Translate this page into:
Cancer stem cells in hepatocellular carcinoma - an immunohistochemical study with histopathological association
Reprint requests: Dr Banumathi Ramakrishna, Department of Pathology, Christian Medical College, Vellore 632 004, Tamil Nadu, India e-mail: banu@cmcvellore.ac.in
-
Received: ,
This is an open access article distributed under the terms of the Creative Commons Attribution NonCommercial ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non commercially, as long as the author is credited and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Background & objectives:
Cancer stem cells (CSCs) may be responsible for tumour recurrence and resistance to chemotherapy in hepatocellular carcinoma (HCC). This study was carried out to evaluate the association between histological parameters and liver CSCs (LCSC) in HCC, and to compare distribution of liver CSCs in HCC associated with and without hepatitis B virus (HBV) infection.
Methods:
Seventy nine tumours (49 surgical resections from 46 patients, and 30 from autopsy) were reviewed. Immunohistochemical staining for the LCSC marker EpCAM (epithelial cell adhesion molecule), liver progenitor cell (LPC) markers CK19 (cytokeratin 19) and neural cell adhesion molecule (NCAM) were performed and were associated with histological features of tumour behaviour.
Results:
Thirty three tumours (41.8%) showed positive staining for EpCAM. CK19 and NCAM expression were seen in 26 (32.9%) and four (5.1%) tumours, respectively. The expression of EpCAM and CK19 was significantly associated with each other (P<0.001). EpCAM expression was significantly associated with clinical and histological features indicating aggressive tumour behaviour, including younger age of onset, higher serum alpha foetoprotein (AFP) levels, tumour cell dedifferentiation, increased mitotic activity, and vascular invasiveness. There was no significant difference in expression of EpCAM, CK19 and NCAM between HBV positive and negative HCC.
Interpretation & conclusions:
The LCSC marker EpCAM was expressed in less than half of HCC, was independent of HBV aetiology, and was strongly associated with clinical and histological features of aggressive tumour behaviour. Positive staining for CK19 suggests a possible LPC origin of the EpCAM positive HCCs.
Keywords
Cancer stem cells
CK19
EpCAM
liver
NCAM
progenitor cells
Hepatocellular carcinoma (HCC) is the most common primary malignancy of the liver and is particularly common in sub-Saharan Africa and Eastern Asia and is now increasingly seen in previously low incidence developed countries12. Approximately 80 per cent of HCC are secondary to chronic hepatitis B virus (HBV) or hepatitis C virus (HCV) infection1. Despite recent advances in early detection and curative treatments, the overall prognosis of patients with HCC remains dismal. This is due to the presence of underlying cirrhosis and liver failure in a majority of cases, as well as the high level of resistance exhibited by the tumour cells to traditional therapeutic modalities like chemotherapy and radiotherapy234.
In HCC, as in several other cancers, there appears to be a distinct subpopulation of cells exhibiting properties consistent with stemness - self renewal, cell proliferation and cell survival. These are called the tumour initiating cells (TICs) or cancer stem cells (CSCs)56. It is believed that the CSC population within a tumour determines critical aspects of tumour biology including invasion, metastasis, and resistance to chemotherapy and radiation therapy. Identification of CSC distribution and frequency within tumours may thus identify aggressive tumours and may help to eventually prognosticate tumours and to tailor therapy. Many surface proteins have been suggested to be markers for CSC in HCC including CD13, CD90 and CD133789. Epithelial cell adhesion molecule (EpCAM or CD326) is a consensus candidate surface marker for liver CSCs (LCSCs) and its expression has been demonstrated on HCC subpopulations exhibiting LCSC properties1011. The cell of origin of LCSCs is yet to be ascertained, and there is speculation that these may arise from adult liver or liver progenitor cells (LPCs) that reside in the canals of Hering12. LPCs may be identified by the surface markers neural cell adhesion molecule (NCAM, CD56) and cytokeratin19 (CK19)613.
The present study was aimed to characterize the pattern and distribution of LCSCs and LPCs in HCC using immunohistochemical staining of tumour specimens retrieved at resection or autopsy. The secondary objectives of the study were to relate the presence and distribution of LCSCs with histological findings, and to compare distribution of LCSCs in HBV-positive and HBV-negative HCC.
Material & Methods
The material for this study included autopsy cases of HCC, surgically resected HCC specimens, and explant livers containing HCC, received at the department of Pathology, Christian Medical College and Hospital, Vellore, Tamil Nadu, India. Thirty autopsy cases of HCC in which adequate blocks were available, seen over a span of 27 yr from August 1985 till March 2012, were included in this study. The surgical pathology and the autopsy reports were taken from the Pathology online database (maintained since the year 2001) or from the department registry for earlier years. Forty nine HCC specimens from 46 patients treated consecutively by segmental resection, partial hepatectomy or orthotopic liver transplantation (OLT), received over a span of 14 yr from January 1998 to March 2012, constituted the surgical group of cases in this study. This group included seven explant livers and three recurrent tumours arising in patients who had undergone previous surgical resection of primary HCC. Altogether, the study population consisted of 79 cases of HCC including 30 autopsy cases and 49 tumours from 46 patients in the surgical group.
Slides and blocks were retrieved from the archives of the department of Pathology, reviewed and representative blocks of tumour as well as adjacent liver were selected for further study. All specimens had been fixed in 10 per cent formalin, embedded in paraffin and four micron (4 μ) thick sections were cut.
For each case, the number of sections examined ranged from 5 to 40 with a mean of 11.8 sections per case. The slides were routinely stained with haematoxylin and eosin (H&E). Special stains, including Foot's reticulin, van Gieson, periodic acid Schiff with or without diastase digestion, orcein and Perl's Prussian blue stains, were used when necessary.
Clinical and laboratory information: The relevant clinical details were abstracted from the biopsy and autopsy records. The laboratory details noted included serological marker status for HBsAg, HCV antibody and serum levels of alpha foetoprotein (AFP), wherever available. The radiological findings were noted with emphasis on tumour size and number, patency of portal vein and the presence of distant metastasis.
Pathological assessment: The gross and microscopic assessment included both the tumour and the non-tumour liver parenchyma. The tumours were categorized as unifocal or multifocal (the latter may represent a multicentric origin or intrahepatic metastasis from a primary tumour). A tumour was described as massive when replacing an entire lobe with or without satellite nodules. When numerous cirrhosis like nodules were present, it was described as diffuse. A tumour was termed multinodular when there were multiple discrete tumour nodules scattered throughout the liver and none of which were massive1415. The findings recorded were tumour location, size, number, degree of tumour differentiation15, presence of microvascular invasion (MVI), portal vein invasion (PVI), bile duct invasion, perineural invasion, mitotic activity with a cut off-value of 5/10HPF (high power field) to designate tumours into low or high mitotic rate categories and presence or absence of underlying cirrhosis.
Immunohistochemistry: Immunohistochemical (IHC) staining for EpCAM, CK19 and NCAM (CD56) were carried out on selected blocks of all 79 tumours included in this study using mouse monoclonal antibodies (RTU-ESA, clone VU-1D9, for EpCAM; NCL-LCD56-1B6, clone 1B6 for NCAM; and NCL-CK19, clone b170 for CK19; all from Novocastra, Leica Biosystems, Melbourne, Australia). IHC staining was carried out using the Envision kit (K5007, Dako, Glostrup, Denmark) according to the manufacturer's instructions. Antigen expression for all three immuno- histochemical markers was defined as positive when staining was present on the tumour cell membranes. Cytoplasmic staining alone without membranous staining was considered as negative. Internal positive control was biliary ductular epithelium in adjacent liver for all three immunomarkers and also nerve bundles for NCAM. EpCAM expression was evaluated using Spizzo's scoring system16. A total immunostaining score (TIS) was calculated as the product of a proportion score (PS) and an intensity score (IS). Scores of 0,1+, 2+, 3+ and 4+ were assigned respectively to none, <10, 10-50, 51-80 and >80 per cent proportion of positive staining, tumour cells. The staining intensity was assessed as 0-3 for absent, weak, moderate and strong staining, respectively. EpCAM expression was analysed categorically as weak (TIS upto 4), moderate (TIS of 6 & 8), and intense (TIS of 9 & 12). CK19 and NCAM expressions were also evaluated based on the proportion of tumour cells showing moderate to strong membranous staining for the antigens.
The study protocol was approved by the institutional review board.
Statistical analysis: Student t test was used to compare continuous variables while chi-square test and Fisher's exact test were used as appropriate for comparing categorical variables between groups.
Results
The mean age of the patients at presentation was 50 ± 15.3 yr. There was a marked male preponderance (male:female ratio 5.3:1). The details of clinical presentation were available for 44 patients in the surgical group and for 29 cases in the autopsy group. Abdominal pain (47.7%) and abdominal mass (43.2%) were the commonest symptoms at presentation in patients who underwent surgery while jaundice and ascites (79.3%) followed by anorexia/weight loss (51.7%) and encephalopathy (44.8%) were the commonest features in the autopsy cases.
Serum alpha foetoprotein (AFP) levels were significantly elevated (>300 IU/ml) in 10 of 37 surgical patients and in eight of nine autopsy cases. The major aetiological factor identified was HBV infection, accounting for 41 (57.8%) of the 71 cases in which viral marker status was investigated. Alcoholic liver disease accounted for 16 cases and HCV infection for only three cases. There was one case each of tyrosinemia and Budd-Chiari syndrome leading to chronic liver disease and HCC. Alcohol intake and diabetes mellitus were found to be the leading co-morbidities (9 cases each) in HBV-related HCC patients.
Tumour characteristics-gross and microscopic: Of the 79 tumours, 31 (39.24%) were unifocal lesions, three (3.8%) of which were massive solitary tumours. Of the remaining 48 (60.8%) multifocal tumours (23 in surgical and 25 in autopsy groups), 11 (13.9%) were massive with satellite nodules, seven (8.9%) were of the diffuse type and 30 (38%) were multinodular. The tumour sizes ranged from 0.4 to 22 cm in maximum dimension, with a median of 6 cm. The majority (43, 55.1%) of the tumours were confined to the right lobe, 21 (26.9%) were confined to the left lobe, while 14 (17.95%) involved both the lobes and in one case detail was not available.
The majority of tumours in the surgical (34) and in the autopsy groups (21) were moderately differentiated HCCs (69.7%) and two tumours in the surgical group also had a focus of cholangiocarcinoma; well differentiated and poorly differentiated HCCs accounted for 16 (20.3%) and eight (10.1%) cases, respectively (Fig. 1a-c). The latter included one case of undifferentiated tumour in the autopsy group. A high mitotic activity of >5/10HPF was observed in 48 tumours including all the poorly differentiated tumours.
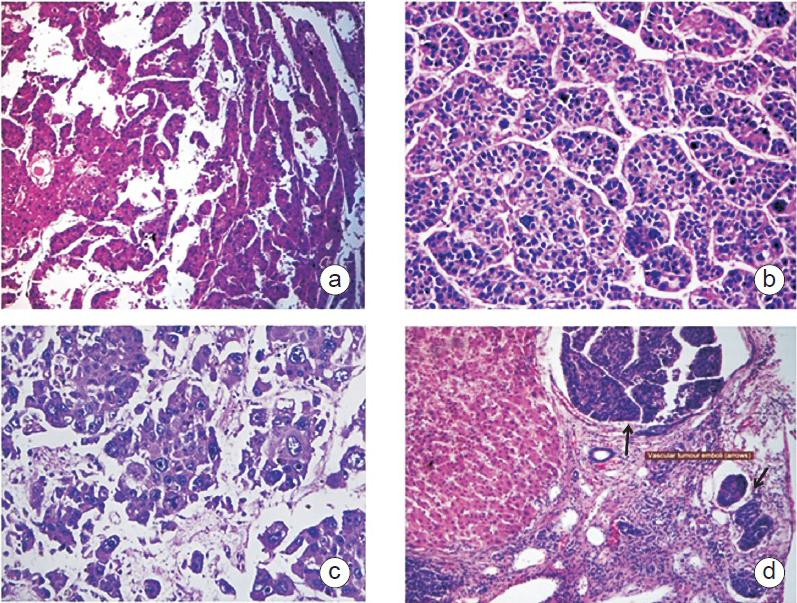
- Hepatocellular carcinoma. (a) Well differentiated, H&E 100X, (b) Moderately differentiated, H&E 200X, (c) Poorly differentiated H&E 200X (d) Microvascular invasion (arrows) H&E100X.
Microvascular invasion (Fig. 1d) was more common in the autopsy group (29 of 30) compared to the surgical group (35 of 49) (P<0.01). Thrombosis of portal vein or its branches was more common in autopsy cases (23 of 30) compared to surgical group (3 of 49 cases) (P<0.001). Bile duct invasion was not significantly different between autopsy group (2 of 30 and surgical group (7 of 49). Two cases in the autopsy group showed perineural invasion.
All 30 tumours in the autopsy group and 20 of the 49 in the surgical group had underlying established cirrhosis. Of the 29 cases in the surgical group without established cirhhosis, six had Ishak17 fibrosis score of 4 to 5, nine had score of 2 to 3 and 14 had score of 0 (no fibrosis). Liver histology in the 14 cases without fibrosis revealed presence of mild steatosis in 11 cases which was macrovesicular in six, microvesicular in two and mixed macro- and microvesicular in three cases. A granulomatous reaction was observed in the adjacent liver parenchyma in six cases, four non-necrotizing granulomas, probably reactive and two were of the foreign body type. There were no dysplastic lesions detected in both cirrhotic and non-cirrhotic cases.
Distant metastasis in autopsy cases: Sixteen cases had documented evidence of distant metastasis, of whom 10 had disseminated metastasis. The most frequent site for metastasis was the lung (8) followed by heart and adrenal/supra renal region five each, lymph nodes three and oesophagus, gall bladder and diaphragmatic peritoneum one each.
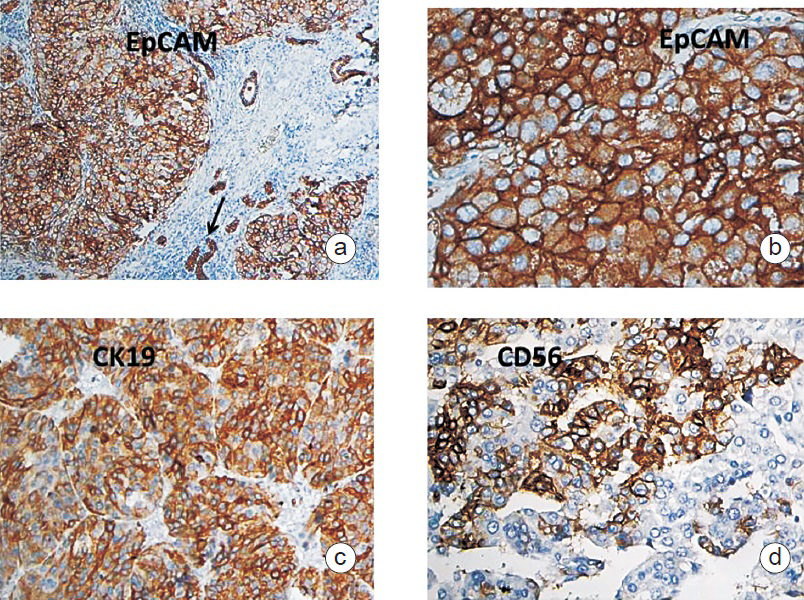
Immunohistochemical expression of LCSC and LPC surface markers: Thirty three (41.8%) of the 79 HCCs, comprising 16 (32.7%) in the surgical group and 17 (56.7%) tumours in the autopsy group, showed positive staining for EpCAM. Subgrouping of the 33 EpCAM positive HCCs, according to the TIS for EpCAM, showed an equal distribution of tumours across the three categories. One third of the tumours (n=11, 7 surgical & 4 autopsy) showed intense expression of EpCAM (Fig. 2a, b) with TIS of 9 and 12. One third of the tumours (n=11, 5 surgical and 6 autopsy) exhibited moderate expression of EpCAM with TIS of 6. The remaining one third of tumours showed only weak expression (n=11, 4 surgical & 7 autopsy) with TIS of <4.
-
a. Tumour cells and bile ductules (arrow-internal control) showing strong membranous staining for EpCAM, Immunohistochemistry100X. b. High power showing EpCAM positive tumour cells, Immunohistochemistry 400X. d. Tumour cells showing strong membranous staining for CK19, Immunohistochemistry100X. d. Tumour cells showing strong membranous staining for CD56, immunohistochemistry 400X.
Twenty six (32.9%) of the 79 tumours [12 (24.5%) from the surgical and 14 (46.7%) from the autopsy groups] were positive for CK19 (Fig. 2c). Expression of NCAM (Fig. 2d) was found only in four (5.1%) tumours; two each from the surgical and the autopsy groups. Twenty three of 33 EpCAM positive tumours stained positive for CK19, of which two also stained positive for NCAM. The distribution of staining patterns is shown in Fig. 3.
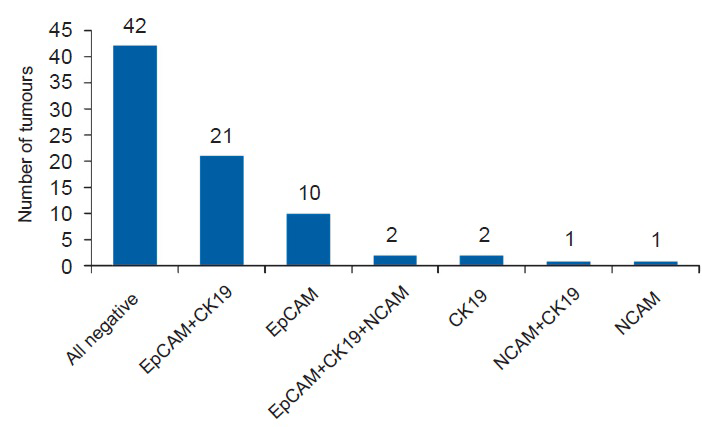
- Distribution of tumours according to immunohistochemical staining pattern (n=79). EpCAM, epithelial cell adhesion molecule; CK19, cytokeratin 19; NCAM, neural cell adhesion molecule.
Of the three patients with recurrent tumours, one showed negative staining for all three markers in both the original and recurrent tumours. Another patient had similar expression for EpCAM (TIS 12) and CK19 (intense) in original and recurrent tumours with negative staining for CD56. The third patient had TIS of 9 and 4 for EpCAM, respectively in the original and the recurrent tumours and intense expression for CK19 and negative for CD56. MVI was present in both original and recurrent tumours in the first two patients and in the third it was seen only in the original tumour.
Association of LCSC and LPC marker expression with HCCs: There was significant association between immunohistochemical expression of LCSC marker EpCAM and LPC marker CK19 (P<0.001). Twenty three of the 33 EpCAM positive tumours (69.7%) were also positive for CK19. Positive expression of CK19 was found in only three of the 46 EpCAM negative tumours (6.5%). Of the four NCAM positive tumours, two were EpCAM positive and two were EpCAM negative.
Association of LCSC marker expression with clinical parameters: EpCAM expression was associated with tumours occurring at a younger age. The mean age of 31 patients with EpCAM positive HCCs was 44.4 ± 15.5 yr compared to 54.2 ± 14 yr for patients with EpCAM negative tumours (P<0.01). EpCAM expression was significantly associated with high serum AFP levels. Of the 37 patients in whom AFP levels were measured, high levels of serum AFP were detected in six of 11 patients with EpCAM positive tumours compared to four of 26 patients with EpCAM negative tumours (P<0.05).
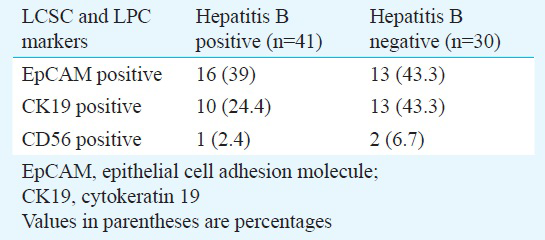
Association of LCSC and LPC marker expression with HBV aetiology of HCC: There was no significant difference in expression of EpCAM, CK19 and NCAM between HBV positive and HBV negative HCCs (Table I).
Association of LCSC marker expression with histological parameters: Expression of EpCAM in HCCs was significantly associated with histological parameters of tumour behaviour including degree of differentiation, presence of MVI, PVT and mitotic activity (Table II). Presence of intrahepatic metastasis and background cirrhosis did not show significant difference between EpCAM positive and EpCAM negative tumours (Table II).
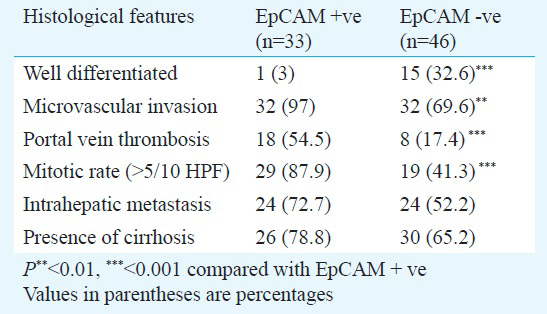
Degree of tumour differentiation: EpCAM expression was associated with loss of mature hepatocytic differentiation. Only one of the 16 well differentiated tumours was EpCAM positive, compared to 25 (45.5%) of 55 moderately differentiated tumours, and seven of eight poorly differentiated tumours (P<0.001).
Microvascular invasion: Thirty two of the 64 tumors with MVI (35 surgical and 29 autopsy) were EpCAM positive (15 surgical and 17 autopsy) compared to one of 15 tumours without microvascular invasion (P<0.01). All EpCAM positive tumours with elevated serum AFP levels (6 surgical cases) showed presence of MVI on histopathological examination.
Portal vein thrombosis: Eighteen of 26 tumours with PVT were EpCAM positive compared to 15 of 59 tumours without portal vein thrombosis (P<0.001).
Mitotic rate: Among the 48 (26 surgical and 22 autopsy) tumours with mitotic activity higher than 5/10HPF, 29 (60.4%) (13 surgical and 16 autopsy) were EpCAM positive, indicating a high degree of association between increased mitotic activity and EpCAM positivity (P<0.01).
Intrahepatic metastasis: The possible association between EpCAM expression and presence of intrahepatic metastasis in HCCs was evaluated. Of the 48 multifocal tumours (23 surgical and 25 autopsy), 24 (50%) (10 surgical and 14 autopsy) were EpCAM positive (P<0.05).
Background cirrhosis: Of the 56 tumours which arose in cirrhotic livers, 26 (46.4%) were EpCAM positive. There was no significant association between EpCAM expression and presence or absence of background cirrhosis in HCCs.
Association of EpCAM expression in HCCs with presence of distant metastasis: Among the 16 autopsy cases with documented metastasis, 11 tumours were EpCAM positive and five were EpCAM negative but the difference was not significant. This was probably due to the overall small number of patients in this group.
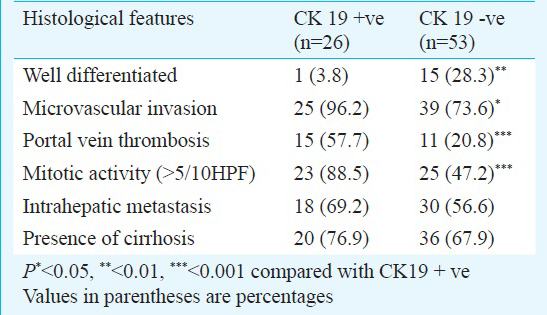
Association of LPC marker (CK19) expression with histological parameters: Expression of CK19 in HCCs was found to be significantly associated with certain histological parameters of tumour behaviour including degree of differentiation (P<0.01), MVI (P<0.05), PVT (P<0.001) and mitotic activity (P<0.001). There was no significant association between CK19 immunoreactivity and presence of intrahepatic metastasis or background cirrhosis (Table III).
Stratification of LCSC derived HCCs based on LPC marker expression: In the present study, 23 tumours were positive for both EpCAM and CK19, while 10 expressed only EpCAM but not CK19. There was no significant association between the above two groups with respect to MVI, PVT, mitotic activity or degree of tumour differentiation.
Discussion
HCCs are heterogenous tumours with a propensity for recurrence even after surgery or transplantation18. These tumours are thought to be initiated and sustained by a distinct subpopulation of CSCs61011, which may determine its behaviour patterns including invasion, metastasis, heterogeneity, recurrence, and resistance to radiotherapy and chemotherapy. EpCAM is one of the markers that identify CSCs within a tumour1920. Signaling pathways in HCC in Indian patients may be different from those in the West2122, underscoring the importance of re-examining the biological correlates of CSC and HCC in this population.
In our study over 40 per cent of HCCs exhibited expression of EpCAM, within the range of EpCAM expression of 10 to 40 per cent reported in other populations162324. Spizzo et al16 reported overexpression of EpCAM in 14 per cent of HCCs in their population; in our study we found overexpression in 27.8 per cent of the tumours.
EpCAM expression in HCC was significantly associated with features of more aggressive biologic behaviour in this study, including younger age of onset, higher serum AFP levels, greater tumour cell dedifferentiation, increased mitotic activity in tumours, and vascular invasiveness. Metastases, either intrahepatic or distant, were more often of EpCAM expressing tumours, although this association did not reach statistical significance. This could be probably due to the small number of cases in each subgroup of surgical and autopsied cases.
EpCAM expression was associated in more than two thirds of our cases with expression of the liver progenitor cell marker CK19. This is consistent with a liver progenitor cell lineage origin for liver CSC. Other studies have also suggested that HCCs with progenitor cell origin have worse prognosis1925 and that EpCAM and CK19 expressions were associated with vascular invasion and poorly differentiated tumours1926.
HBV infection followed by alcoholism were the major aetiological factors associated with HCC in this study. There was no association between EpCAM and CK19 expression and factors associated with aetiopathogenesis or with background cirrhosis. In contrast, Villanueva et al26 had shown that hepatitis B associated liver damage was enriched with CK19 signatures. Mutations in beta-catenin, which are noted in patients from West with HBV-related HCC, may be important in maintenance and renewal of certain types of CSCs. It is possible to speculate that the lack of enrichment in CK19 positive cells in HBV-related HCC may be related to the rarity of beta-catenin mutations in Indian patients with HBV-related HCC22.
The majority of the tumours in this study were multifocal (60.8%). Among the multifocal tumours, most (30) were multinodular with only seven being of the diffuse type. This is in concordance with the study by Yuki et al27 where multinodular and diffuse types of HCC accounted for 48.1 and 10.5 per cent of cases, respectively. Multifocality, which denotes intrahepatic metastasis of HCC, was predominantly seen in the autopsy group (83.3%).
Further stratification of EpCAM positive HCCs based on their CK19 expression status did not reveal any significant difference between their histological parameters of behaviour. It is, therefore, possible that all EpCAM positive cells arise from LPCs, but that about half of them lose expression of CK19 during the process of tumourigenesis.
In conclusion, this study has demonstrated the definite presence of LCSC marker EpCAM expression in less than half of the HCCs in the Indian population. As expected of a CSC derived tumour, LCSC marker positive HCCs in this study were strongly associated with clinical and histological features of aggressive tumour behaviour such as high serum AFP levels, early occurrence, poor degree of differentiation, presence of MVI and PVT and high mitotic rates. The expression pattern of LCSC marker EpCAM was closely associated with that of LPC marker CK19, pointing towards a possible LPC origin of at least some of the LCSC marker positive HCCs. However, CK19 expression status did not significantly affect the pathobiologic profile of EpCAM positive HCCs implying that irrespective of their cell of origin, LCSCs imparted characteristic properties to the tumours expressing them, In addition, LCSC expression was found to be independent of aetiology of HCC. Demonstration of EpCAM positive subset of HCCs can have future implications in the development of targeted therapeutics.
Acknowledgment
Authors acknowledge Shri Prasanna Samuel, Department of Biostatistics, Christian Medical College, Vellore, for assistance in statistical analysis. This study was supported by Fluid Research Grant from Christian Medical College, Vellore.
Conflicts of Interest: None.
References
- Epidemiology of viral hepatitis and hepatocellular carcinoma. Gastroenterology. 2012;142:1264-73.
- [Google Scholar]
- Hepatocellular carcinoma: current trends in worldwide epidemiology, risk factors, diagnosis and therapeutics. Hepat Med. 2012;4:19-37.
- [Google Scholar]
- Emerging approaches in hepatocellular carcinoma. J Clin Gastroenterol. 2007;41:839-54.
- [Google Scholar]
- Stem cells in liver diseases and cancer: recent advances on the path to new therapies. Hepatology. 2012;55:298-306.
- [Google Scholar]
- The biology of cancer stem cells and its clinical implication in hepatocellular carcinoma. Gut Liver. 2012;6:29-40.
- [Google Scholar]
- CD13 is a therapeutic target in human liver cancer stem cells. J Clin Invest. 2010;120:3326-39.
- [Google Scholar]
- Significance of CD90+ cancer stem cells in human liver cancer. Cancer Cell. 2008;13:153-66.
- [Google Scholar]
- Identification and characterization of tumorigenic liver cancer stem/progenitor cells. Gastroenterology. 2007;132:2542-56.
- [Google Scholar]
- EpCAM-positive hepatocellular carcinoma cells are tumor-initiating cells with stem/progenitor cell features. Gastroenterology. 2009;136:1012-24.
- [Google Scholar]
- EpCAM, a new marker for cancer stem cells in hepatocellular carcinoma. J Hepatol. 2010;52:280-1.
- [Google Scholar]
- Liver stem/progenitor cells in the canals of Hering: cellular origin of hepatocellular carcinoma with bile duct tumor thrombi? Stem Cell Rev. 2010;6:579-84.
- [Google Scholar]
- Hepatocellular carcinoma with progenitor cell features distinguishable by the hepatic stem/progenitor cell marker NCAM. Cancer Lett. 2011;309:95-103.
- [Google Scholar]
- WHO Classification of tumours of the digestive system. (4th ed). Lyon, France: International Agency for Research on Cancer; 2010.
- [Google Scholar]
- Tumours and tumourlike lesions of the liver. In: Burt A, Portmann B, Ferrell L, eds. MacSween's pathology of the liver (6th ed). Edinburgh: Churchill Livingstone; 2012. p. :761-88.
- [Google Scholar]
- EpCAM expression in primary tumour tissues and metastases: an immunohistochemical analysis. J Clin Pathol. 2011;64:415-20.
- [Google Scholar]
- Impact of stem cell marker expression on recurrence of TACE-treated hepatocellular carcinoma post liver transplantation. BMC Cancer. 2012;12:584.
- [Google Scholar]
- Human hepatocellular carcinomas with “stemness”-related marker expression: keratin 19 expression and a poor prognosis. Hepatology. 2011;54:1707-17.
- [Google Scholar]
- Angiogenesis and clinicopathologic characteristics in different hepatocellular carcinoma subtypes defined by EpCAM and alpha-fetoprotein expression status. Med Oncol. 2011;28:1012-6.
- [Google Scholar]
- Hepatitis B virus associated hepatocellular carcinoma from India: role of viral genotype and mutations in CTNNB1 (beta-catenin) and TP53 genes. J Gastrointest Cancer. 2011;42:20-5.
- [Google Scholar]
- EpCAM and alpha-fetoprotein expression defines novel prognostic subtypes of hepatocellular carcinoma. Cancer Res. 2008;68:1451-61.
- [Google Scholar]
- Expression and role of epithelial cell adhesion molecule in dysplastic nodule and hepatocellular carcinoma. Int J Oncol. 2012;41:2150-8.
- [Google Scholar]
- A novel prognostic subtype of human hepatocellular carcinoma derived from hepatic progenitor cells. Nat Med. 2006;12:410-6.
- [Google Scholar]
- Combining clinical, pathology, and gene expression data to predict recurrence of hepatocellular carcinoma. Gastroenterology. 2011;140:1501-12.e2.
- [Google Scholar]
- Growth and spread of hepatocellular carcinoma.A review of 240 consecutive autopsy cases. Cancer. 1990;66:2174-9.
- [Google Scholar]






