Translate this page into:
Antimicrobial resistance in beta-haemolytic streptococci in India: A four-year study
For correspondence: Dr Purva Mathur, Department of Laboratory Medicine, Jai Prakash Narayan Apex Trauma Centre, All India Institute of Medical Sciences, New Delhi 110 029, India e-mail: purvamathur@yahoo.co.in
-
Received: ,
This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Background & objectives:
The incidence and severity of invasive and non-invasive infections demonstrate variability over time. The emerging resistance of Group A streptococci (GAS) to commonly used antibiotics is of grave concern. This study was conducted to assess the antimicrobial resistance of beta-haemolytic streptococci (βHS) in India and to ascertain the molecular mechanisms of resistance.
Methods:
All isolates of βHS from the Trauma Centre of All India Institute of Medical Sciences (AIIMS) (north India), and heavily populated area of old Delhi from 2010 to 2014 and Yashoda Hospital, Secunderabad (in south India, 2010-2012) and preserved isolates of βHS at AIIMS (2005-2009) were included. Phenotypic confirmation was done using conventional methods and the Vitek 2. Antibiotic sensitivity testing was done by disc diffusion and E-test. Detection of resistance genes, erm(A), erm(B), mef(A), tet(M) and tet(O), was done by polymerase chain reaction (PCR).
Results:
A total of 296 isolates of βHS (240 from north and 21 from south India) were included in the study. Of the 296 βHS, 220 (74%) were GAS, 52 (17.5%) were Group G streptococci and 11 (3.7%), 10 (3.3%) and three (1%) were Group B streptococci, Group C streptococci and Group F streptococci, respectively. A total of 102 (46%) and 174 (79%) isolates were resistant to tetracycline and erythromycin, respectively; a lower resistance to ciprofloxacin (21, 9.5%) was observed. A total of 42 (14%) and 30 (10%) isolates, respectively, were positive for tet(M) and erm(B) genes. Only 13 (5%) isolates were positive for mef(A). None of the isolates were positive for erm(A) and tet(O). There was discordance between the results of E-test and PCR for erythromycin and tetracycline.
Interpretation & conclusions:
A high level of resistance to erythromycin and tetracycline was seen in βHS in India. Discordance between genotypic and phenotypic results was reported. Absence of erm(A) and tet(O) with high prevalence of tet(M) and erm(B) was observed.
Keywords
Antimicrobial resistance
beta-haemolytic streptococci
Group A streptococci
Group C streptococci
Group G streptococci
Infections due to beta-haemolytic streptococci (βHS) vary from mild, self-limiting to potentially fatal ones1. There has been an increase in invasive infections by Group A streptococci (GAS) and non-GAS alike. Group G streptococci and Group C streptococci (GGS and GCS) are increasingly found to be associated with infections in humans and are together classified as Streptococcus dysgalactiae ssp. equisimilis (SDSE)2. In India, the disease burden of streptococcal infections and its sequela in the form of rheumatic fever and rheumatic heart disease are considerable34. There appears to be a geographical predilection for throat and skin infections by GAS, with a high prevalence of pharyngitis in the north, as compared to pyoderma in the southern part of India567.
Although GAS stands rather alone in being universally susceptible to penicillin, reports of rising minimum inhibitory concentration (MIC) or diminished susceptibility to penicillin are causing concern89. Simultaneously, macrolide resistance and therapeutic failure are also increasing9. This resistance is mediated by methylation of the adenine residue of the target, 23S rRNA, encoded by two classes of gene, i.e. erm(A) and erm(B) (erythromycin resistance methylase), which causes constitutive or inducible resistance phenotypes1011. A unique pattern of resistance (M phenotype) caused by mef(A) gene encoded acute-drug efflux pump is also seen11. However, it is characterized by resistance only to macrolides-lincosamides-streptogramines (MLS) to 14- and 15-membered macrolides.
GAS has maintained a reasonable level of susceptibility to tetracycline, being an alternative for penicillin-allergic patients infected with macrolide-resistant strains. Resistance to tetracycline is due to genetic acquisition of ribosomal protection genes - tet(O) and tet(M)111213. These are generally associated with conjugative chromosomal elements, which encode for their own transfer. These conjugation transposons transfer mobilizable plasmids to other isolates and species and even unlinked genomic DNA.
Studies on GAS distribution and antimicrobial resistance have been performed worldwide, but there is a paucity of information from India, where the epidemiology of GAS infections may be different. To understand the mechanism of this rapid resistance among streptococcal isolates, studies on the molecular basis are required. This study was conducted to understand the pattern of antimicrobial resistance in GAS and non-GAS isolates and to ascertain their molecular resistance mechanisms.
Material & Methods
The study was conducted in the Microbiology Laboratory of Jai Prakash Narayan Apex Trauma Centre of All India Institute of Medical Sciences (AIIMS), New Delhi, a tertiary care hospital of India.
Bacterial isolates
The βHS were recovered from clinical samples of patients under the following groups:
(i) Trauma patients (north India): This group included βHS (n=191) recovered from various clinical samples of patients admitted to the trauma centre, AIIMS, New Delhi, and from those presenting to its outpatient department, between April 2010 and December 2014.
(ii) Pharyngitis patients (north India): This group included βHS recovered from a total of 20 patients who presented with pharyngitis/tonsillitis to an outdoor clinic situated in a heavily populated area of old Delhi between April 2010 and December 2014.
(iii) Patients (south India): This group included all βHS (n=21) recovered from clinical samples of patients admitted/presented to Yashoda Hospital, Secunderabad (in south India, 500 bedded), between June 2010 and March 2012.
(iv) Preserved isolates of βHS at AIIMS (north India): A total of 64 isolates of βHS, which were isolated at microbiology laboratory of the AIIMS hospital from pus samples between 2005 and 2009, were also included in the study. All these isolates were also from wounds/postoperative samples.
The study protocol was approved by the Institute's ethical committee.
βHS was identified by the standard microbiological methods. The identification was confirmed for all isolates by the Vitek 2 identification cards (BioMerieux, France). Grouping of the streptococci was performed by agglutination test (HiMedia Labs, Mumbai) according to the manufacturer's instructions.
All the isolates were stocked at −70°C for further analysis in stocking beads (Microbank™, Pro-Lab Diagnostics, Richmond Hill, Canada).
Antimicrobial susceptibility testing: The antimicrobial susceptibility testing of streptococci was performed by the disc diffusion method on Mueller-Hinton agar with five per cent sheep blood according to the recommendations of the Clinical and Laboratory Standards Institute14. The antibiotics tested were penicillin G, ampicillin, clindamycin, vancomycin, linezolid, erythromycin, ciprofloxacin, tetracycline, cefotaxime, ceftriaxone, teicoplanin, levofloxacin and chloramphenicol. Streptococcus pneumoniae ATCC 49619 was used as control for antimicrobial susceptibility testing. The MIC was determined by E-test for all the above antimicrobials, which was performed according to the manufacturer's recommendations (BioMerieux Ltd., formerly AB Biodisk, Sweden).
D-test: D-test was done for the isolates which were erythromycin resistant and clindamycin susceptible. Standard disc diffusion D-zone testing was performed using erythromycin and clindamycin disks placed 20 mm apart on Mueller-Hinton five per cent sheep blood agar plates incubated at 37°C in five per cent CO2 for 48 h. Blunted, D-shaped clear zone around clindamycin disk proximal to the erythromycin disk indicated a positive D-test result.
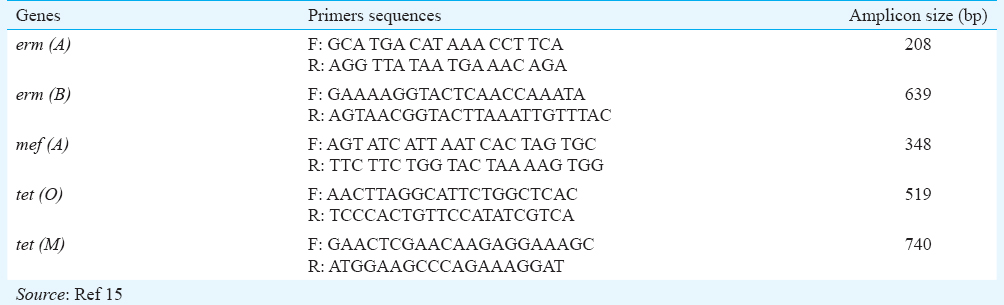
Detection of resistance genes by polymerase chain reaction (PCR): erm(A) and erm(B); tet(O) and tet(M) and mef(A) genes were detected by PCR15. For this, DNA was isolated by commercially available DNA extraction kit (QIAamp DNA Blood Mini Kit, Qiagen, Hilden, Germany) directly from pure culture. Primers used for the amplifications are shown in Table I. PCR amplification was performed with an initial eight minutes denaturation at 94°C followed by 30 cycles of denaturation at 94°C for 30 sec, 30 sec of annealing at the appropriate temperature for each gene and 60 sec of extension at 72°C with a final extension step at 72°C for seven minutes. For standardization of erm(B), mef(A) and tet(M), phenotypically resistant laboratory clinical strains were used as positive control, and iB21 was used for erm(A) and tet(O) [courtesy of Pietro E. Varaldo, M.D and Dr. Vitali Luca A., University of Camerino, School of Pharmacy, Microbiology Unit, Camerino (MC)]. Amplicons were identified by gel electrophoresis in 1.5 per cent gel with ethidium bromide.
Results
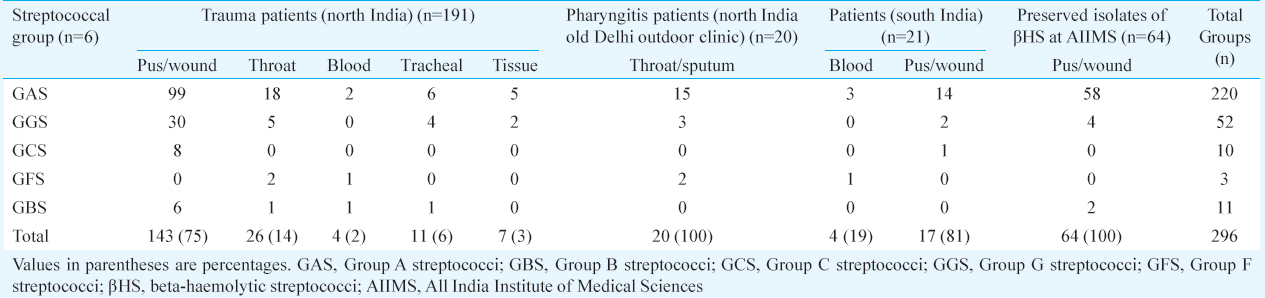
A total of 296 βHS isolates were obtained from the various sources. Of these 296 βHS, 220 (74%) were GAS, 52 (17.5%) were GGS and 11 (3.7%), 10 (3.3%) and three (1%) were Group B streptococci (GBS), GCS and Group F streptococci (GFS), respectively. Pus (75.6%) was the most common source followed by throat swabs (15%). Eight isolates were recovered from invasive bloodstream infections. After Streptococcus pyogenes, S. dysgalactiae was the most common species (14%) isolated. Of these 296 isolates, 46 (16%) were non-invasive isolates from throat and sputum and 250 (84%) invasive isolates were from blood, pus, tracheal and other tissues. Distribution of all the invasive and non-invasive clinical specimens from different hospitals is given in Table II.
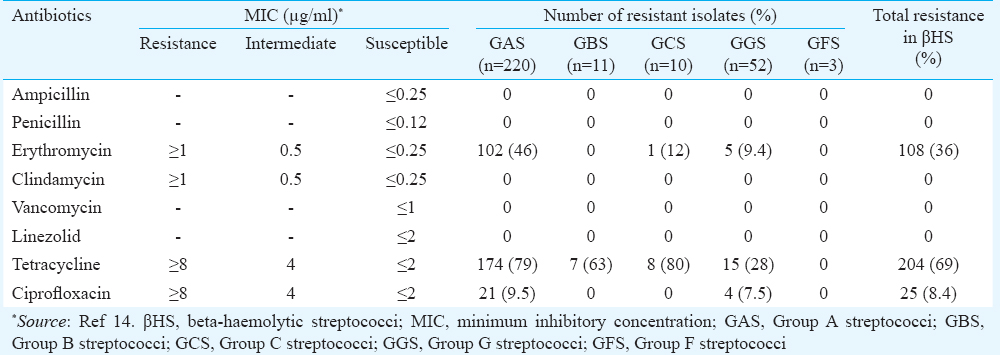
Antimicrobial resistance: Antimicrobial susceptibility testing (disc diffusion test and E-test) revealed all the isolates to be sensitive to penicillin G, ampicillin, clindamycin, vancomycin and linezolid, with variable resistance levels to erythromycin, tetracycline and ciprofloxacin. Among GAS isolates, resistance to erythromycin, tetracycline and ciprofloxacin was seen in 102 (46%), 174 (79%) and 21 (9.5%) isolates, respectively. Sixty two isolates (30.6%) were resistant to both erythromycin and tetracycline and nine isolates (4%) were resistant to three different classes of drugs. The phenotypic results of antimicrobial resistance for other βHS are shown in Table III. Of the 220 GAS isolates, 61 (28%) were found to be erythromycin resistant and clindamycin susceptible. Inducible clindamycin resistance phenotype was observed in all 61 GAS isolates by D-test. Hundred per cent concordance was seen between the phenotypic tests for the determination of antimicrobial susceptibility.
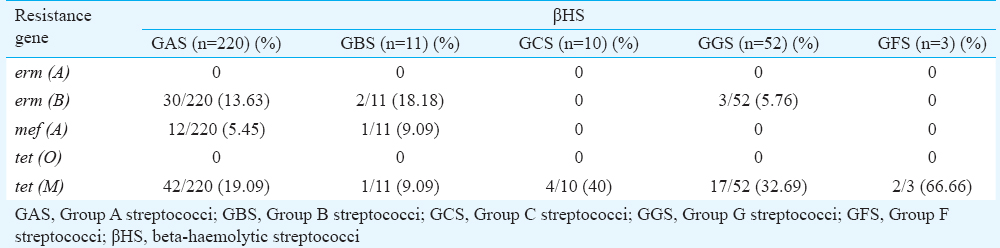
The presence of erm(B) and tet(M) genes was observed in 30 (10%) and 42 (14%) isolates, respectively, with absence of erm(A) and tet(O) gene in any GAS isolates. Of the 275 isolates from north India, erm(A), mef(A) and tet(M) were present in 58 (24%), 11 (5%) and 60 (25%), and of the 21 isolates from south India, erm(B), mef(A) and tet(M) were present in two (10%), two (10%) and six (29%), respectively. The genotypic results of antimicrobial resistance for other βHS are shown in Table IV and V.
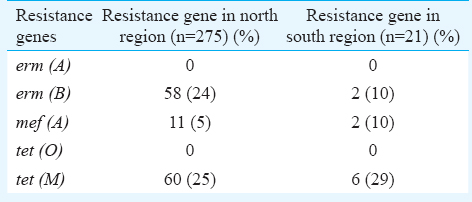
Antimicrobial resistance phenotype (by disc diffusion test or E-test) was not observed in the absence of resistance gene [erm(B) and tet(M)]. Resistance rates observed were 28 per cent for erythromycin and 57 per cent for tetracycline by both E-test and disc diffusion testing; however, only 20 and 25 per cent of the isolates were observed to harbour erm(B) and tet(M) genes, respectively.
Discussion
The prevalence of invasive and non-invasive streptococcal infections has increased gradually in India and other Asian countries13161718. In our study, GAS was the predominant βHS followed by GGS. In our earlier study, 142 βHS isolates were recovered, of which 25 (18%) were Group C and Group G streptococci (GCGS) recovered from pus, wound, respiratory tract and blood19. In the present study, a higher prevalence of GGS and SDSE was seen. The clinical presentation of GGS was found to be often similar to GAS. Moreover, antimicrobial resistance has been increasing in both. Thus, isolation of both these pathogens and monitoring their antimicrobial resistance patterns are important.
Despite the increasing incidence of invasive GAS infection worldwide, the organism remains sensitive to penicillin and other commonly used β-lactam antibiotics. Although GAS remains sensitive to penicillin, the worldwide spread of erythromycin and clindamycin resistance is also emerging as a major problem since erythromycin is the choice of treatment in penicillin-allergic patients. In the present study, βHS was found susceptible to all antimicrobial agents, except erythromycin, tetracycline and ciprofloxacin. High rates of resistance to erythromycin (28%) and tetracycline (57%) were found, while 10 per cent isolates displayed resistance to ciprofloxacin.
Erythromycin resistance rates vary from low to high in different geographic area20212223. In a four-year surveillance study conducted in UK and Ireland in 2006, erythromycin resistance was reported as 10.8 per cent, which increased over time24. In contrast to this, in an eight-year study from northern India, erythromycin resistance was reported to be only 2.6 per cent only18. The prevalence of macrolide resistance in GAS is low and limited to certain geographical regions252627. In our study, 46 per cent resistance in GAS and nine per cent in GGS to macrolides was observed.
Tetracycline is a choice for the empirical treatment for invasive βHS infections. A high rate of tetracycline resistance (79%) was observed in GAS in our study, similar to other reports from the world2223. Since resistance of GAS and GGS to tetracycline has been reported to be very high, it can no longer be included as an option in the empirical treatment of patients infected with βHS.
In North America and Europe, the incidence of fluoroquinolone resistance among βHS (1%) remains low28; in contrast, we observed a high (10%) rate of ciprofloxacin resistance. This study was also aimed to add information on antibiotic resistance mechanism and genotypic characterization of βHS. In the present study, the presence of erm(B), tet(M) and mef(A) revealed the mechanism of resistance in the βHS in north and south regions of the country. Wajima et al29 from Japan found macrolides resistance in 16.2 per cent strains, while the percentage of strains possessing the resistance genes erm(A), erm(B) and mef(A) was 2.5, 6.2 and 7.5 per cent, respectively. Another study from Korea in 992 healthy school children observed the presence of erm(B) and mef(A) in 62.5 and 31.3 per cent isolates, respectively30. Our data showed that tet gene was responsible for tetracycline resistance, and of the two tetracycline resistance genes [tet(O) and tet(M))] studied, only tet(M) was present in isolates from north and south regions of India. In erythromycin, only erm(B) and mef(A) were found in the present study. A difference in phenotypic and genotypic pattern of resistance was observed. Most of the published studies have shown 100 per cent agreement of PCR results with the phenotypic detection methods31. However, in our study, only 50 per cent agreement was observed between the phenotypic and genotypic tests because the studied gene was not expressed and resistance might be mediated by other mode of resistance.
In the present study, 100 per cent concordance was found in D-test for inducible clindamycin resistance. D-test should be used as a routine method for the detection of inducible clindamycin resistance, which might help in the empirical treatment of the patients. Our results indicated that phenotypic testing was more important than the genotypic testing and only phenotypic tests should be preferred in routine clinical microbiology. However, for the better understanding of the mechanisms of antibiotic resistance and for the epidemiological studies, both phenotypic and genotypic tests should be done.
In conclusion, an alarmingly high level of antimicrobial resistance was observed amongst βHS from India. Based on our findings, it may be suggested that for better understanding of antibiotic resistance, both phenotypic and PCR-based tests should be done to accurately identify the resistant isolates. The reason for phenotypic resistance in the absence of a resistance gene could not be ascertained.
Financial support & sponsorship: This study was funded by a grant from the Indian Council of Medical Research (ICMR), New Delhi
Conflicts of Interest: None.
References
- A decade of molecular pathogenomic analysis of group A Streptococcus. J Clin Invest. 2009;119:2455-63.
- [Google Scholar]
- Group C and G streptococci infections: Emerging challenges. Clin Lab Sci. 2003;16:209-13.
- [Google Scholar]
- Rheumatic fever and rheumatic heart disease in India at the turn of the century. Indian Heart J. 2001;53:35-7.
- [Google Scholar]
- Topley and Wilson's Microbiology and Microbial Infections. Vol 3. (9th ed). London: Oxford Press; 1998. p. :257-75.
- [Google Scholar]
- Molecular typing of Streptococcus pyogenes from remote aboriginal communities where rheumatic fever is common and pyoderma is the predominant streptococcal infection. Epidemiol Infect. 2007;135:1398-405.
- [Google Scholar]
- Heterogeneity of community based pediatric GAS isolates from India: Challenges to the multivalent vaccine. 2006:49-53. Streptococci - New insights into an old enemy Amsterdam: Elsevier
- [Google Scholar]
- High diversity of group A streptococcal emm types in an Indian community: The need to tailor multivalent vaccines. Clin Infect Dis. 2005;40:46-51.
- [Google Scholar]
- Emerging resistance to erythromycin and penicillin among Streptococcus pyogenes isolates in Zagazig, Egypt. Int J Curr Microbiol Appl Sci. 2014;3:750-6.
- [Google Scholar]
- Resistance to erythromycin and rising penicillin MIC in Streptococcus pyogenes in India. Jpn J Infect Dis. 2006;59:334-6.
- [Google Scholar]
- Genetic elements responsible for erythromycin resistance in streptococci. Antimicrob Agents Chemother. 2009;53:343-53.
- [Google Scholar]
- The macrolide resistance genes erm(B) and mef(E) are carried by tn2010 in dual-gene Streptococcus pneumoniae isolates belonging to clonal complex CC271. Antimicrob Agents Chemother. 2007;51:4184-6.
- [Google Scholar]
- High rate of tetracycline resistance in Streptococcus pyogenes in Iran: An epidemiological study. J Clin Microbiol. 2000;38:2103-7.
- [Google Scholar]
- Tetracycline antibiotics: Mode of action, applications, molecular biology, and epidemiology of bacterial resistance. Microbiol Mol Biol Rev. 2001;65:232-60.
- [Google Scholar]
- Performance Standards for Antimicrobial Susceptibility Testing. In: Sixteenth Informational Supplement M100-S16. Wayne, PA: CLSI; 2006.
- [Google Scholar]
- Distribution and molecular analysis of mef(A)-containing elements in tetracycline-susceptible and -resistant Streptococcus pyogenes clinical isolates with efflux-mediated erythromycin resistance. J Antimicrob Chemother. 2004;54:991-8.
- [Google Scholar]
- Antibiotic resistance pattern of group-a beta-hemolytic streptococci isolated from North Indian children. Indian J Med Sci. 2008;62:392-6.
- [Google Scholar]
- Invasive beta-haemolytic streptococcal infections in a tertiary care hospital in Northern India. J Med Microbiol. 2002;51:791-2.
- [Google Scholar]
- Antimicrobial susceptibility pattern of β-haemolytic group A, C and G streptococci isolated from North India. J Med Microbiol. 2013;62:386-93.
- [Google Scholar]
- Clinical and molecular epidemiology of beta-hemolytic streptococcal infections in India. J Infect Dev Ctries. 2014;8:297-303.
- [Google Scholar]
- Epidemiology of invasive group B streptococcal disease in Alberta, Canada, from 2003 to 2013. J Clin Microbiol. 2016;54:1774-81.
- [Google Scholar]
- Antibiotic susceptibility evaluation of group A Streptococcus isolated from children with pharyngitis: A study from Iran. Infect Chemother. 2015;47:225-30.
- [Google Scholar]
- Antibiotic susceptibility and molecular mechanisms of macrolide resistance in streptococci isolated from adult cystic fibrosis patients. J Med Microbiol. 2015;64:1375-86.
- [Google Scholar]
- Resistance genes and genetic elements associated with antibiotic resistance in clinical and commensal isolates of Streptococcus salivarius. Appl Environ Microbiol. 2015;81:4155-63.
- [Google Scholar]
- Non-susceptibility trends among enterococci and non-pneumococcal streptococci from bacteraemias in the UK and Ireland, 2001-06. J Antimicrob Chemother. 2008;62(Suppl 2):ii75-85.
- [Google Scholar]
- Molecular characterization and antibiotic resistance of clinical Streptococcus dysgalactiae subsp. equisimilis in Beijing, China. Infect Genet Evol. 2016;40:119-25.
- [Google Scholar]
- Molecular analysis of Streptococcus pyogenes macrolide resistance of paediatric isolates during a 7 year period (2007-13) J Antimicrob Chemother. 2016;71:2113-7.
- [Google Scholar]
- Drug resistance characteristics and macrolide-resistant mechanisms of Streptococcus pneumoniae in Wenzhou city, China. Med Sci Monit. 2016;22:2731-5.
- [Google Scholar]
- Prevalence of erythromycin and clindamycin resistance among clinical isolates of the Streptococcus anginosus group in Germany. J Med Microbiol. 2009;58:222-7.
- [Google Scholar]
- Distribution of emm type and antibiotic susceptibility of group A streptococci causing invasive and noninvasive disease. J Med Microbiol. 2008;57:1383-8.
- [Google Scholar]
- Epidemiology and antibiotic resistance of group A streptococci isolated from healthy schoolchildren in Korea. J Antimicrob Chemother. 2004;54:447-50.
- [Google Scholar]
- Detection of macrolide resistance mechanisms in Streptococcus pneumoniae and Streptococcus pyogenes using a multiplex rapid cycle PCR with microwell-format probe hybridization. J Antimicrob Chemother. 2001;48:541-4.
- [Google Scholar]






