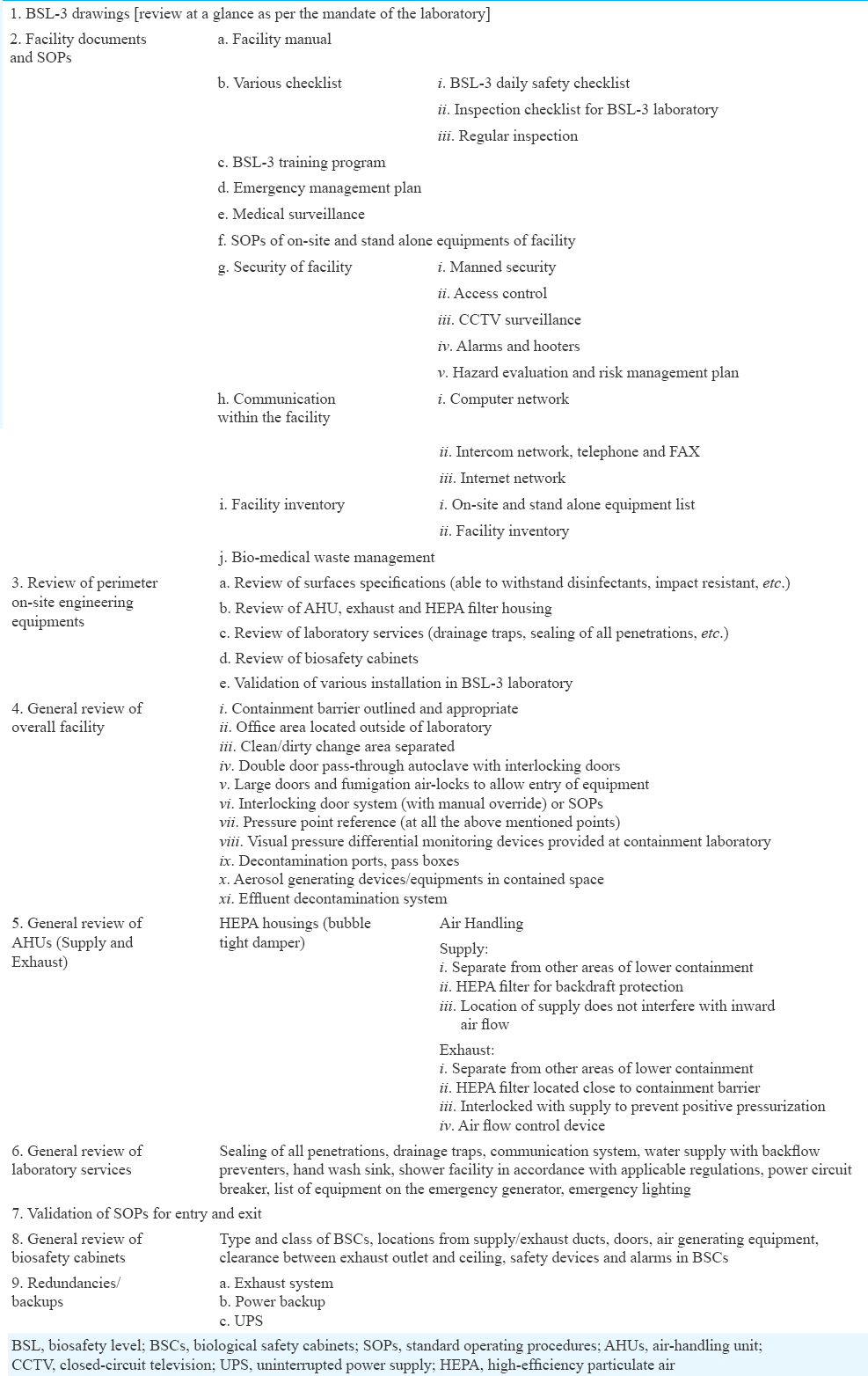
There are no standards available for validating and certification of physical facilities such as containment laboratories; this is because every facility is unique for its physical features suited as per the mandates and objectives of that laboratory. The Table II provides salient points which need to be considered for certification and validation of a biosafety laboratory.
In a country like India, attempts made for making generalized guidelines, may not be useful until and unless biosafety experts physically examine the integrity of physical facility as per the minimum required standards for biocontainment6 in terms of PPEs, workplace practices, administrative controls, engineering controls and laboratory management data and interpret and judge rightly suggesting that facility meets or not the required norms and there is no possibility of breach in biosafety and biosecurity on the part of engineering controls as well as in laboratory management systems and procedure.
Conclusion
To summarize, certification covers the assessment of physical aspects of the bio-containment facility while validation encompasses the review of processes and procedures to be followed in the containment laboratory including protocols, SOPs and competence records of training staff. Other significant aspects under certification and validation include stand-alone equipments, and installations, documents and records pertaining to the facility (access controls, BSL-3 entry-exit sheet logs, daily checklist logs including laboratory maintenance and management, daily duties of cleaning staff, equipment maintenance status and placements as per the expected workload), work flow in laboratory and availability of associated SOPs and emergency response plan. It also includes telephone extension numbers, defined and appropriately located and responsibilities assigned, training protocols and staff assessment records, SOP of complete facility, SOPs of all the equipment and of all the important process of the laboratory. Role of management is very important during certification and validation process to ensure that the laboratory is certified and validated prior to its use.
Conflicts of Interest: None.
References
- Establishment of Biosafety Level-3 (BSL-3) laboratory: Important criteria to consider while designing, constructing, commissioning & operating the facility in Indian setting. Indian J Med Res. 2014;140:171-83.
- [Google Scholar]
- Centers for Disease Control and Prevention and National Institutes of Health. In: Biosafety in microbiological and biomedical laboratories (5th ed). Washington: U.S. Government Printing Office; 2007.
- [Google Scholar]
- Anthology of biosafety II. Facility design considerations. Mundelein: American Biological Safety Association; 2000.
- 2006. Biorisk Management: Laboratory Biosecurity Guidance. Available from: http://www.who.int/ihr/biosafety/publications/en/index.html
- Regulatory compliance of a BSL-3 laboratory unit in a drug discovery environment. Appl Biosaf. 2007;12:208-85.
- [Google Scholar]
- Laboratory biosafety manual (3rd ed). Geneva: WHO; 2004.
- National Institutes of Health Biosafety Level 3 Laboratory Certification Requirements. Available from: https://www.scribd.com/document/339576674/BSL3CertificationGuidelinesFINAL-508
- [Google Scholar]
- Health Laboratory Technology Unit. Safety in health-care laboratories. Geneva: WHO; 1997.
- [Google Scholar]
- Feasibility of establishing a biosafety level 3 tuberculosis culture laboratory of acceptable quality standards in a resource-limited setting: An experience from Uganda. Health Res Policy Syst. 2015;13:4.
- [Google Scholar]
- Laboratory Biorisk Management Strategic Framework for Action 2012-2016 2012 WHO/HSE/2012.3. Enhancement of laboratory biosafety (WHA58.29)
- 1.3: Warning Signs for Radiation Sources. Radiation and Nuclear Safety Authority. 2013.
- Laboratory Safety Guidance. Occupational Safety and Health Administration U.S. OSHA 3404-11R. Washington: Department of Labor; 2011.
- Effectiveness of UV exposure of items contaminated with anthrax spores in a class 2 biosafety cabinet and a biosafety level 3 laboratory pass-box. Appl Biosaf. 2008;13:164-8.
- [Google Scholar]
- Design Guidelines for Blood Centres 2010
- Division of Environmental Health and Safety Office of Business Affairs. University of Florida; Revised May 2013. Laboratory Safety Manual. Available from: http://webfiles.ehs.ufl.edu/labsafe.pdf
- Biosafety breaches. Accidents spur a closer look at risks at biodefense labs. Science. 2007;317:1852-4.
- [Google Scholar]
- Practices, procedures, facilities, and safety equipment for BSL-3 and BSL3/2 laboratories. Available from: https://www.aiha.org/aihce02/handouts/fm239kowalewsky3.pdf
- Framework for leadership and training of Biosafety Level 4 laboratory workers. Emerg Infect Dis. 2008;14:1685-8.
- [Google Scholar]
- Environment Health and Safety; University of Washington. Available from: http://www.ehs.washington.edu/rbsbiosafe/BSM.pdf
- Public Health Mycobacteriology: A Guide for the Level III Laboratory. Atlanta, GA: Centers for Disease Control; 1985.
- U.S. Department of Health and Human Services, Public Health Service, Centers for Disease Control and Prevention, and National Institute of Health. In: Biosafety in Microbiological and Biomedical Laboratories (4th ed). Washington: US Government Printing Office Sec. III; 1999. p. :27-36.
- [Google Scholar]
- Primary containment for biohazards: Selection, installation and use of biological safety cabinets (2nd ed). Washington, DC: U.S. Department of Health and Human Services/Centers for Disease Control and Prevention/National Institutes of Health; 2000.
- 2016. NIH Guidelines for Research Involving Recombinant or Synthetic Nucleic Acid Molecules. Available from: https://osp.od.nih.gov/wp-content/uploads/NIH_Guidelines.html






