Translate this page into:
Are childhood externalizing disorders the harbinger of early-onset alcohol dependence?
Reprint requests: Dr Savita Malhotra, House No. 461, Sector 37A, Chandigarh 160 036, India e-mail: savita.pgi@gmail.com
-
Received: ,
This is an open access article distributed under the terms of the Creative Commons Attribution NonCommercial ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non commercially, as long as the author is credited and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Background & objectives:
The subtyping of alcohol dependence (AD) into early-onset (EO) and late-onset (LO) subgroups has been shown to have clinical and biological validity. As externalizing disorders (EDs) predate AD, the link of ED with age of onset of alcohol dependence needs to be investigated. The aim of this study was to examine the relationship of EDs such as disruptive behaviour disorder (DBD) and attention deficit hyperactivity disorder (ADHD) with age at onset of AD in a sample of male subjects.
Methods:
One hundred consecutive male subjects with AD presenting to the De-Addiction Services and an equal number of biologically unrelated non-substance-dependent control subjects were included in the study. The AD subjects were divided into EO (age of onset of AD ≤25 yr; n = 21) and LO (age of onset of AD >25 yr; n = 79). Subjects were examined for evidence of DBD and ADHD in childhood, and current ADHD using structured instruments such as Semi-Structured Assessment for the Genetic of Alcoholism-IV (SSAGA-IV) and Kiddie – SADS – Present and Lifetime Version (K-SADS-PL). The odds ratio of association of EDs with EO and LO AD was calculated by comparing these subgroups with the biologically unrelated control group. Later, both the subgroups of alcohol dependence were compared for the presence of EDs.
Results:
All EDs (DBDs/childhood or adult ADHD) were more common in AD individuals as compared to the controls. However, when AD subgroups were compared with controls, the association of DBDs and ADHD reached a significant level only in the EO subgroup. A comparison of EO and LO AD showed that more EO individuals had history of both childhood disruptive disorder and ADHD compared to LO subgroup. Adult ADHD was also over-represented in EO subgroup.
Interpretation & conclusions:
Our study showed more EDs in alcohol dependent individuals compared to controls. Further, the association observed between EDs and EO alcohol dependence points towards a developmental continuum between these two conditions.
Keywords
Alcohol dependence
attention deficit hyperactivity disorder
early onset
externalizing disorders
Alcohol dependence is a complex and heterogeneous disease in clinical medicine. Social, psychological and biological factors influencing the aetiogenesis of alcohol dependence are manifold. There are generally two accepted basic phenotypes of alcohol-dependent individuals, defined as low severity/vulnerability subgroup and high severity/vulnerability subgroup1. The first one is characterized by a later onset of problem drinking, less severe alcohol dependence and alcohol-related problems. The latter is characterized by an early onset (EO) of problem drinking, family history of alcohol dependence problems, antecedents of psychopathology and severe alcohol dependence and alcohol-related problems.
Oppositional defiant disorder (ODD), conduct disorder (CD) and attention deficit hyperactive disorder (ADHD) are grouped together as externalizing disorder (ED) of childhood2. The link between CD and drug use and abuse has been confirmed345. Evidence is presented cross-sectionally34 and prospectively, for CD as a strong predictor of the use and abuse of alcohol5. Interestingly, the younger the sample, the stronger the prediction from CD to substance use disorder (SUD)6. Disruptive behaviour disorders (DBDs) appear to be among the most common co-morbid conditions in adolescents afflicted with an SUD7891011. In a meta-analysis on the association of ADHD and alcohol dependence, a positive association was demonstrated12. However, the authors have also commented that ‘Given the substantial co-morbidity between ADHD and DBD, including ODD and CD, as well as the robust relations between ODD/CD and substance outcomes the conclusions suggested from this meta-analysis must be interpreted cautiously12. In their extensive review in this area, Flory and Lynam13 have commented on the significant degree of overlap between CD and ADHD which eventually leads to a limited role of ADHD as a predictor of substance dependence. Therefore, the association of CD with alcohol dependence is almost unequivocal and research evidence indicates a possible association with adolescence SUDs. The offshoot of National Comorbidity Survey Replication (NCSR) has reported the co-morbidity of alcohol and drug dependence with adult ADHD as 5.8 and 4 per cent, respectively14. Are these associations relevant to alcohol dependence in general? Or is there a subgroup to which these associations are more applicable, is the question which is still not answered convincingly. Age of onset of alcohol dependence could be the most appropriate parameter to stratify the patients into well-defined subgroups.
The only study available from the southern part of India showed a positive association between EO alcohol dependence and ADHD both in the childhood and in adults15. However, in this study the Diagnostic and Statistical Manual of Mental Disorders-III (DSM-III) compatible diagnostic instruments were used and it was conducted on a relatively smaller sample, did not examine other EDs and, most importantly, did not have any control group. In an earlier study from northern India personality characteristics were studied in relation to the age of onset of alcohol dependence16. Personality characteristics such as sensation seeking, guilt proneness though are relevant for research and understanding the underlying construct, but are not practically applicable and clinically meaningful as per as current nosology. Therefore, this study was undertaken to investigate whether childhood EDs which are otherwise closely associated with alcohol dependence, had a differential occurrence in the EO and LO alcohol-dependent males.
Material & Methods
The study consisted of subjects recruited from the patient population attending the outpatient and the inpatient services of the Drug De-addiction and Treatment Centre of Postgraduate Institute of Medical Education and Research, a tertiary care institute in Chandigarh, India. One hundred male individuals with AD were included in this study over a period of eight months (May to December, 2010). One hundred male attendants accompanying AD subjects, hailing from similar socio-economic background and who had never (or only occasionally) used any substance in their lifetime, were included as controls. The controls were neither biologically related nor were the spouse of the subjects. They were other male persons accompanying the AD subject, such as their neighbours, their colleagues or someone from their wife's family. Ethical clearance for the study protocol was obtained from the Institutional Ethics Committee.
Inclusion and exclusion criteria for study subjects: The inclusion criteria included the following: (i)Fulfilling the International Classification of Diseases-10 (ICD-10)/DSM-IV criteria1718 of alcohol dependence past/present; and (ii) Age 20-50 yr.
Those (i) having childhood psychotic illness; (ii) were dependent/used substance other than alcohol; (iii) had history suggestive of mental retardation; and (iv) any organic disease – visual, hearing problem, pervasive development disorders and seizure disorder, were excluded.
Inclusion and exclusion criteria for the control: Those male subjects aged 20-50 yr not fulfilling ICD-10/DSM-IV criteria for any substance dependence were included as controls. Those who were biologically related to the cases, and those not willing to participate in the study, were excluded.
Assessment: The following instruments were applied for the study purpose. The socio-demographic profile was collected from all participants using the proforma developed for this purpose. The Semi-Structured Assessment for the Genetic of Alcoholism (SSAGA- IV)19, which was designed to assess the physical, psychological and social manifestations of alcohol abuse or dependence and other psychiatric disorders, was used to assess alcohol dependence. This same instrument was also applied to diagnose CD and ODD in the study subjects during their childhood. Another instrument, the Kiddie-SADS-Present and Lifetime Version (K-SADS-PL, Version 2.1 of October 1996)20, which is a semi-structured diagnostic interview designed to assess current and past episodes of psychopathology according to DSM-IV criteria, was used to diagnose childhood ADHD retrospectively. For the assessment of adult ADHD, continuation of childhood ADHD symptoms into adulthood was considered. Whenever feasible, information obtained from the subject was clarified by interviewing their parents.
The study subjects were grouped as EO and LO by the age-of-onset criterion (i.e., subjects with onset of DSM-IV TR/ICD-10 positive alcohol dependence after the age of 25 yr were categorized as ‘LO’; those with age at onset of alcohol dependence less than or up to 25 yr were categorized as ‘EO’)16. Two hundred consecutive male subjects, fulfilling all the intake criteria, were recruited for the study. Informed written consent was obtained from each of them, after explaining the non-invasive nature of the study and assuring them of anonymity and confidentiality.
A cross-sectional examination was completed by applying SSAGA-IV scale to reconfirm the diagnosis of alcohol dependence, to find out alcohol-related social, legal, physical and psychological complications and to measure certain severity-related clinical variables such as age of the first drink or time latency between the first alcohol use and dependence. SSAGA-IV alcohol section was not administered in the control group. The same instrument was also applied in both the AD subjects and controls to diagnose childhood disruptive disorders (CD/ODD) in the past. Childhood and adulthood ADHD was diagnosed by K-SADS-PL scale.
Statistical analysis: The data generated were subjected to statistical analysis (Chi-square test with or without Yates’ correction for the frequency categories and Student's unpaired t test for the parametric variables). The objective was to see whether the socio-demographic, severity of alcohol dependence-related clinical variable and childhood or adult psychopathology were significantly different in the two groups of alcohol-dependent subjects.
Results
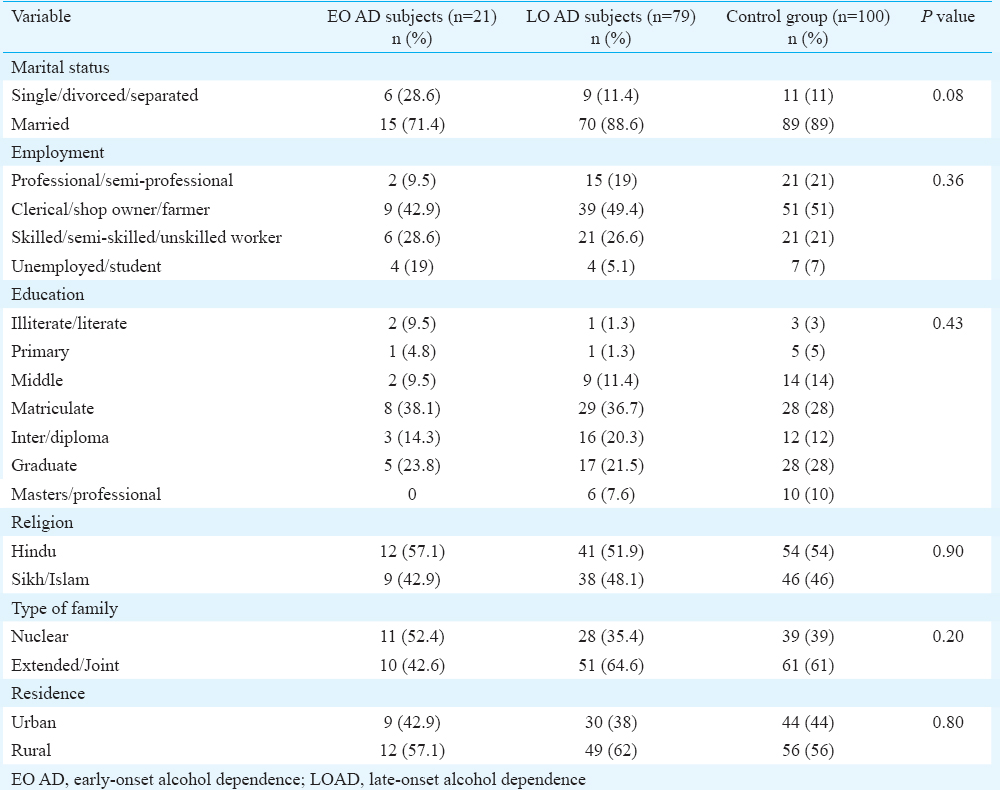
Among the 100 alcohol-dependent males, 21 were EO and 79 were LO cases. The age of EO cases ranged from 26 to 49 yr (mean = 35.5 ± 7.3 yr) and that of the LO subgroup was 28-49 yr (mean = 40.2 ± 6.6 yr). The difference was significant (P < 0.01) indicating that EO subjects sought treatment at a lower age. With respect to the socio-demographic profile, all three groups, i.e., the EO, LO and control were comparable regarding marital status, education, occupation, residence, religion and type of family (Table I).
Comparison of the two subgroups of AD cases showed that EO had significantly more (P < 0.001) number of alcohol-related complications as compared to the LO subgroup. Alcohol-related complications consisted of legal, social, physical and psychological adversities originating due to alcohol intake and were measured by SSAGA-IV. A total score combining all these complications was used in the analysis. Moreover, the individuals in the EO subgroup had their first drink at a significantly earlier age (P < 0.001) as compared to the LO subgroup. The time latency required to become dependent to alcohol after initial alcohol use was observed to be significantly less (P < 0.05) in the EO subgroup.
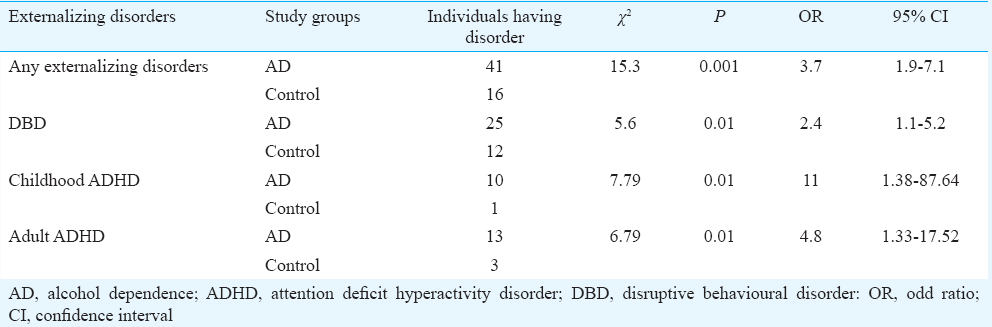
Table II shows a comparison between the AD subjects and biologically unrelated controls. Any ED was significantly more [P = 0.001, odds ratio (OR) = 3.7] in the alcohol-dependent group as compared to the controls. Likewise, DBDs (P = 0.01, OR = 2.4) and childhood ADHD (P = 0.01, OR = 11) were observed to be significantly associated with alcohol dependence. The co-occurrence of adult ADHD (P = 0.01, OR = 4.8) was more in the AD group.
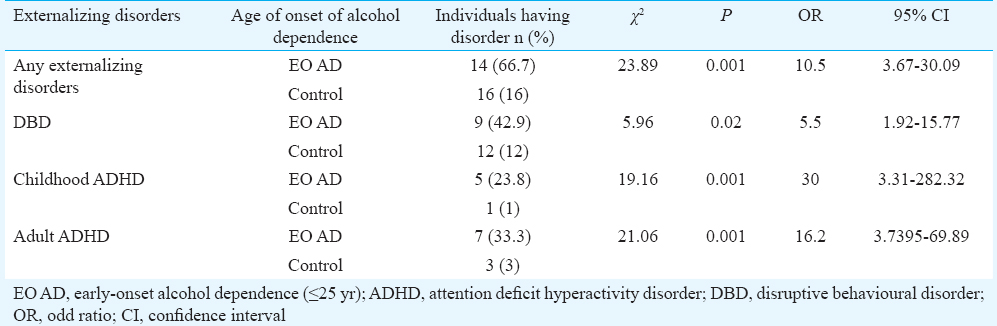
In Table III, the comparison of EO AD with the control group was made. Any ED more often predated EO AD as compared to the controls. EO AD was significantly associated with DBDs (P = 0.02, OR = 5.5), childhood (P = 0.001, OR = 30) and adult ADHD (P = 0.001, OR = 16.2).
Comparison of LO AD with the control group was also done. Although any ED (P = 0.004, OR = 2.7) was significantly associated with LO AD, the occurrence of DBDs (P = 0.15), ADHD either in childhood (P = 0.08) or in the adults (P = 0.18) was equally common in both the groups (Table IV).

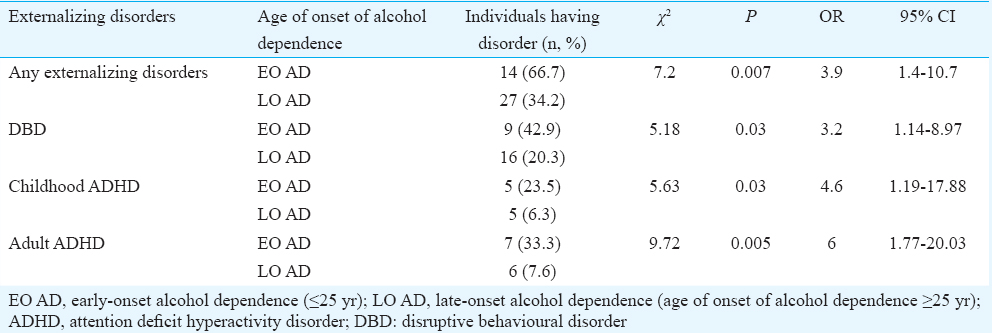
Table V demonstrates a comparison between the two subgroups of alcohol-dependent individuals with respect to the presence of psychopathology mostly in the childhood but also in the adults. Childhood EDs which include ADHD and childhood disruptive disorders (conduct and ODD) were present in 14 EO and 27 LO AD cases. Their comparison showed significantly higher (P < 0.05) positivity of EDs in EO subgroup. Nine and 16 of EO and LO AD cases were found to have childhood disruptive disorders, respectively. The difference was significant (P < 0.05). Five subjects from each subgroup were found to have ADHD in childhood. EO cases were found to be significantly more (P < 0.05) likely to be suffering from ADHD in childhood as compared to the LO subgroup. The adult ADHD was co-morbid with seven EO and six LO AD individuals. The EO subgroup was observed to have significantly higher (P < 0.01) co-morbidity with adult ADHD.
Discussion
In our study, alcohol-dependent individuals were classified into two groups based on their age of onset of dependence. The cut-off age used for designating EO and LO alcohol dependence was 25 yr, as has been done in an earlier study by Varma et al16. In 1988, Parrella and Filstead21 reported the existence of a developmental sequence for onset and progress of alcohol dependence and concluded that no definition about EO and LO was more right than the others and accepted 25 years as a reasonable cut-off. The EO subgroup had a significantly earlier age of first drink and took lesser time to become dependent to alcohol as compared to the LO group. Further, the EO subjects encountered significantly higher number of complications. Hence EO is a more severe subgroup which is concordant with the available literature from the world22 and India16.
AD was observed to have a significant association with all EDs (DBD/ADHD). However, analysis of the subgroups of alcohol dependence showed that it was the EO AD which was significantly predated by EDs. When EDs were further classified as childhood ADHD or DBDs, both of them were found to be significant antecedents of the subgroups with an EO of alcohol dependence. The study of concurrent adult ADHD also had findings on the similar lines. Adult ADHD showed the strongest association with the EO group. In fact, this association may be even stronger than that for other disorders such DBDs, going by the strength of associations as reflected in the odds ratios.
Another interesting finding was that when the overall sample was considered, the co-morbidity among the childhood disorders was less than expected. However, in the EO AD subgroup, the rate of co-morbidity was high. This concurrence of EO AD, DBD and ADHD alludes to the concept of EDs and substantiates EO AD (but not LO AD) as a part of externalizing spectrum.
The early age of onset was shown to be associated with aggression, problems with law23; social role maladaptation, loss of behavioural control when drinking24 and childhood criminality25. Varma et al16 found that individuals with EO AD were higher sensation seekers and tended to display aggression, violence and general disinhibition when drinking. The close link between a few childhood disorders and a subgroup of alcohol dependence demonstrated in the present study supports the notion of a common underlying genetic and temperamental vulnerability. There is strong evidence of a disturbance in brain serotonergic transmission among anti-social, impulsive and violent EO alcoholic subjects. Serotonin transporter ‘S’ promoter polymorphism has been shown to be associated with an increased risk for EO alcohol dependence and is also associated with anti-social personality disorder and impulsive, habitually violent behaviour26. In addition to the serotonergic system, dopaminergic neurotransmission is also found to be involved. DRD2 gene is associated with susceptibility to EO alcohol dependence27. The same system also has been implicated in the aetiopathogenesis of ADHD. Not only genetic, but there has also been a substantial neurobiological overlap between EDs and EO alcohol dependence. Deficits in prefrontal cortex (PFC)-mediated executive functions of decision-making, sustained attention, verbal fluency abstraction, behavioural inhibition, working memory, regulation of motivation and motor control are seen in ADHD2829 and CD30. Delayed PFC maturation (less myelination of the PFC) may be an inherent vulnerability that enhances the risk for EO alcohol dependence31. The EO individuals might represent the same spectrum as the EDs.
Clinical and psychological characterization of EO alcoholic subtypes could be addressed to provide a more accurate research evidence for pharmacologically and/or psychologically tailored treatments. Benegal et al32 demonstrated a direct treatment implication. Their results showed that treatment with atomoxetine was not only effective in controlling externalizing symptoms but also could increase the period of abstinence, quality of life and shorter duration of relapse. It would be interesting to study if this beneficial effect is more pronounced in EO subjects.
In this study, the sample was drawn from individuals attending a de-addiction clinic for treatment rather than from alcohol-dependent subjects from the community. In general, complicated and severe alcohol dependence is dealt within a clinic setting. Thus the extent, to which the findings of this study may be generalized, is limited to the clinic attending, treatment-seeking individuals of the entire alcohol-dependent population. Moreover, in our study the number of adult ADHD cases was more than the childhood ADHD cases. Hence, this also could have some effect in the generalizability of the results. The basis of determination of the presence of ADHD/CD/ODD (other than adult ADHD) was essentially and necessarily retrospective in nature. Hence, factors such as recall bias, selective forgetting and retrospective falsification cannot be ruled out. To minimize the effect of these factors information put forth by the individuals was corroborated from the available informants whenever feasible. In this study the investigator was not blind to the outcome. Hence, the possibility of ascertainment bias could not be ruled out. The onset of alcohol dependence was determined later after examining the life chart as per SSAGA and that was done after the individuals were interviewed for the presence of EDs. Hence, the interviewer was not aware of their onset of AD status during the time of assessment for the exposure (presence of EDs). This must have reduced the interviewer's bias. Furthermore, in our study, we did not examine the effect of other risk factors for the development of alcohol dependence such as peer acceptance, academic achievement, maternal alcohol use and maternal hostility using a multivariate model. Along with EDs, these factors could have influenced the developmental trajectory of alcohol dependence.
In conclusion, our results indicate a developmental trajectory which starts from the childhood EDs and culminates in EO alcohol dependence. Our findings demonstrate this concept in an Indian setting, supporting the growing literature in this area from other countries. The study also provides an impetus for the future researchers to explore the entity of EO alcohol dependence more systematically and extensively. The association of EO alcohol dependence with various EDs is expected to create a window of opportunity to reveal the underlying genetic and neurobiological vulnerability of these disorders.
Conflicts of Interest: None.
References
- Age of onset as a discriminator between alcoholic subtypes in a treatment-seeking outpatient population. Am J Addict. 2000;9:17-27.
- [Google Scholar]
- Review of the evidence base for treatment of childhood psychopathology: Externalizing disorders. J Consult Clin Psychol. 2002;70:1267-71.
- [Google Scholar]
- A comparison of the symptoms associated with early and late onset alcohol dependence. J Nerv Ment Dis. 1997;185:507-9.
- [Google Scholar]
- Comorbidity of substance use disorders and other psychiatric disorders among adolescents: evidence from an epidemiologic survey. Drug Alcohol Depend. 2007;88(Suppl 1):S4-13.
- [Google Scholar]
- Development of psychiatric comorbidity with substance abuse in adolescents: effects of timing and sex. J Clin Child Psychol. 1999;28:298-311.
- [Google Scholar]
- Psychiatric predictors of adolescent and young adult drug use and abuse: what have we learned? Drug Alcohol Depend. 2007;88(Suppl 1):S97-9.
- [Google Scholar]
- Conduct disorder, substance use disorders, and coexisting conduct and substance use disorders in adolescent inpatients. Am J Psychiatry. 1996;153:914-20.
- [Google Scholar]
- An epidemiological study of disorders in late childhood and adolescence – I. Age- and gender-specific prevalence. J Child Psychol Psychiatry. 1993;34:851-67.
- [Google Scholar]
- Comorbidity of substance abuse and other psychiatric disorders in adolescents. Am J Psychiatry. 1989;146:1131-41.
- [Google Scholar]
- Conduct disorder among adolescent alcohol and drug abusers. J Stud Alcohol. 1996;57:314-24.
- [Google Scholar]
- Psychopathology in preadolescent sons of fathers with substance use disorders. J Am Acad Child Adolesc Psychiatry. 1997;36:495-502.
- [Google Scholar]
- Prospective association of childhood attention-deficit/hyperactivity disorder (ADHD) and substance use and abuse/dependence: a meta-analytic review. Clin Psychol Rev. 2011;31:328-41.
- [Google Scholar]
- The relation between attention deficit hyperactivity disorder and substance abuse: what role does conduct disorder play? Clin Child Fam Psychol Rev. 2003;6:1-16.
- [Google Scholar]
- The prevalence and correlates of adult ADHD in the United States: results from the National Comorbidity Survey Replication. Am J Psychiatry. 2006;163:716-23.
- [Google Scholar]
- The association between attention-deficit/hyperactivity disorder and early-onset alcohol dependence: a retrospective study. Indian J Psychiatry. 2008;50:262-5.
- [Google Scholar]
- Correlates of early- and late-onset alcohol dependence. Addict Behav. 1994;19:609-19.
- [Google Scholar]
- The ICD-10 classification of mental and behavioural disorders: clinical descriptions and diagnostic guidelines. Geneva: World Health Organization; 1992.
- Diagnostic and statistical manual of mental disorders: DSMIV-TR. Washington, DC: American Psychiatric Association; 2000.
- A validity study of the SSAGA – A comparison with the SCAN. Addiction. 1999;94:1361-70.
- [Google Scholar]
- Schedule for affective disorders and schizophrenia for school-age children-present and lifetime version (K-SADS-PL): initial reliability and validity data. J Am Acad Child Adolesc Psychiatry. 1997;36:980-8.
- [Google Scholar]
- Definition of onset in the development of onset-based alcoholism typologies. J Stud Alcohol. 1988;49:85-92.
- [Google Scholar]
- Types of alcoholics, I. Evidence for an empirically derived typology based on indicators of vulnerability and severity. Arch Gen Psychiatry. 1992;49:599-608.
- [Google Scholar]
- Platelet MAO activity as a biological marker in subgroups of alcoholism. Acta Psychiatr Scand. 1985;72:51-8.
- [Google Scholar]
- Age of onset versus duration of problem drinking on the Alcohol Use Inventory. J Stud Alcohol. 1985;46:398-402.
- [Google Scholar]
- Clinical importance of age at onset in type 1 and type 2 primary alcoholics. Arch Gen Psychiatry. 1990;47:320-4.
- [Google Scholar]
- Association between low activity serotonin transporter promoter genotype and early onset alcoholism with habitual impulsive violent behavior. Mol Psychiatry. 1999;4:385-8.
- [Google Scholar]
- Association between early-onset alcoholism and the dopamine D2 receptor gene. Am J Med Genet. 1997;74:179-82.
- [Google Scholar]
- Behavioral inhibition, sustained attention, and executive functions: constructing a unifying theory of ADHD. Psychol Bull. 1997;121:65-94.
- [Google Scholar]
- Neural substrates of decision making in adults with attention deficit hyperactivity disorder. Am J Psychiatry. 2003;160:1061-70.
- [Google Scholar]
- Neuropsychological characteristics of adolescents with conduct disorder: association with attention-deficit-hyperactivity and aggression. J Abnorm Child Psychol. 1999;27:225-36.
- [Google Scholar]
- A.E. Bennett Research Award. Developmental traumatology. Part II: brain development. Biol Psychiatry. 1999;45:1271-84.
- [Google Scholar]
- The efficacy of atomoxetine as adjunctive treatment for co-morbid substance use disorders and externalizing symptoms. Asian J Psychiatr. 2013;6:544-7.
- [Google Scholar]






