Translate this page into:
An unusual case of phthiriasis palpebrarum with common itchy eyes
* For correspondence: lcwchina800@jlu.edu.cn
-
Received: ,
This article was originally published by Wolters Kluwer - Medknow and was migrated to Scientific Scholar after the change of Publisher.
A five year old girl† was admitted to the department of Ophthalmology, The First Hospital of Jilin University, Jilin, P.R. China, in November 2019, with a history of repeated episodes of redness and itching for more than two months in both her eyes. Her mother informed that she had been diagnosed with allergic blepharoconjunctivitis one month ago; however, the symptoms were not relieved with the anti-allergic medications.
On examination, visual acuity was 20/20 and intraocular pressure was normal in both eyes. Slit-lamp examination revealed mild bilateral conjunctival hyperaemia (Figure A). Several adult crab-like lice partially buried into the eyelid skin were found (Figure B). Moreover, there were multiple red dotted pinpoint lesions adhering to the eyelid skin in both her eyelids (Figure C). On further examination, lice infestation was not found in other hair-bearing skins, such as the eyebrows and the scalp hairs. The girl’s mother was also examined, and no lice infestation was noted. She also denied any significant medical history in her husband. Sexually transmitted diseases and child abuse were excluded. The diagnosis of phthiriasis palpebrarum was made. Lice were mechanically removed after instillation of topical anaesthesia with 0.4 per cent oxybuprocaine hydrochloride eye drop (Figure D). No lice and recurrence was found after one week of follow up.
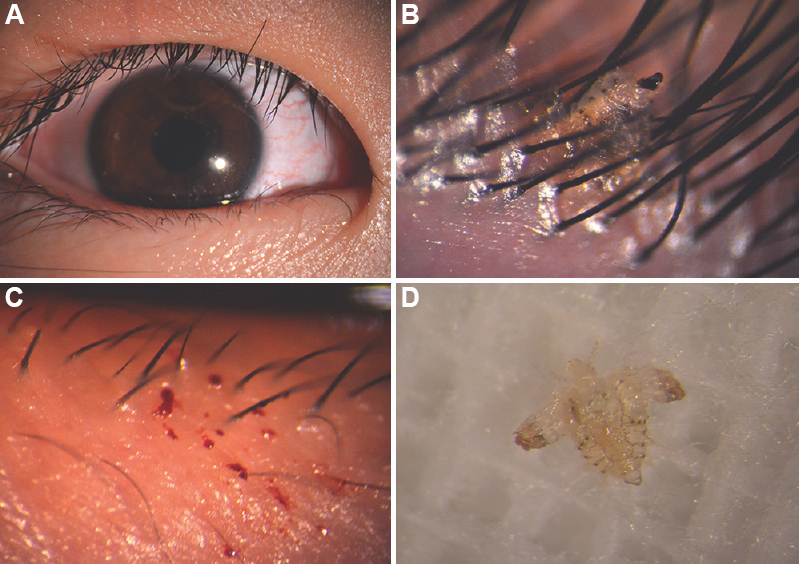
- Slit-lamp examination of phthiriasis palpebrarum. (A) Mild conjunctival congestion. (B) Louse were partially buried into the eyelid skin. (C) Multiple red pinpoint lesions. (D) Louse body after it was mechanically removed.
Hence, careful ocular examination should be done in cases with ocular itching and redness, to rule out phthiriasis palpebrarum, which is often misdiagnosed as allergic blepharoconjunctivitis.
Acknowledgment
This work was supported by grants by the National Natural Science Foundation of China (Grant No. 81800828).
Conflicts of Interest: None.





