Translate this page into:
Anterior pituitary hormone dysfunction among individuals with complete heart block requiring pacemaker
For correspondence: Dr Bashir Ahmad Laway, Department of Endocrinology, Sher-I-Kashmir Institute of Medical Sciences, Srinagar, Jammu & Kashmir 190 011, India e-mail: drlaway@gmail.com
-
Received: ,
Abstract
Background & objectives
Neuronal hypoxia associated with conditions like traumatic brain injury and cardiac tachyarrhythmia has been implicated in causing hypopituitarism. Individuals with complete heart block (CHB) may be predisposed to develop anterior pituitary hormone dysfunction in the long term. The objective of this study was to investigate anterior pituitary hormone functions in individuals after CHB.
Methods
This prospective cohort study included 30 individuals (21 men and 9 women) with CHB requiring pacemaker implantation, who were evaluated at admission and then at a mean follow up of 12.4 ± 2.2 months to look for development of any degree of hypopituitarism. In addition to the measurement of hormones like follicle-stimulating hormone (FSH), luteinising hormone (LH), thyroid stimulating hormone (TSH), total tetra iodothyronines (TT4), free tetraiodothyronines (FT4), cortisol, insulin-like growth factor-1 (IGF-1), testosterone and estradiol, a fixed-dose glucagon stimulation test (GST) was performed to assess growth hormone (GH) and adrenocorticotrophic hormone (ACTH) axis.
Results
The mean age of the participants was 64.9 ± 11.3 yr. At follow up evaluation, 17 (56.7%) had low serum IGF-1, and among them, seven (23%) had growth hormone deficiency (GHD) (peak GH <1.0 ng/ml after GST). Six participants (20%) had ACTH deficiency (peak cortisol <9 ug/dl after GST) and one had TSH deficiency. None had prolactin (PRL) or gonadotropin deficiency. Overall, hormone deficiencies were observed in nine patients (30%).
Interpretation & conclusions
This pilot study detected loss of anterior pituitary hormones in a significant number of individuals of CHB at 12 months follow up. Unrecognised hypopituitarism may have resulted in significant morbidity and mortality in these individuals.
Keywords
Arrhythmia
growth hormone deficiency
heart block
hypopituitarism
pituitary
Acquired hypopituitarism is mostly caused by tumours of the sellar region, pituitary surgeries, radiotherapy and inflammatory disorders1,2. Cardiovascular insults like severe postpartum haemorrhage (PPH), traumatic brain injury (TBI) and subarachnoid haemorrhage (SAH) are other causes of hypopituitarism3,4. Neuronal hypoxia and neuro-inflammation have been proposed as probable mechanisms leading to hypopituitarism in these vasogenic conditions5, 7. The pituitary gland, by virtue of its unique blood supply from hypothalamic portal vessels, is prone to ischemia8. Cardiac arrhythmias leading to neuronal hypoxia and an increase in pro-inflammatory cytokines within the central nervous system9,10 is an unusual cause of hypopituitarism, mainly growth hormone deficiency (GHD)11. Complete heart block (CHB) is a cardiac arrhythmia that presents with pre-syncope to hemodynamic instability and encephalopathy12. Whether individuals with CHB develop pituitary dysfunction on follow up is so far not known. Hence, the aim of this prospective observational pilot study was to investigate anterior pituitary hormone functions among individuals with CHB on follow up.
Material & Methods
Study population
This study was conducted in the department of Endocrinology and Cardiology at Sher-I-Kashmir Institute of Medical Sciences, a tertiary care hospital in North India between October 2017 and January 2019. Thirty consecutive individuals admitted to the cardiac unit with the diagnosis of CHB and implanted with permanent pacemakers were included after procuring an informal consent from those willing to participate in this study. Individuals with malnutrition, chronic kidney disease, chronic liver disease, uncontrolled hypertension or diabetes mellitus (DM), malignancy, life-threatening illness, chronic infections, rheumatological diseases, history of cranial irradiation, existing pituitary disorder and using any medications that could interfere with pituitary axis were excluded from the study. Informed consent was obtained from all the participants and the study was approved by the Institutional Ethics Committee. All women included in the study were post-menopausal.
Sample collection and hormone testing
Blood samples(10 ml) were collected after an overnight fast between 0800 and 0900 h from all the participants within 24 h of hospitalisation for estimating serum thyroid stimulating hormone (TSH), total tri-iodothyronine (TT3), free tri-iodothyronine (FT3), total tetraiodothyronine (TT4), free tetraiodothyronines (FT4), luteinising hormone (LH), follicle-stimulating hormone (FSH), prolactin (PRL), total cortisol, insulin-like growth factor-1 (IGF-1), total testosterone (in men) and estradiol (in women). The participants continued on routine care (including the use of antihypertensives, beta-blockers, statins, aspirin, etc.) and were reassessed after a mean follow up of 12.4 ± 2.2 months (range 10-19 months, Figure). Repeat blood samples for TT3, TT4, FT3, FT4, FSH, TSH, PRL, LH, cortisol and IGF-1 were also collected and glucagon stimulation test (GST) was done to assess any growth hormone (GH) and adrenocorticotrophic hormone (ACTH) axis defect. Fixed-dose glucagon was used depending on the weight of the patient (<90 kg-1 mg; ≥90 kg-1.5 mg). The test was performed by giving glucagon (GlucaGen®, Novo Nordisk, Bagsvaerd, Denmark) intramuscularly and blood samples were obtained at 0, 60, 90, 120, 180 and 240 min after the injection for measurement of GH and cortisol13.
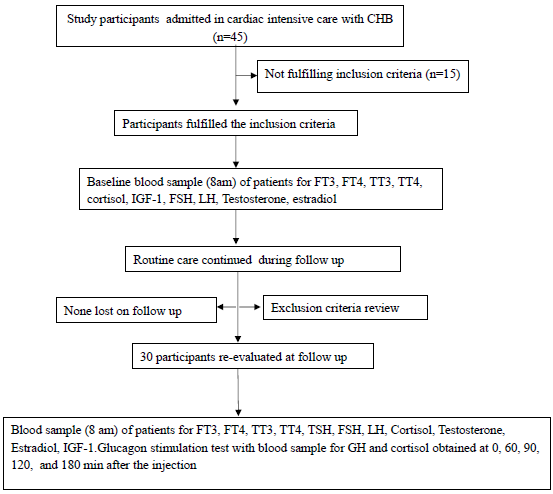
- PERT chart showing study design and flow (mean follow up 12.4 ± 2.2 months). PERT, program evaluation and review technique; TSH, thyroid stimulating hormone; TT3, total tri-iodothyronine; FT3, free tri-iodothyronine; TT4, total tetra iodothyronines; FT4, free tetraiodothyronines; LH, luteinising hormone; FSH, follicle stimulating hormone; IGF-1, insulin-like growth factor-1; GH, growth hormone; CHB, complete heart block.
Clinical assessment
The clinical assessment included recording of presenting symptoms, underlying comorbidities, weight, height, waist and hip circumference, blood pressure (BP), mean arterial pressure (MAP)14 and Glasgow Coma Scale (GCS). On follow up, a relevant history focusing on premature ejaculation or erectile dysfunction, decreased libido, dyspareunia, weight gain, fatigue, lethargy and decreased appetite was obtained.
Operational definitions and cut offs
In male participants, gonadotropin deficiency was defined as the total serum testosterone levels <180 ng/dl in the presence of normal or inappropriately low FSH (normal range: 1.6–11.6 IU/L) and LH (0.5–10 IU/L). In women, gonadotropin deficiency was defined by FSH of <27 IU/L (normal range: 27–129 IU/L) and LH of <7 IU/L (normal range: 7–58 IU/L). TSH deficiency was defined by FT4 < 0.6 ng/dl (normal range: 0.61–1.12 ng/dl) and TT4 <4 µg/dl (normal range: 4–13 µg/dl) in the presence of inappropriately low or normal TSH (0.5–4.5 mIU/ml). Hyperprolactinemia was defined as PRL greater than the normal range (women: 1–27 µg/L; men: 1–20 µg/L), while PRL deficiency was defined by PRL levels lower than the normal range. GH deficiency was defined as serum IGF-1 levels <80 ng/ml (normal range for age >50 yr: 80–237 ng/ml) and peak GH <1 ng/ml15. ACTH deficiency was defined as a basal cortisol level of <15 µg/dl and a peak cortisol value of <9 µg/dl after GST16.
Laboratory measurements
10 ml of blood sample was collected and analysed using the methods as described previously17. Measurements of urea, creatinine, bilirubin, alanine aminotransferase, alkaline phosphatase, total protein and albumin were carried out on the same day on an automated chemistry analyser (HITACHI-912). Plasma glucose was also estimated same day by enzymatic method using glucose oxidase and peroxidase on an automated chemistry analyser (HITACHI-912). Serum PRL, TSH, FT3, FT4, TT3, TT4, FSH, LH, cortisol, GH and testosterone were measured same day by commercial chemiluminescent immunoassay (Beckman Coulter Unicel, DXI-800). IGF-1600 ELISA kit was used to measure serum IGF-1 concentration (DEMEDITEC Germany, DE4140)
Statistical analysis
Statistical analysis was done using the IBM SPSS 20 (SPSS Inc, Chicago, IL, USA) programme. The normality of the sample was assessed by Kolmogorov-Smirnov test. Continuous variables were presented as mean ± standard deviation (SD) or median and interquartile range (IQR), depending on the normality of the data. Categorical variables were reported as frequencies and percentages. The chi-square test was employed for categorical variables to compare differences between groups. For continuous variables, the student-paired t-test was used when the data followed a normal distribution, while the Wilcoxon signed-rank test was applied for non-normally distributed data. Furthermore, we performed Pearson’s correlation analysis for normally distributed variables and Spearman’s rank correlation for non-normally distributed variables to determine if there were significant correlations between the selected variables. A P-value of less than 0.05 was considered as significant.
Results & Discussion
This study included 30 participants (21 men and 9 women) with a mean (± SD) age of 64.9 ± 11.3 yr (range 50–85 yr) and mean body mass index (BMI) of 24.6 ± 4.4 kg/m2 (range 19.6–44.1 kg/m2). Twenty-five participants were hypertensive and eight had controlled DM. The main presenting symptom was presyncope in 21 participants and syncope in nine (30%). The average MAP was 92.6±18 mmHg and the mean GCS was 14.5±1 (Table I). At hospitalisation, three participants (all women) had hyperprolactinemia, which normalised after two weeks and was attributed to prokinetics. Nine (eight men and one woman) had low T3 syndrome (low FT3 with normal TT4 and TSH). Gonadotropin deficiency was seen in three participants (2 men and 1 woman). Hyperprolactinemia and gonadotroph dysfunction were reversed on follow up. Low IGF-1 (age and sex-matched) was observed in seven individuals at baseline, of which five had normal IGF-1 and two had persistent low IGF-1 at follow up. Eighteen participants (13 men and 5 women) had borderline cortisol values (between 3 and 15 µg/dl) at baseline. The baseline and follow up hormonal parameters of individuals are described in Table II. At follow up, low serum IGF-1 was documented in 17 individuals (15 were new onset and 2 were persistent). Out of these, seven (23%) exhibited GHD, six (20%) demonstrated ACTH deficiency determined by peak serum cortisol <9 ug/dl after GST, one participant had TSH deficiency, while none showed deficiencies in PRL or gonadotropin levels. Overall, hormone deficiencies were observed in nine patients (30%), including two cases of isolated GHD, four cases of combined GHD and ACTH deficiency and one case of GHD combined with TSH deficiency. Moreover, two participants exhibited isolated ACTH deficiency (Table III and Supplementary Table I). There was no significant difference between hormone deficient and sufficient individuals in terms of age (63.71 + 12.41 vs. 68.22 + 8.64, P = 0.332), sex (P = 0.441), BMI (24.85 ± 4.99 vs. 23.29 ± 2.90, P = 0.564), GCS (14.38 ± 4.99 vs. 14.89 ± 0.33, P = 0.234), MAP (92.05 ± 18.97 vs. 93.67 ± 11.71, P = 0.532) or systolic (132.48 ± 23.48 vs. 127.56 ± 18.54, P = 0.232) and diastolic BP (71.90 ± 20.93 vs. 76.89 ± 10.54, P = 0.342). A positive correlation was seen between TT3 and GCS at admission (r = 0.4, P = 0.03); TT4 with MAP (r = 0.4, P = 0.04), diastolic BP (r = 0.5, P = 0.01) and GCS at admission (r = 0.4, P = 0.02). Similarly, there was a positive correlation between FT4 and MAP (r = 0.4, P = 0.04) and diastolic BP (r = 0.5, P = 0.01). No significant correlation was observed between GCS at presentation or MAP with serum IGF-1, peak GH or cortisol concentration.
| Parameters | Baseline | Follow up | P value | Reference range |
|---|---|---|---|---|
| Age (yr) | 65.08 ± 11.30 | 66.75 ± 7.78 | 0.066 | - |
| Weight (Kg) | 69.27 ± 11.43 | 71 ± 13.41 | 0.78 | - |
| BMI (Kg/m2) | 24.57 ± 4.41 | 24.88 ± 2.60 | 0.814 | 18-23 |
| SBP (mmHg) | 131 ± 21.48 | 120.56 ± 10.32 | 0.306 | 120-130 |
| DBP (mmHg) | 73.40 ± 18.86 | 72.91 ± 10.77 | 0.977 | 80-90 |
| MAP (mmHg) | 92.53 ± 17.70 | 89.66 ± 27.74 | 0.701 | <200 |
| Pulse rate (per min) | 44.60 ± 16.17 | 58.02 ± 12.12 | 0.014 | 60-100 |
| GCS | 14.53 ± 1.04 | 15 | 0.231 | 3-15 |
| Hb (g/dl) | 13.23 ± 2.19 | 13.98 ± 4.53 | 0.672 | 12-16 |
| TLC (X 103/ul) | 8.25 ± 3.09 | 9.18 ± 2.31 | 0.542 | 4-10 |
| PLT (X 103/ul) | 132.27 ± 66.54 | 134.23 ± 5.33 | 0.677 | 100-400 |
| BGF (mg/dl) | 88.48 ± 9.95 | 87.78 ± 9.48 | 0.451 | 70-100 |
| Urea (mg/l) | 44.43 ± 15.06 | 40.13 ± 12.56 | 0.342 | 13-45 |
| Creatinine (mg/dl) | 1.29 ± 0.24 | 1.1 ± 0.23 | 0.454 | 0.5-1.3 |
| Sodium (mEq/l) | 135.53 ± 11.4 | 136.76 ± 13.67 | 0.673 | 135-145 |
| Potassium (mEq/l) | 3.76 ± 0.57 | 4.01 ± 1.24 | 0.563 | 3.5-5.5 |
| Bilirubin (mg/dl) | 0.94 ± 0.43 | 0.87 ± 0.34 | 0.123 | 0.3-1.5 |
| ALT (IU/l) | 42.37 ± 12.14 | 40.23 ± 13.12 | 0.156 | 10-31 |
| ALP (IU/l) | 120.45 ± 45.09 | 112.45 ± 34.67 | 0.321 | 40-145 |
| Albumin (mg/dl) | 3.78 ± 0.43 | 3.98 ± 0.78 | 0.492 | 3.5-5.2 |
BMI, body mass index; SBP, systolic blood pressure; DBP, diastolic blood pressure; MAP, mean arterial pressure; GCS, glasgow coma scale; Hb, haemoglobin; TLC, total leucocyte count; PLT, platelet count; BGF, blood glucose fasting; ALT, alanine transaminase; ALP, alkaline phosphatase
| Parameters | Baseline | Follow up | P value | Reference range |
|---|---|---|---|---|
| TT4 (ug/dl) | 9.73 (8.04-11.10) | 8.5 (6.49-10.04) | 0.004 | 4-12 |
| TT3 (ng/ml) | 0.77 (0.67-0.94) | 1.10 (0.62-1.16) | 0.004 | 2.5-4.5 |
| FT4 (ng/dl) | 0.95 (0.83-1.16) | 0.78 (0.59-0.92) | 0.001 | 0.61-1.12 |
| TSH (IU/ml) | 2.41 (0.89-3.74) | 3.04 (2.07-5.08) | 0.001 | 2.5-4.5 |
| IGF-1 (ng/ml) | 95.31 ± 87.18 | 70.25 ± 38.53 | 0.889 | 80-237 |
| Testosterone (ng/dl) | 309.55 ± 111.03 | 406.54 ± 153.25 | 0.692 | 180-1200 |
| Estradiol (pg/ml) | 37.66 ± 14.04 | 40.55 ± 12.06 | 0.120 | 0-30 |
| LH (IU/L) | 9.47 (6.1-19.09) | 12.21(7.39-13.88) | 0.11 | Males: 0.5-10, Females: 7-58 |
| FSH (IU/L) | 14.32 (6.96-50.2) | 18.34 (8.06-69.83) | 0.001 | Males:1.6-11.6, Females: 27-129 |
| PRL (ng/ml) | 8.1 (6.3-16.98) | 11.66 (7.39-13.88) | 0.582 | Males: 1-20, Females: 1-27 |
| Cortisol (ug/dl) | ||||
| Cortisol- 0 min | 14.69 ± 5.75 | 10.12 ± 3.58 | 0.01 | 3-15 |
| Cortisol - 60 min | 8.24 ± 2.53 | - | ||
| Cortisol - 90 min | 8.46 ± 2.24 | - | ||
| Cortisol - 120 min | 10.28 ± 4.72 | - | ||
| Cortisol - 180 min | 9.05 ± 3.21 | - | ||
| Peak cortisol | 12.71 ± 4.39 | - | ||
| GH (ng/ml) | ||||
| GH-0 min | 0.66(0.21-1.55) | 0.20(0.06-0.69) | 0.05 | - |
| GH-60 min | 0.19 (0.06-1.21) | - | ||
| GH-90 min | 0.34 (0.12-1.69) | - | ||
| GH-120 min | 1.14 (0.14-4.3) | - | ||
| GH-180 min | 0.57 (0.14-2.07) | - | ||
| Peak GH | 2.57 (0.97-5.89) | - |
TT4, total thyroxine; TT3, total tri-iodothyronine; FT4, free thyroxine; TSH, thyroid stimulating hormone; PRL, prolactin; LH, luteinising hormone; FSH, follicle-stimulating hormone; GH, growth hormone; IGF-1, insulin-like growth factor-1
| Hormones |
Deficiencies in acute phase (n) |
Recovery in follow up evaluation (n) |
Persistent deficiencies in follow up (n) |
New onset deficiencies in follow up (n) |
Overall hormone deficiencies remaining at the end of the study (n) |
|---|---|---|---|---|---|
| TSH (mU/L) | 0 | 0 | 0 | 1 | 1 |
| FSH/LH (U/L) | 3 | 3 | 0 | 0 | 0 |
| ACTH (pg/ml) | 18* | 14 | 4 | 2 | 6# |
| GH (ng/ml) | 7© | 5 | 2 | 5 | 7# |
In this study, the hormone patterns at initial evaluation were typical of acute illness, characterised by hyperactivity of the hypothalamic-pituitary axis leading to raised PRL and cortisol, low T3 and testosterone and normal to raised TSH and LH18,19. The pattern of pituitary hormone deficiencies at follow up in our study resembles neuro-endocrine dysfunction seen following TBI and SAH20,21. Generally, in TBI, somatotrophs are commonly involved, followed by gonadotrophs, while in SAH, somatotrophs followed by corticotrophs are involved the most22,23. Somatotroph and gonadotroph axis were the most commonly affected in survivors of fatal cardiac arrhythmia11. This partial loss of anterior pituitary functions after vascular events has been reported extensively24. Individuals with CHB usually are elderly with multiple comorbidities and multiple complaints25. Hypopituitarism with varied and non-specific symptomology can add to impaired quality of life in the elderly26. Individuals with untreated GHD have higher BMI and increased cardiovascular risk factors, which tend to increase morbidity in them27, 30. So, the questions that remain unanswered and open for further research are: (i) Should individuals with CHB be evaluated for hypopituitarism, and if yes, (ii) should GH be indicated for treatment? GH replacement therapy has been tried in both healthy as well as GH-deficient elderly individuals with mixed results in some studies31 and beneficial effects in others32.
This study did have some specific limitations. First, we did not investigate cortisol insufficiency related to critical illness in our study participants during the acute phase evaluation, nor did we conduct any dynamic testing to explore this further. It is worth noting that the ACTH stimulation test can yield false negative results within the initial four weeks after ACTH deficiency onset, as the adrenal glands initially retain their responsiveness to externally administered ACTH15. Furthermore, we did not measure serum ACTH levels, which could have provided valuable information. Additionally, the GST we used is not the preferred method for assessing cortisol reserve due to its approximate eight per cent false positive rate compared to the insulin tolerance test33. To avoid overestimating ACTH deficiency, we chose to apply the lowest reported threshold for diagnosing cortisol insufficiency based on the GST16. Moreover, the inclusion of a control group matched for age, sex and comorbidities would have strengthened our findings. Regarding GHD, our study revealed that 28.5 per cent of the participants had low IGF-1 levels during the initial evaluation. It is important to consider the possibility of age-related decline in the GH-IGF-1 axis (somatopause) in these individuals, irrespective of the presence of heart block. However, it is important to note that we only conducted a single dynamic test for diagnosing GHD. Last, our study was limited by small sample size, lack of sample size calculation, relatively short follow up duration and the potential confounding effect of BMI on GH dynamics.
Overall, our findings suggest that a substantial number of previously undetected cases of hypopituitarism could be uncovered in individuals with CHB if our results are replicated in future studies. However, to validate these findings, it is crucial to conduct cross-validation studies involving larger sample sizes, including a healthy comparator group and have a longer duration of follow up.
Acknowledgment
We acknowledge the support of Dr Imtiyaz Ahmad and Altaf Ahmad in sample processing.
Financial Support & Sponsorship
The study was supported by Institutional Research Grant (Grant number: SIMS/ACAD/185) from Sher-I-Kashmir Institute of Medical Sciences, Srinagar, India.
Conflict of Interest
None.
Use of Artificial Intelligence (AI)-Assisted Technology for manuscript preparation
The authors confirm that there was no use of AI-Assisted Technology for assisting in the writing of the manuscript and no images were manipulated using AI.
References
- Hypothalamopituitary dysfunction following traumatic brain injury and aneurysmal subarachnoid hemorrhage: A systematic review. JAMA. 2007;298:1429-38.
- [Google Scholar]
- The GH-IGF-I axis and the cardiovascular system: Clinical implications. Clin Endocrinol (Oxf). 2008;69:347-58.
- [Google Scholar]
- Pathophysiology of hypopituitarism in the setting of brain injury. Pituitary. 2012;15:2-9.
- [Google Scholar]
- Animal models of neuroinflammation secondary to acute insults originated outside the brain. J Neuro Res. 2018;96:371-8.
- [Google Scholar]
- The central nervous system cytokine response to global ischemia following resuscitation from ventricular fibrillation in a porcine model. Resuscitation. 2009;80:249-52.
- [Google Scholar]
- The proinflammatory cytokine response following resuscitation in the swine model depends on the method of VF induction. Acad Emerg Med. 2008;15:939-44.
- [Google Scholar]
- Evaluation of long-term pituitary functions in patients with severe ventricular arrhythmia: A pilot study. J Endocrinol Invest. 2014;37:1057-64.
- [Google Scholar]
- Frequency of cardiac rhythm abnormalities in a half million adults. Circ Arrhythm Electrophysiol 2018:e006273.
- [Google Scholar]
- American Association of Clinical Endocrinologists and American College of Endocrinology Disease State Clinical Review: Update on growth hormone stimulation testing and proposed revised cut-point for the glucagon stimulation test in the diagnosis of adult growth hormone deficiency. Endocr Pract. 2016;22:1235-44.
- [Google Scholar]
- Calculation of mean arterial pressure during exercise as a function of heart rate. Appl Human Sci. 1995;14:293-5.
- [Google Scholar]
- Hormonal replacement in hypopituitarism in adults: an endocrine society clinical practice guideline. J Clin Endocrinol Metab. 2016;101:3888-921.
- [Google Scholar]
- Growth hormone and cortisol secretion in the elderly evaluated using the glucagon stimulation test. Endocrine. 2017;56:317-24.
- [Google Scholar]
- Metabolic Abnormalities, Inflammatory Markers and Endothelial Dysfunction in Hyperprolactinemia due to Prolactinoma before and after Normalisation of Serum Prolactin: A Prospective Case Control Study. Indian J Endocrinol Metab. 2023;27:357-364.
- [Google Scholar]
- Novel insights into the neuroendocrinology of critical illness. Eur J Endocrinol. 2000;143:1-13.
- [Google Scholar]
- Guidelines for the diagnosis and management of critical illness-related corticosteroid insufficiency (CIRCI) in critically ill patients (Part I): Society of Critical Care Medicine (SCCM) and European Society of Intensive Care Medicine (ESICM) 2017. Intensive Care Med. 2017;43:1751-63.
- [Google Scholar]
- High risk of hypopituitarism after traumatic brain injury: a prospective investigation of anterior pituitary function in the acute phase and 12 months after trauma. J Clin Endocrinol Metab. 2006;91:2105-11.
- [Google Scholar]
- High risk of pituitary dysfunction due to aneurysmal subarachnoid haemorrhage: A prospective investigation of anterior pituitary function in the acute phase and 12 months after the event. Clin Endocrinol (Oxf). 2007;67:931-7.
- [Google Scholar]
- American association of clinical endocrinologists and American college of endocrinology disease state clinical review: A neuroendocrine approach to patients with traumatic brain injury. Endocr Pract. 2015;21:823-31.
- [Google Scholar]
- Pituitary dysfunction after aneurysmal subarachnoid hemorrhage: a systematic review and meta-analysis. Neurosurgery. 2016;79:253-64.
- [Google Scholar]
- Clinical, hormonal and radiological features of partial Sheehan’s syndrome: An Indian experience. Arch Endocrinol Metab. 2016;60:125-9.
- [Google Scholar]
- Pacemaker therapy in very elderly patients: Survival and prognostic parameters of single centre experience. J Geriatr Cardiol. 2019;16:880-84.
- [Google Scholar]
- Excess Mortality associated with hypopituitarism in adults: a meta-analysis of observational studies. J Clin Endocrinol Metab. 2015;100:1405-11.
- [Google Scholar]
- Detection of premature atherosclerosis by high-resolution ultrasonography in symptom-free hypopituitary adults. Lancet. 1992;340:1188-92.
- [Google Scholar]
- Metabolic changes and vascular risk factors in hypopituitarism. Horm Res. 1992;38:68-72.
- [Google Scholar]
- Insulin resistance, metabolic syndrome and chronic low grade inflammation in Sheehan’s syndrome on standard replacement therapy: A case control study. Pituitary. 2015;18:312-8.
- [Google Scholar]
- Prevalence of coronary calcium deposits in Sheehan’s syndrome patients on long term replacement treatment. Pituitary. 2022;25:92-99.
- [Google Scholar]
- GH replacement therapy in elderly GH-deficient patients: A systematic review. Eur J Endocrinol. 2011;164:657-65.
- [Google Scholar]
- Baseline characteristics and effects of growth hormone therapy over two years in younger and elderly adults with adult onset GH deficiency. J Clin Endocrinol Metab. 2006;91:4408-14.
- [Google Scholar]
- How should we interrogate the hypothalamic-pituitary-adrenal axis in patients with suspected hypopituitarism? BMC Endocr Disord. 2016;16:36-8.
- [Google Scholar]






