Translate this page into:
Antipsychotic treatment, psychoeducation & regular follow up as a public health strategy for schizophrenia: Results from a prospective study
Reprint requests: Dr. Channaveerachari Naveen Kumar, Department of Psychiatry, National Institute of Mental Health & Neurosciences, Hosur Road, Bengaluru 560 029, Karnataka, India e-mail: cnkumar1974@gmail.com
-
Received: ,
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Background & objectives:
In low- and middle-income countries such as India, a feasible public health strategy could be to ensure continuous antipsychotics and psychoeducation for those with schizophrenia. Whether such a strategy favourably influences its course and outcome is not well-studied. The objectives of this study were to examine these issues in a cohort of patients with schizophrenia in a rural south Indian taluk (an administrative block). This cohort was part of a community intervention programme running in the place since the past one decade.
Methods:
A total of 201 patients were assessed after an average of four years of follow up. Psychopathology, disability and course of illness were assessed using Positive and Negative Syndrome Scale (PANSS), Indian Disability Evaluation and Assessment Scale (IDEAS) and Psychiatric and Personal History Schedule (PPHS), respectively. Interventions included ensuring continuous antipsychotic treatment and low-intensity psychoeducation.
Results:
One hundred and forty two [70.6%; 95% confidence interval (CI): 64.35-76.95] of the 201 patients achieved clinical remission by the end of follow up period (four years); 140 (69.6%; 95% CI: 63.29-76.07) had satisfactory outcome (42.3% best outcome and 27.4% intermediate outcome). There was a significant reduction in the proportion of patients with disability [134/201 (66.7%) at baseline; 55/201 (27.3%) at follow up; P< 0.01]. Best course pattern and least disability were seen in patients with best treatment adherence.
Interpretation & conclusions:
Treatment with antipsychotics and psychoeducation can favourably influence the course of schizophrenia and reduce disability in a substantial proportion of patients. Structured psychosocial interventions may be indicated in the significant minority who show suboptimal outcome with this strategy.
Keywords
Antipsychotics
course
disability
outcome
rural community
schizophrenia
Schizophrenia is a severely disabling disorder1. Antipsychotics are effective for acute phase and relapse prevention23. However, their role in influencing the long-term illness course and reducing disability has been questioned4. Most guidelines emphasize on the importance of additional psychosocial therapies, including family therapy, cognitive remediation, social skills training and rehabilitation25. Trained workforce is required to provide such structured psychosocial interventions. In low- and middle-income countries such as India, there is a dearth of clinical psychologists, psychiatric social workers and psychiatric nurses6 who are ideally suited to provide such interventions. On the other hand, since antipsychotic medications form the cornerstone of schizophrenia treatment, a reasonable public health strategy could be to provide antipsychotic medication therapy and basic psychoeducation. Whether such a strategy favourably influences the course and outcome of the disease is not well-studied. This study was undertaken to examine whether this particular strategy had any influence on the long-term course and outcome of schizophrenia including symptom severity and disability in a group of patients in a rural setting in southern India.
Material & Methods
The sample for this study was selected from the ongoing ‘Community Interventions in Psychotic Disorders (CoInPsyD)’ programme in Thirthahalli Taluk (a rural administrative block) of Karnataka State in southern India. Eight Primary Health Centres (PHCs) cater to the health needs of this population. The CoInPsyD programme entails identifying all schizophrenia patients living in the taluk, treating and following them up. Details on patient identification and training ground level staff are described elsewhere7. Research psychiatrists diagnosed the identified patients using International Classification of Diseases-10 (ICD-10) criteria8. They used the Mini International Neuropsychiatric Interview9 to confirm the diagnosis. A total of 332 patients were selected, of them 244 (73.5%) patients completed minimum three years of follow up. Of these 244, 43 patients were excluded for various reasons (Fig. 1). Thus, 201 patients were finally included in this study.
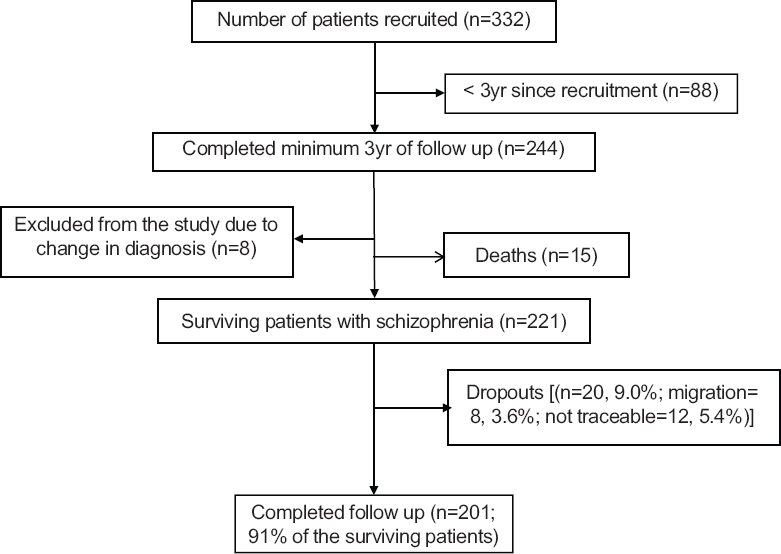
- Flow charts showing follow up status of the patients.
The study was conducted in the department of Psychiatry, National Institute of Mental Health & Neurosciences (NIMHANS), Bengaluru, India in 2011. The study protocol was approved by the ethics committee of NIMHANS and written informed consent was obtained from the patients or family members.
At the time of enrolment, patients and their family members were requested to provide past treatment details. They were offered a choice of receiving treatment either from our research team or from private psychiatrists of their choice. All patients were followed up in their respective PHCs once every two months. Apart from the research data, the following clinical details were recorded during each follow up visit: patients’ symptomatic and functional status, details of the medications, adverse effects, identity of the family members who accompanied them and treatment advice. The diagnosis was verified by clinical interviews at successive follow up visits; patients who had a change of diagnosis were excluded from the study.
Patients were prescribed antipsychotics by the research psychiatrists or their respective private psychiatrists (n=120; 59.7%; n=81; 40.3% respectively). Psychiatrist's role was limited to making diagnosis, medication prescription and psychoeducation. Psychoeducation covered the following aspects: nature of the illness, factors affecting its course, benefits of continued antipsychotic treatment, their adverse effects and the need for keeping patients occupied in meaningful activities (low-intensity psychoeducation). During follow ups, the psychoeducation sessions lasted only for 5-10 min covering the needy areas. The task of ensuring regular follow up was carried out by the research social worker. His tasks involved reminding and arranging follow ups, liaising with taluk health administration for maintaining continuous supply of medications and making home visits for those irregular patients. The structured psychosocial interventions (as mentioned in standard treatment guidelines)25 could not be provided due to non-availability of workforce.
Assessments
Psychopathology: The Positive and Negative Syndrome Scale (PANSS) was used to assess psychopathology10 once in six months by trained raters (psychiatrists). Overall change in scores over the follow up period was assessed using the paired-sample t test. Differences in PANSS scores among different subgroups were assessed using analysis of variance (ANOVA). Different raters administered PANSS during successive follow ups.
Disability: The Indian Disability Evaluation and Assessment scale (IDEAS)11 was used to assess the disability level once in six months. IDEAS had been originally developed for measuring and certifying disability in psychiatric patients in India. It assesses disability across four domains: self-care, interpersonal relationships, communication and understanding and work. Disability is scored from 0 to 4 for each domain (0=no disability; 4=profound disability) and the sum of all the four domain scores gives the total disability score. As in our previous study7, the patients with total IDEAS scores of 7 or more were defined as ‘disabled’. IDEAS has satisfactory psychometric properties12 and has been used in research713. Mc Nemar's test was used to compare change in the categorical variables over time. Repeated measures ANOVA (RMANOVA) was used to assess course of disability among the three different ‘adherence groups’. As with PANSS, different raters administered IDEAS during successive follow ups.
Course: The Psychiatric and Personal History Schedule (PPHS)14 was used to assess the course and outcome. A research psychiatrist reviewed case files for case notes, PANSS and IDEAS scores. Remission was defined according to Andreasen et al15. These criteria require sustained ratings of mild or lower severity (≤3) on all relevant items: (i) For the dimension of reality distortion, the selected PANSS items are P1 (delusions), P3 (hallucinatory behaviour) and G9 (unusual thought content); (ii) For the dimension of disorganization, these are P2 (conceptual disorganization) and G5 (mannerisms/posturing); (iii) For the dimension of negative symptoms, these are N1 (blunted affect), N4 (social withdrawal), and N6 (lack of spontaneity). Relapse was defined as achieving remission at least once followed by an exacerbation of symptoms to the extent of not meeting remission criteria. In the original PPHS, negative symptoms are described as ‘residual personality changes’. In this study, ‘residual personality change’ was defined by scores of 4 or more on any of N1, N4 or N6 of PANSS. Similarly, marked personality change of original PPHS was defined by negative symptoms (as defined above) plus scores of two or more on the ‘work’ item of the IDEAS.
Outcome: Patients were grouped into the following three outcome groups based on an earlier, similar classification16: (i) Best outcome - patients with complete or near complete remission without relapse or exacerbations (Course A, Fig. 2); (ii) Intermediate outcome - patients with no relapses or exacerbations but with residual personality changes, those with one or more relapses or exacerbations with residual personality changes and those with one or more relapses or exacerbations but with full or near full remissions (Courses B, C, D, Fig. 2); and (iii) Worst outcome - patients with continuous psychosis and those with one or more relapses along with marked personality changes (Courses E, F, Fig. 2). Frequency analysis was used to count patients belonging to these different ‘course’ categories.

- Patterns of the courses.
Medication adherence: Patients were divided into the following three groups based on the pattern of adherence to antipsychotic medications17: (i) those who were adherent for more than 75 per cent of the follow up period (best-adherence group); (ii) those who were adherent between 50 and 75 per cent of the follow up period (moderate-adherence group); and (iii) those who were adherent for less than 50 per cent of the follow up period (worst-adherence group). Adherence was assessed based on patient reporting corroborated invariably by family members. The average follow up duration of these 201 patients was 47 months.
Statistical analysis: Percentages and median with interquartile ranges were used for descriptive analysis. Wilcoxon's sign rank test was used to measure the pre-post differences among continuous variables (psychopathology and disability scores). Chi-square test was used to measure the differences among discrete variables. Mc-Nemar test was used to measure the pre-post differences of discrete variables. Non-parametric tests were employed as standard deviation values were noted to be high at some places. Repeated measures (RM) ANOVA was used to assess the course of disability.
Results
Baseline characteristics of the patients are shown in Table I. The patients had median illness duration of 10 yr. One hundred and four (52%) of them were on treatment; of the remaining 97, 45 (22.2%) received antipsychotic medications sometime in the past but were not on any medications at the time of recruitment. Fifty two (25.8%) patients never received any medications for their psychotic illnesses.
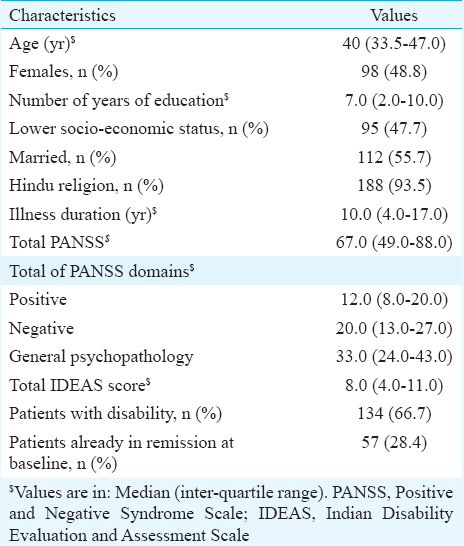
Table II shows the status at final follow up. Most patients received either risperidone (dose range: 2-8 mg/day) or olanzapine (dose range: 5-20 mg/day). Dose adjustment was done as per the patients’ needs. Only 11 patients were on two antipsychotics simultaneously. Nearly, three-fourth of the patients were adherent to medications. There was a significant reduction in psychopathology [Median (interquartile range) PANSS total score=67.0 (49.0-88.0) at the baseline and 42.0 (35.0-56.0) at follow up; P<0.01] and disability level [baseline IDEAS total score=8.0 (4.0-11.0) & 3.0 (0-7.0) at follow up; P≤0.01]. About, 71 per cent (n=142) of the patients were in clinical remission; 83 per cent (n=167) had achieved remission at least once during the follow up period. About 42 per cent (n=85) had the best outcome (Course A); 27.4 per cent (n=55) had intermediate outcome (Courses B, C, D) and 30.3 per cent (n=61) had the worst outcome (Courses E and F; Fig. 2). Overall, 70 per cent (n=140) (95% confidence interval=63.29-76.07) had satisfactory (best or intermediate) outcome.
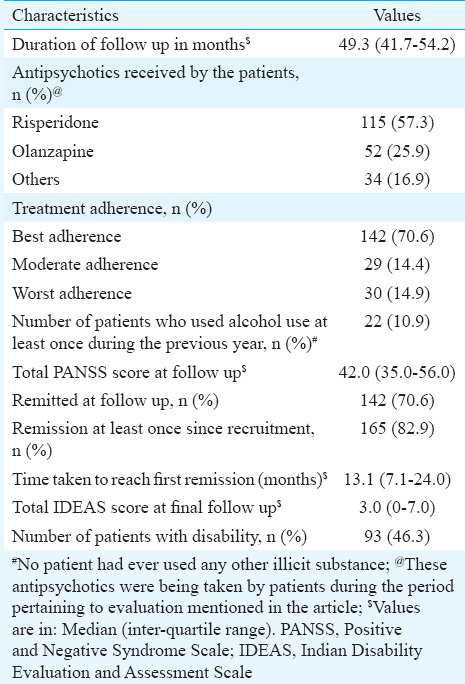
Table III shows the comparison of the three patterns of course and outcomes. Being adherent to treatment, having lesser disability and having shorter duration of illness were associated with more favourable course.
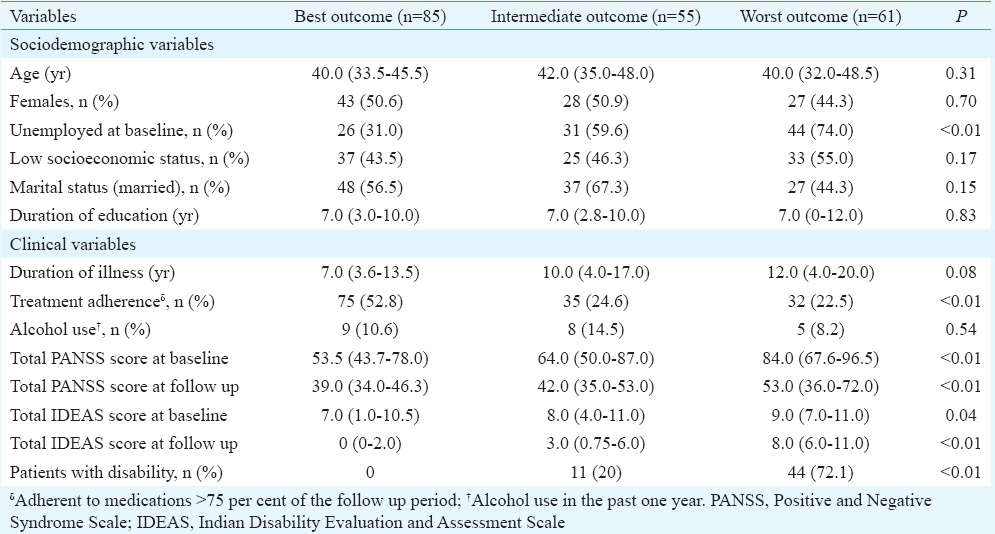
Table IV shows the effect of medication adherence on outcomes. At baseline, best adherence group had significantly lesser severity of symptoms and comparable disability with the other two adherence groups. However, at the follow up, best adherence group had significantly less disability while the three groups were similar with regards to psychopathology. Fig. 3 shows the course of disability among the three adherence groups. The group X time interaction effect was significant (F=2.97; P=0.05) indicating that the best adherence group had the maximum benefit.

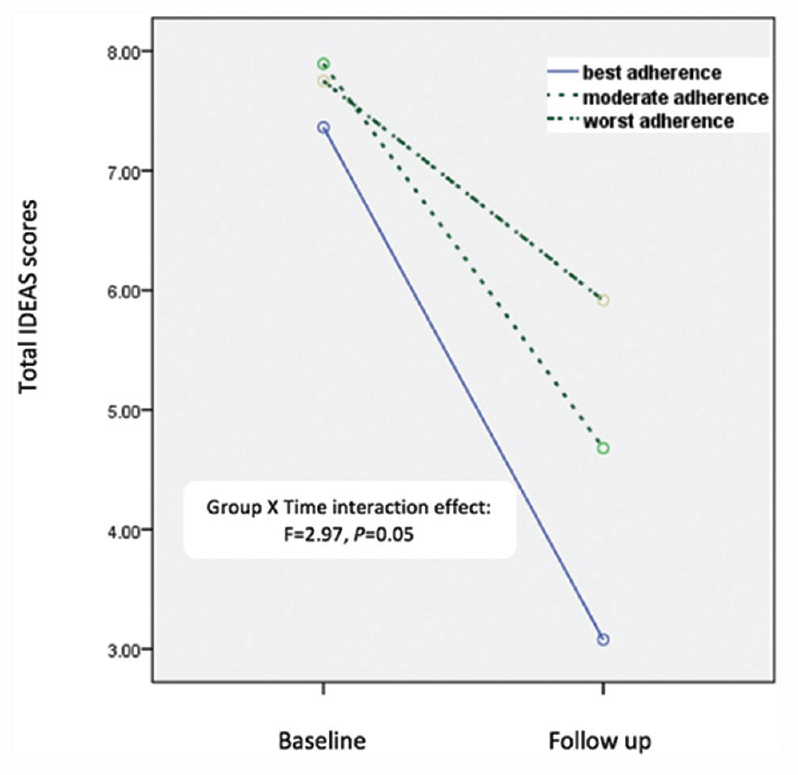
- Course of disability among the three adherence groups. IDEAS, Indian Disability Evaluation and Assessment Scale.
The proportion of patients with disability reduced from 134 (66.7%) to 55 (27.3%; P<0.01). The proportion of patients meeting criteria for disability was 31/142 (21.8%), 11/29 (37.9%) and 13/30 (43.3%) for the best, moderate and worst adherence groups, respectively (P<0.05). In the best-adherence group, the proportion of patients with a disability was significantly lower at follow up [31/142 (21.8%)] than at the baseline [94/142 (66.2%); P<0.01)]. The disability status of the moderate-adherence group also improved significantly [(20/29 (69.0%) at the baseline vs. 11/29 (37.9%) at follow up (P<0.05)]. However, there was no difference in the proportion of disabled people in the worst-adherence group [20/30 (66.7%) at baseline vs. 13/30 (43.3%) at follow up; P=0.09]. Finally, only 17 patients had total IDEAS scores of zero at recruitment. This number increased to 65 at the end of follow up period.
Discussion
In our study 69.6 per cent rural schizophrenia patients had satisfactory outcome over a four-year period when they received antipsychotic medications and low-intensity psychoeducation. Overall outcomes were better in terms of symptom severity, remission from the episodes, as well as disability. Disability was particularly less among those with better medication adherence. The study suggested that the public health strategy of ensuring continuous antipsychotic medications and low-intensity psychoeducation could favourably influence the course of schizophrenia and limit disability in patients living in rural communities of India. Similar intervention has been shown to be successful earlier as well albeit in a different kind of patient sample18. Patients in that particular study were all treatment seekers from community outreach clinics and not truly community dwelling.
In the study, unlike disability, desirable association did not emerge between symptom severity and treatment adherence. Although this may suggest that better adherence is not related to lesser symptoms, a couple of other interpretations are also possible: (i) disability is a relatively stable trait when compared to symptom severity and on and off changes in adherence is likely to affect symptoms much more than disability. (ii) Compared to other adherence groups, baseline PANSS score itself was less in the best adherence group and this could be one reason for the differences not reaching statistical significance at the end of follow up.
Experiments of brief training programmes in which primary care doctors are trained in identification and pharmacological treatment of psychiatric disorders including schizophrenia have been shown to be successful19. Families also actively take the role of case-managers by supervising medication, making the patient work at home or family professions, etc.
Structured psychosocial interventions are manpower-intensive. Due to shortage of this workforce in our country, it is reasonable to suggest that such structured interventions may be reserved for those who have suboptimal outcomes with antipsychotic medications and low-intensity psychoeducation. One discouraging observation was that 30 per cent of our patients had worst outcomes both in terms of clinical remission and disability. Clearly, antipsychotic medications alone were not sufficient in these patients. Structured community-level psychosocial interventions are indicated precisely for such patients. Chatterjee et al20 found modest efficacy of ‘collaborative community-based care plus facility-based care intervention’ over ‘facility-based care’ alone, especially for reducing disability and symptoms of psychosis.
The proportion of patients showing different patterns of course in our study was comparable to the earlier longitudinal studies of schizophrenia conducted across India16212223. However, our patients group differed from them as it consisted of a mixture of treated and untreated patients residing in the community. A recent report of a study conducted in a rural community in Madhya Pradesh13 also reported substantial reduction in disability over four years of follow up after providing community-based rehabilitation programme. This study had a mixture of patients with schizophrenia (n=128; 54.2%), bipolar affective disorders (n=68; 28.8%) and other psychoses (n=40; 16.9%). Moreover, figures for schizophrenia have not been provided separately. Hence, it is difficult to compare our findings with findings of this study.
Following were the limitations of our study: (i) Although the majority had a favourable outcome and though better adherence was associated with better outcome, the results could not be interpreted as providing definitive evidence for antipsychotics’ efficacy in reducing disability as there was no randomized comparison of different groups. Ethical and practical considerations acted as serious deterrents to conduct such studies, especially among community dwelling patients; (ii) In a naturalistic follow up study of this nature, several confounding factors might have influenced the association between treatment and outcome. For instance, patients might have become poorly adherent to medications because they did not perceive appreciable benefit; the association between adherence and outcome may, in fact, reflect this point. This factor figured as a reason for non-adherence in a recent observational study from another group of persons with First Episode Schizophrenia24. We had earlier observed that poorly adherent patients also had poor family support7. The latter could have contributed to their disability; (iii) Assessment of symptoms and disability were done by different raters during successive follow up. This issue could have influenced the results in a biased manner. (iv) The medication side-effects and burden of their cost were not reported. However, during the period of follow up, very low occurrence of tardive dyskinesias was observed in this group of patients. In the absence of gold standard methods to address these issues, an in-depth analysis of the naturalistic data is essential.
In conclusion, our study showed that ensuring adherence to antipsychotic medications and low-intensity psychoeducation could be a reasonable public health strategy to cater to about two-thirds of community dwelling patients with schizophrenia. Structured psychosocial interventions may be indicated in the significant minority who show suboptimal outcome with this strategy. Future studies could address the limitations mentioned above.
Acknowledgment
The CoInPsyD programme was supported by the research grants from the National Mental Health Programme, Government of India to the last author (BNG) and institutional research grants (National Institute of Mental Health and Neurosciences, Bengaluru, India) to the first two authors (CNK, JT).
Conflicts of Interest: None.
References
- Size of burden of schizophrenia and psychotic disorders. Eur Neuropsychopharmacol. 2005;15:399-409.
- [Google Scholar]
- Practice guidelines for the treatment of patients with schizophrenia (2nd ed). Arlington, VA: American Psychiatric Association; 2004.
- Antipsychotic drugs versus placebo for relapse prevention in schizophrenia: A systematic review and meta-analysis. Lancet. 2012;379:2063-71.
- [Google Scholar]
- London: NICE; 2014.
- National mental health programme: Manpower development scheme of eleventh five-year plan. Indian J Psychiatry. 2011;53:261-5.
- [Google Scholar]
- Prospective comparison of course of disability in antipsychotic-treated and untreated schizophrenia patients. Acta Psychiatr Scand. 2009;119:209-17.
- [Google Scholar]
- World Health Organization. The ICD-10 Classification of Mental and Behavioral Disroers: Clinical description and diagnostic guidelines. Geneva: WHO; 1992.
- [Google Scholar]
- The Mini-International Neuropsychiatric Interview (M.I.N.I.): The development and validation of a structured diagnostic psychiatric interview for DSM-IV and ICD-10. J Clin Psychiatry. 1998;59(Suppl 20):22-33.
- [Google Scholar]
- The positive and negative syndrome scale (PANSS) for schizophrenia. Schizophr Bull. 1987;13:261-76.
- [Google Scholar]
- Rehabilitation Committee of the Indian Psychiatric Society. Indian Disability Evaluation and Assessment Scale (IDEAS): A Scale for Measuring and Quantifying Disability in Mental Disorders. Gurgaon: Indian Psychiatric Society; 2002.
- [Google Scholar]
- Outcomes of people with psychotic disorders in a community-based rehabilitation programme in rural India. Br J Psychiatry. 2009;195:433-9.
- [Google Scholar]
- World Health Organization. Schizophrenia – an international follow-up study. Chichester: Wiley; 1979.
- [Google Scholar]
- Remission in schizophrenia: Proposed criteria and rationale for consensus. Am J Psychiatry. 2005;162:441-9.
- [Google Scholar]
- Factors associated with the course and outcome of schizophrenia in India. Results of a two-year multicentre follow-up study. Br J Psychiatry. 1989;154:499-503.
- [Google Scholar]
- Risperidone nonadherence and return of positive symptoms in the early course of schizophrenia. Am J Psychiatry. 2011;168:286-92.
- [Google Scholar]
- Community outreach for untreated schizophrenia in rural India: A follow-up study of symptoms, disability, family burden and costs. Psychol Med. 2005;35:341-51.
- [Google Scholar]
- Management of priority mental disorders in the community. Indian J Psychiatry. 1981;23:174-8.
- [Google Scholar]
- Effectiveness of a community-based intervention for people with schizophrenia and their caregivers in India (COPSI): A randomised controlled trial. Lancet. 2014;383:1385-94.
- [Google Scholar]
- Long term course and outcome of the Agra cases in the International Pilot Study of Schizophrenia. Acta Psychiatr Scand. 1984;70:170-9.
- [Google Scholar]
- Schizophrenia: Manifestations, incidence and course in different cultures. A World Health Organization ten-country study. Psychol Med Monogr Suppl. 1992;20:1-97.
- [Google Scholar]
- Twenty-year course of schizophrenia: The Madras Longitudinal Study. Can J Psychiatry. 2004;49:564-9.
- [Google Scholar]
- Reasons for non-adherence to antipsychotic medications in first episode schizophrenia in India: Results from a Prospective Study. 10th World Congress of the World Association for Psychosocial Rehabilitation; 2009 Nov 12-15, Bangalore, India. 2009
- [Google Scholar]






