Translate this page into:
Assessment of striatal & postural deformities in patients with Parkinson's disease
Reprint requests: Dr Sanjay Pandey, Department of Neurology, Room No. 507, Academic Block, GB Pant Hospital, New Delhi 110 002, India e-mail: sanjaysgpgi2002@yahoo.co.in
-
Received: ,
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Background & objectives:
Though striatal and postural deformities are known to occur commonly in atypical Parkinsonism patients, these may also be seen in patients with Parkinson's disease (PD). These are frequently misdiagnosed as joint or orthopaedic pathology leading to unnecessary investigations. This study was conducted to observe the various striatal and postural deformities among patients with PD in India.
Methods:
This study was conducted at a tertiary care teaching institute in north# India. Seventy consecutive patients with PD diagnosed as per the modified UK Brain Bank criteria were included. Various striatal (hand & foot) and postural (antecollis, camptocormia, scoliosis & Pisa syndrome) deformities and their relation with the duration of disease, severity [measured by the Unified Parkinson's Disease Rating Scale (UPDRS)] and levodopa intake were analyzed.
Results:
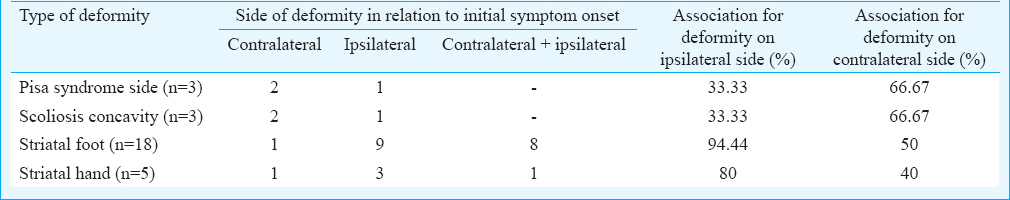
Of the 70 patients with PD, 34 (48.57%) had either striatal or postural deformities. Striatal foot was the most common deformity observed (25.71%). Camptocormia was the second most common deformity (20%). Striatal and postural deformities were seen in more advanced PD as suggested by significantly higher UPDRS and Hoehn and Yahr scale (P<0.001). Striatal deformities were more ipsilateral to PD symptom onset side (agreement 94.44%). Pisa and scoliosis concavity were more on contralateral side to PD symptoms onset side (66.67%).
Interpretation & conclusions:
Our results showed that striatal and postural deformities were common and present in about half of the patients with PD. These deformities we more common in patients with advanced stage of PD.
Keywords
Camptocormia
dyskinesias
Pisa syndrome
scoliosis
striatal foot
Propensity to bend forward is an important clinical feature in patients with Parkinson's disease (PD). As the disease progresses, many patients develop striatal and postural deformities which include striatal hands, striatal foot, antecollis, camptocormia, Pisa syndrome and scoliosis1. However, these deformities are seen more commonly among atypical Parkinsonism such as multisystem atrophy, progressive supranuclear palsy and drug-induced Parkinsonism. The pathogenesis of these deformities is a combination of ongoing Parkinsonian symptoms such as rigidity and bradykinesia, musculoskeletal changes, dystonia and use of dopaminergic medications23. These deformities increase the morbidity of patients by postural instability, gait problems, increased falls and reduced dexterity leading to disability in the activities of daily living1. These deformities are frequently misdiagnosed as rheumatoid arthritis, Dupuytren's contracture, trigger finger, equinovarus deformity, etc2. The objective of this study was to describe the clinical features of these deformities in Indian patients with PD.
Material & Methods
The study was conducted at Govind Ballabh Pant Institute of Postgraduate Medical Education and Research, New Delhi, India a tertiary care teaching institute from 2011 to 2014. The study was approved by institute's Review and Ethical Committee. A written informed consent was taken from all patients.
Over a period of three years, 70 consecutive patients with PD fulfilling the United Kingdom Brain Bank criteria4 were evaluated in detail for symptomatology, side of onset, duration, drug history along with the duration of levodopa intake, dyskinesia and family history of PD4. For all patients, the Unified PD Rating Scale (UPDRS) score in off state (without dopaminergic medications) was calculated according to the Movement Disorder Society-UPDRS4. All patients were clinically examined for various striatal and postural deformities (antecollis, camptocormia, Pisa syndrome, scoliosis, striatal hands and striatal foot). Those patients having postural deformities were evaluated by a locally made goniometer for quantitative measurement of deformity. All patients having clinically appreciable deformities underwent radiological evaluation by X-ray. Scoliosis was measured by Cobb angle radiologically. Needle electromyography was done to rule out myopathy in patients having antecollis, camptocormia and Pisa syndrome. Clinical criteria for striatal and postural deformities were taken as described elsewhere256.
Statistical analysis: Pearson's chi-square test and Student's t test were used for univariate analysis and ANOVA test was used for multivariate analysis. Spearman's rank correlation test was used for calculating correlation between variables. All statistical analyses were done on Statistical Package for the Social Sciences, SPSS version 20.0 software (IBM, USA).
Results
A total of 79 patients with a possible diagnosis of PD were included. Out of these, nine patients were excluded from the study as they were diagnosed as having PD-plus syndrome. Of the 70 patients with PD, 47 (67.1%) were male and 23 (32.9%) were females (M : F ratio; 2.04:1). Mean age at presentation was 56.48±11.36 years. Majority of the patients were in the age group of 60-70 yr (37.14%). Mean age of onset of PD symptom was 51.42±12.09 yr, and up to 35.71 per cent patients had PD symptom onset between 51 and 60 years. The mean duration of PD symptoms at presentation was 4.95±4.19 years. Eighteen (25.7%) patients had not received levodopa till the time of presentation. The mean duration of levodopa treatment in the remaining 52 patients was 2.89 yr (range: 20 days to 14 yr).
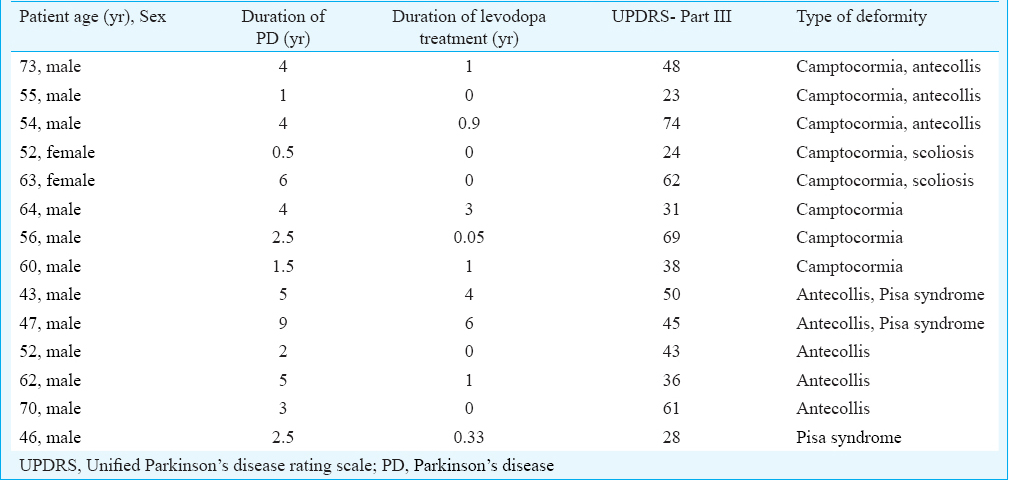
Of the 70 patients with PD, 34 (48.57%) (Tables I-III patients had some degree of postural or striatal or combined deformities. The UPDRS score (total and Part III in off state) and Hoehn and Yahr (H&Y) score were significantly higher (P<0.001) in patients with PD with postural or striatal deformities compared to patients with PD without deformities (Table IV). The durations of PD symptom (5.20±4.72 vs. 4.73±3.69 yr) and levodopa therapy (3.01±3.43 vs. 2.78±3.36 yr) were longer in patients with PD with deformities compared to patients with PD without deformities, but it was not significant. Of the 34 patients, 23 patients had significant deformities (camptocormia ≥45°, antecollis ≥45°, Pisa syndrome ≥10°, scoliosis ≥10°, striatal foot and striatal hand). Patients with PD with significant deformities had significantly higher UPDRS Part III score (P<0.001), total UPDRS score (P<0.001) and H&Y score (P=0.046) compared to patients with PD without significant deformities.
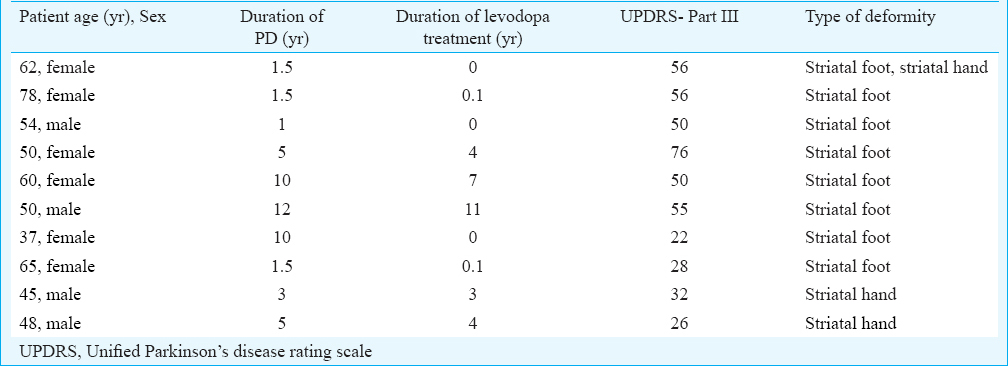

Striatal foot and striatal hand were common deformities observed in patients with PD (Fig. 1), however, striatal foot was most common deformity (n=18). Patients with PD with striatal foot had significantly higher UPDRS III score (P<0.001), total UPDRS score (P<0.001) and H and Y score (P=0.018) compared to patients with PD without striatal foot. Striatal foot was significantly more (P<0.001) among female patients compared to male patients. Among striatal foot deformities, the most common deformity was toe flexion, being present in 94.44 per cent (n=17) patients having striatal foot deformity (Fig. 1 C, D). Five (7.14%) patients had striatal hand deformity and the most common deformity observed was flexion at metacarpophalangeal (MP) joint and extension at interphalangeal (IP) joint (Fig. 1 A, B). Others types of foot deformities were big toe hyperextension in four, equinovarus deformity in three and big toe lateral flexion in two patients.

- Striatal hand showing flexion at metacarpophalangeal joint with extension at interphalangeal joint and ulnar deviation of the left hand (A), which was confirmed by hand X-rays (B), striatal toe showing lateral flexion of the great toe with flexion of other toes (C), which was confirmed by foot X-rays (D).
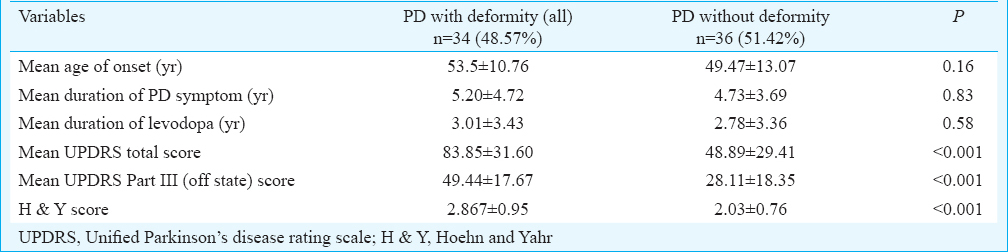
Three patients had Pisa syndrome ≥10° (Fig. 2) and three had scoliosis ≥10° (Fig. 3). Though the duration of PD symptoms, UPDRS score (Part III & total) and H and Y score were greater in patients with Pisa syndrome and patients with scoliosis, the difference was not significant. Scoliosis was significantly more in female patients with PD compared to male patients with PD. Fourteen patients had camptocormia and 13 had antecollis (Figs. 4, 5).

- Pisa syndrome in a patient with Parkinson's disease characterized by leaning towards left side (A), which was confirmed by spine X-rays (B).
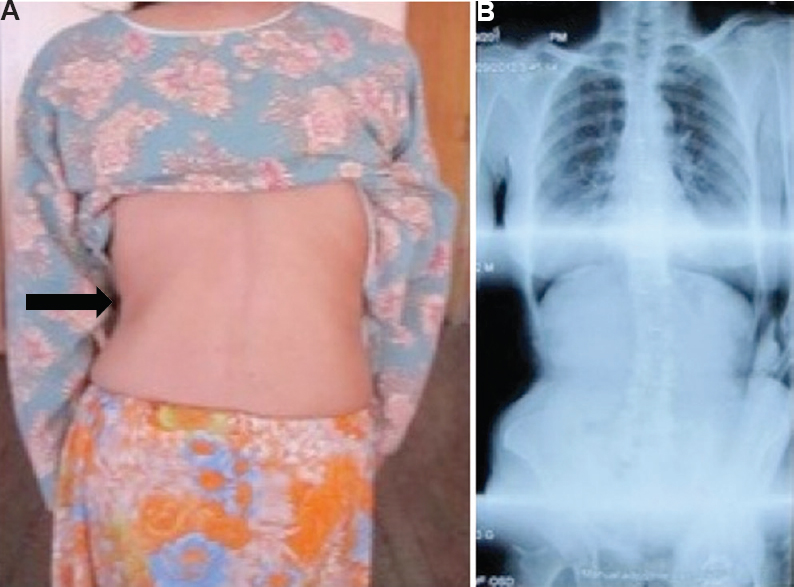
- A patient with Parkinson's disease with scoliosis with concavity towards left side (A), which was confirmed by spine X-rays (B).

- Camptocormia in a patient with Parkinson's disease (A and B), which was corrected by pushing against wall (C) and while lying down (D).

- Antecollis in a patient with Parkinson's disease (A) which was confirmed by cervical spine X-rays (B) and relieved completely on lying supine (C).
Dyskinesias were present in 12 (17.1%) patients. Dyskinesia was significantly more in patients with PD who had longer duration of levodopa intake (P<0.001) and patients with longer duration of PD symptoms (P=0.005). Patients with dyskinesia did not show significant difference in UPDRS and H and Y scores compared with patients without dyskinesia.
Striatal foot and striatal hand were present on ipsilateral side of the PD symptom in relation to initial symptom onset in 94.44 (17/ 18) and 80 (4/ 5) per cent, respectively. Pisa syndrome and concavity of scoliosis were on contralateral side to PD symptom onset side in 66.67 per cent each (2/ 3) (Table V).
Discussion
In our study, striatal foot was the most common deformity observed, followed by camptocormia in patients with PD. Various striatal and postural deformities have been described among PD and PD plus patients. In a study by Ashour and Jankovic1, these deformities were present in 33.5 per cent of patients with PD. Among these deformities, the most common was striatal limb deformity (12.8%) and camptocormia. In our study, patients with significant deformities also had significantly higher UPDRS III, total UPDRS, and H and Y scores suggestive of more likelihood of deformities in more advanced PD. Patients with postural or striatal deformities did not have significant difference in the age of onset of PD symptoms, duration of PD symptoms, duration of levodopa intake and family history of PD/tremor compared to patients without deformities.
Ashour and Jankovic1 described the characteristics of striatal foot deformity as great toe extension or flexion, planter flexion of remaining toe and equinovarus foot (ankle inversion). The relative frequency of various components of striatal foot may indicate the severity of striatal foot deformity. Big toe lateral flexion and equinovarus foot may indicate severe form of striatal foot deformity. Jankovic and Tintner7 found striatal hand and foot deformities in up to 10 per cent of untreated patients with advanced PD. In another study foot dystonia was found to develop in 20-40 per cent of the patients with PD receiving sustained levodopa treatment8.
Ashour and Jankovic1 found that patients with striatal deformity were younger and had earlier disease onset than patients without deformity. Gortvai9 suggested that MP flexion and IP extension, due to contraction of lumbricals and interossei, respectively, could be the earliest signs of striatal hand. In our study, among striatal hand deformities, flexion at MP joint and extension of IP joint were most common. Spagnolo et al10 concluded that striatal hand was significantly worse on the side of PD onset and on the side having more PD symptoms.
In our study, camptocormia was present in 20 per cent patients and they had higher UPDRS and H and Y scores compared to patients without camptocormia. Camptocormia has been reported to be present in 3- 7 per cent patients with PD1112. Camptocormia has been found to be associated with severe disease (high UPDRS score and H&Y score) and longer duration of levodopa therapy1112. Abe et al13 reported camptocormia in 17.64 per cent patients and there was no significant difference in age, duration, severity and drug dose between patients with and without camptocormia. In a recent review, authors have classified camptocormia as upper and lower types and reported its prevalence in patients with PD ranging from 3 to 18 per cent3.
Antecollis was seen in 7.14 per cent patients in our study, as was also reported earlier1. In a study by Kashihara et al6, dropped head syndrome was found in six per cent patients. Fujimoto14 found that seven of the 131 (5.3%) patients with PD had dropped head.
In our study, Pisa syndrome was found in five (7.14%) patients with PD. Bonanni et al15 found 26/1400 (1.9%) patients presenting with lateral flexion of the trunk (≥15°). Tassorelli et al16 found Pisa syndrome in 20 (6.67%) patients out of 300 patients with PD. Age, disease duration, gender, UPDRS III score, and H and Y score among patients with Pisa and without Pisa syndrome were almost equal and did not show any significant difference. Doherty et al17 analyzed 15 patients with PD having Pisa syndrome and found that the angle of scoliosis/Pisa improved up to 44 per cent while patients moved from standing to supine position.
In our study, scoliosis was present in five of 70 patients with PD, of whom three had significant scoliosis (≥10°). Ashour and Jankovic1 found scoliosis in 8.5 per cent patients with PD. Baik et al18 found scoliosis (≥10°) in 32 of the 97 patients with PD (32.98%) and it was observed more frequently in women than in men (P=0.006).
Duvoisin and Marsden19 analyzed 19 patients of PD with scoliosis and found that 16 of them had scoliosis concavity towards contralateral side to the initial parkinsonian symptomatology and three towards ipsilateral side. There has been debate about the direction of trunk leaning (Pisa syndrome or scoliosis) towards or away from predominant parkinsonian symptom side6. Ashour and Jankovic1 found that side of striatal deformity correlated with the side of initial parkinsonian symptom in all patients with striatal hand and in 83.3 per cent of patients with striatal foot. Baik et al18 found no correlation between PD symptom laterality and scoliosis. The number of patients having Pisa syndrome and scoliosis was less in our study, so proper assessment regarding their sidedness could not be done.
In conclusion, our study showed that striatal and postural deformities were common in Indian patients with PD. These were more frequent in advanced stage of disease as reflected by significantly higher UPDRS, and H and Y scores in these patients. Striatal foot and striatal hand were more likely to be ipsilateral to the side of PD symptom onset.
Conflicts of Interest: None.
References
- Joint and skeletal deformities in Parkinson's disease, multiple system atrophy, and progressive supranuclear palsy. Mov Disord. 2006;21:1856-63.
- [Google Scholar]
- Striatal deformities of the hand and foot in Parkinson's disease. Lancet Neurol. 2005;4:423-31.
- [Google Scholar]
- Camptocormia in Parkinson's disease: definition, epidemiology, pathogenesis and treatment modalities. J Neurol Neurosurg Psychiatry. 2016;87:75-85.
- [Google Scholar]
- Parkinson's disease: clinical features and diagnosis. J Neurol Neurosurg Psychiatry. 2008;79:368-76.
- [Google Scholar]
- The pharmacology of foot dystonia in Parkinsonism. Clin Neuropharmacol. 1987;10:47-56.
- [Google Scholar]
- Deformities of the hands and feet in Parkinsonism and their reversibility by operation. J Neurol Neurosurg Psychiatry. 1963;26:33-6.
- [Google Scholar]
- Striatal hand in Parkinson's disease: the re-evaluation of an old clinical sign. J Neurol. 2014;261:117-20.
- [Google Scholar]
- A specific clinical pattern of camptocormia in Parkinson's disease. J Neurol Neurosurg Psychiatry. 2006;77:1229-34.
- [Google Scholar]
- Camptocormia in Parkinson disease: an epidemiological and clinical study. J Neurol Neurosurg Psychiatry. 2009;80:145-8.
- [Google Scholar]
- Botulinum toxin treatment of lateral axial dystonia in Parkinsonism. Mov Disord. 2007;22:2097-103.
- [Google Scholar]
- Pisa syndrome in Parkinson's disease: clinical, electromyographic, and radiological characterization. Mov Disord. 2012;27:227-35.
- [Google Scholar]
- Pisa syndrome in Parkinson's disease: a mobile or fixed deformity? J Neurol Neurosurg Psychiatry. 2013;84:1400-3.
- [Google Scholar]
- Note on the scoliosis of Parkinsonism. J Neurol Neurosurg Psychiatry. 1975;38:787-93.
- [Google Scholar]






