Translate this page into:
Advances in management of locally advanced cervical cancer
For correspondence: Dr Sushil Beriwal, Department of Radiation Oncology, Allegheny Health Network Cancer Institute, 314 E. North Avenue, Pittsburgh, PA 15212, USA. e-mail: sushilberiwal@gmail.com
-
Received: ,
This article was originally published by Wolters Kluwer - Medknow and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Globally, cervical cancer has the fourth highest cancer incidence and mortality in women. Cervical cancer is unique because it has effective prevention, screening, and treatment options. This review discusses the current cervical cancer advances with a focus on locally advanced cervical cancer. Topics discussed include diagnostic imaging principles, surgical management with adjuvant therapy and definitive concurrent chemoradiotherapy. Emphasis is given on current advances and future research directions in radiation therapy (RT) with an emphasis on three-dimensional brachytherapy, intensity-modulated RT, image-guided RT, proton RT and hyperthermia.
Keywords
Chemotherapy
hyperthermia
image-guided brachytherapy
intensity-modulated radiation therapy
locally advanced cervical cancer
proton therapy
Introduction
Globally, cervical cancer has the fourth highest cancer incidence and mortality in females. This burden is disproportionately higher in limited-resource areas such as Sub-Saharan Africa and South-Eastern Asia1. Cervical cancer is unique because it has effective prevention, screening, and treatment options. In this review current advances in cervical cancer are discussed with a focus on locally advanced cervical cancer.
Updated FIGO staging for cervical cancer
In 2018, the International Federation of Gynaecology and Obstetrics (FIGO) updated cervical cancer staging guidelines with some major changes2. In FIGO stage I disease, stage IA no longer includes a lateral size extension criteria, and in stage IB, three distinct subgroups were included: IBI, IB2 and IB3 for diameters of ≥5 mm to <2 cm, ≥2 to <4 cm and ≥4 cm, respectively. In an important paradigm shift, imaging and pathological findings can now be used for staging to determine tumour size, tumour extent and involvement of retroperitoneal lymph nodes. Consequentially, FIGO stage III disease now includes stage IIIC1 and IIIC2 for involved pelvic or para-aortic lymph nodes, respectively2.
Diagnostic studies
In addition to history and physical examination, imaging plays a vital role in the assessment of the cervical cancer staging which ultimately determines management options. Imaging is a useful adjunct in determining the primary tumour extent and the spread of metastatic disease.
Evaluation of primary disease: Currently, magnetic resonance imaging (MRI) is the standard of care for primary tumour staging, but there is growing evidence for ultrasound. In a systematic review, pelvic MRI sensitivity for parametrial invasion and regional lymph nodes was 74 and 60 per cent, whereas pelvic computed tomography (CT) had sensitivity of 55 and 43 per cent, respectively3. The specificity of MRI and CT for parametrial invasion and lymph node involvement were similar at about 80 and 90 per cent. The sensitivity of MRI was high for the detection of rectum and bladder invasion3. In the ACRIN 6651/GOG 183 intergroup study, MRI was found to be superior to CT or clinical examination for assessing pathological tumour size, but none of these imaging modalities were found to accurately predict the extent of cervical stromal invasion4. The European Society of Urogenital Radiology guidelines recommend pelvic MRI to evaluate the local extent of disease and lymph node involvement5.
With significant barriers to MRI implementation in limited-resource areas, and recent advancements in ultrasound technology, there has been a renewed interest in ultrasound-based staging. In a single institution based study for early-stage cervical cancer, trans-rectal ultrasound was found to have comparable accuracy in detecting parametrial invasion and superior accuracy in detecting tumour volume6. In a prospective multi-institutional trial, ultrasound demonstrated increased accuracy compared to MRI for assessment of residual tumour and parametrial invasion and comparable accuracy for evaluation of deep stromal invasion and tumour size7. A recent meta-analysis demonstrated equivalent outcomes in regard to parametrial invasion8.
Evaluation of metastatic disease: Pelvic and para-aortic lymph node involvement is associated with worse prognosis29. The most recent FIGO staging2 now denotes the prognostic importance of these nodes as stage IIIC1 and IIIC2, respectively.
In a meta-analysis by Selman et al10, sentinel node biopsy showed higher accuracy than imaging. Historically, surgical staging was performed for locally advanced cervical cancer patients due to combined analysis of Gynecologic Oncology Group (GOG) 85, 120 and 165 which demonstrated that pre-treatment surgical staging before pelvic chemoradiation (CRT) resulted in an improvement in disease-free survival (DFS) and overall survival (OS)11. However, a positron emission tomography (PET)/CT randomized trial of 61 patients demonstrated a worse progression-free survival (PFS) and OS for pre-treatment surgical staging after initial clinical staging by CT or MRI12. In ACRIN6671/GOG 0233 trial, PET-CT versus CT demonstrated a borderline significant increase in the detection of abdominal lymph node metastasis13. When using ultrasound to examine lymph nodes, it has demonstrated a poor sensitivity14.
In a meta-analysis comparing various imaging modalities for accurate detection of metastatic lymph nodes, PET/CT demonstrated 82 per cent sensitivity and 95 per cent specificity in patient-based analysis, performing better than CT or MRI15. In a prospective randomized trial, the combination of PET/CT with MRI increased the detection of extra-pelvic lymph nodes and resulted in modified radiotherapy fields16. However, in PET/CT imaging, the false-negative rate for para-aortic lymph nodes was between 12 and 22 per cent depending on the involvement of pelvic lymph nodes17. Patients without involvement of the pelvic lymph nodes had a false-negative rate of about 10 per cent17. For patients without involvement of the pelvic lymph nodes, the additional toxicity of surgical or RT management likely does not justify the benefit of treatment intensification. However, patients with the involvement of pelvic nodes had a false-negative rate between 20 and 25 per cent17. This has significant clinical consequences for CRT target delineation and planning. Currently, there are three management options in this situation: pre-treatment surgical sampling, RT field covering one level above positive pelvic lymph nodes or inclusion of para-aortic lymph nodes in the radiation field, especially in patients with >2 pelvic nodes involvement18. The early results of uterus-11 multicentre phase III intergroup trial comparing radiographic treatment versus pre-treatment surgery have demonstrated an acceptable increase in grade 2 anaemia and leucocytopenia for surgical staging19. A clinical trial (NCT01365156), investigating the role of extra-peritoneal para-aortic lymph node dissection before CRT, has accrued and primary results are awaited.
Definitive chemoradiation
Definitive CRT is the standard of care for cervical cancer patients with FIGO IIB-IVA disease. Multiple studies have demonstrated an improvement of OS with the addition of cisplatin-based therapy at the cost of increased acute gastrointestinal (GI) toxicity and myelosuppression and no increase in late toxicities202122. For patients with FIGO stage IB3 and IIA2, surgery can be considered, but definitive CRT is preferred due to the high rate of adjuvant RT for tumours >4 cm23. The current standard of care is definitive CRT incorporating concurrent weekly or triweekly cisplatin with external beam radiation therapy (EBRT) and brachytherapy (BT) boost24.
Definitive IMRT: As discussed above, IMRT has been shown to improve outcomes in cervical cancer patients. Gandhi et al25 randomized a total of 44 patients with intact cervix to conventional three-dimensional (3D) radiation versus IMRT and demonstrated a decrease in grade ≥2 acute GI toxicities and less chronic GI issues. The multi-institutional phase II INTERTECC-2 trial used IMRT to spare bone marrow and reduce dose to GI organs-at-risk (OAR)26. A subset of the trial used an optional PET/CT to delineate functional bone marrow for contouring in order to help reduce myelosuppression. Compared to historical norms, IMRT decreased grade ≥3 neutropenia and clinically significant GI toxicity. The use of PET/CT for contouring of bone marrow has also decreased the risk of grade ≥3 neutropenia26.
Another benefit of IMRT is the ability to perform simultaneous integrated boost (SIB) to involved pelvic and para-aortic lymph nodes. When delivering 45 Gy in 25 fractions to the whole pelvis and prophylactic lymph nodes, an SIB of 55.0-57.5 Gy to involved nodes has resulted in a high level of complete response at three month PET/CT27. This technique (SIB) is now adopted by many centres for patients with involved lymph nodes (Fig. 1). The current EMBRACE II study is assessing IMRT/image-guided radiation therapy (IGRT) for cervical cancer patients and incorporates SIB for involved lymph nodes28.
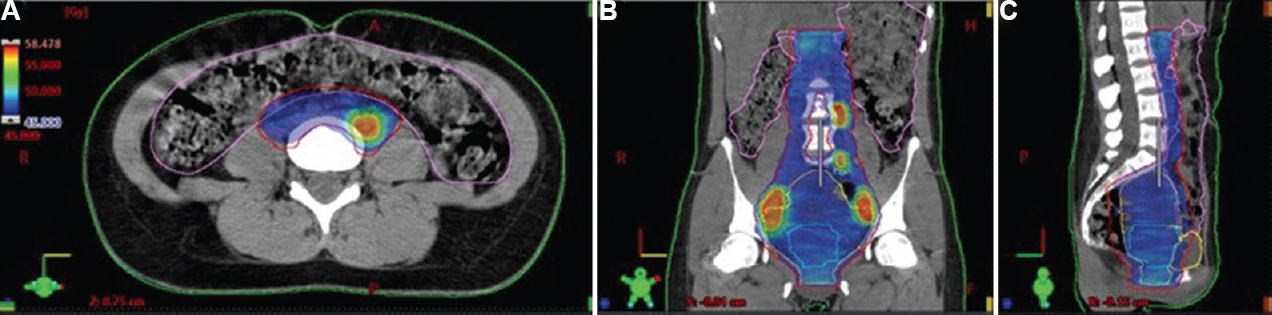
- Volumetric modulated arc therapy treatment plan for a FIGO stage IIIC1 cervical carcinoma patients with involved lymph node simultaneous integrated boost (prescription dose 45 Gy, nodal SIB 57.5 Gy, 25 fractions). (A) Axial computed tomography view of the para-aortic region with involved nodal boost. Isodose colour wash as shown in dose level legend. (B) Coronal computed tomography view of extended field radiation therapy. (C) Sagittal computed tomography view of extended field radiation therapy.
Image-guided radiation therapy (IGRT): With the ability of IMRT to deliver highly conformal radiation to target areas and minimize dose to OARs, the importance of IGRT cannot be overstressed29. Multiple studies have examined the inter-fraction movement of the uterus, cervix, vaginal and other target areas30. This movement can result in the GTV/CTV being under dosed or OARs being overdosed31. The position of cervix, uterus, bladder and rectum can therefore vary on daily setup. As a result, the successful delivery of IMRT is highly dependent on the ability to account for this variability in motion. The most common techniques to correct for motion are patient preparation/positioning methods, CTV/ITV margins32, cone-beam CT (CBCT) or fiducial markers. The most commonly used IGRT system is CBCT33. Daily CBCT has been shown to result in acceptable setup variation with reduced planning target volume (PTV) margins and thereby allow successful delivery of radiotherapy to the CTV while avoiding OAR33.
Proton radiation therapy: Improvements in patient-reported outcomes (PROs) with advanced photon-based modalities have generated interest to test the hypothesis if proton beam therapy (PBT) could help further maximize outcomes in gynaecological cancer. Initial approaches utilized proton therapy as a boost in patients not eligible for BT. An initial Japanese experience of 25 patients with cervical cancer that used proton boost to achieve a median of 86 Gy demonstrated local control (LC) at five years ranging from 100 per cent for stage IIB and 61 per cent for stage IIIB/IVA patients with a 10 yr survival of 89 and 40 per cent, respectively34. Modern PBT technique of intensity-modulated proton therapy (IMPT) has been shown to result in superior cumulative doses to target and OAR when compared to volumetric modulated arc therapy (VMAT)-based stereotactic boost3536. However, even most modern PBT techniques such as IMPT cannot match the dose escalation with BT which therefore continues to remain the standard of care for locally advanced cervical cancer37.
Most of the research has focussed on exploring PBT as an alternate to photon based EBRT. Dosimetric studies have demonstrated a significant dose reduction to small and large bowel, despite maintaining excellent dose distribution to the target volume. This benefit is especially notable when treating the para-aortic nodal chains where PBT also reduces dose to the kidneys and spinal cord36373839. In a dosimetric study comparing IMPT and IMRT plans, even in the worst case scenarios accounting for range and set up uncertainties, IMPT resulted in 20-40 per cent improvement in various dosimetric parameters related to functional bone marrow (V5 Gy, V10 Gy, V20 Gy and V40 Gy)40. Since whole pelvic RT can induce premature menopause in young patients, a dosimetric study41 evaluated ovarian-sparing IMPT in comparison to VMAT (Fig. 2). In this study, all the IMPT plans and only 40 per cent of VMAT plans were able to achieve a Dmean to the ovary less than 15 Gy while meeting appropriate target coverage41.
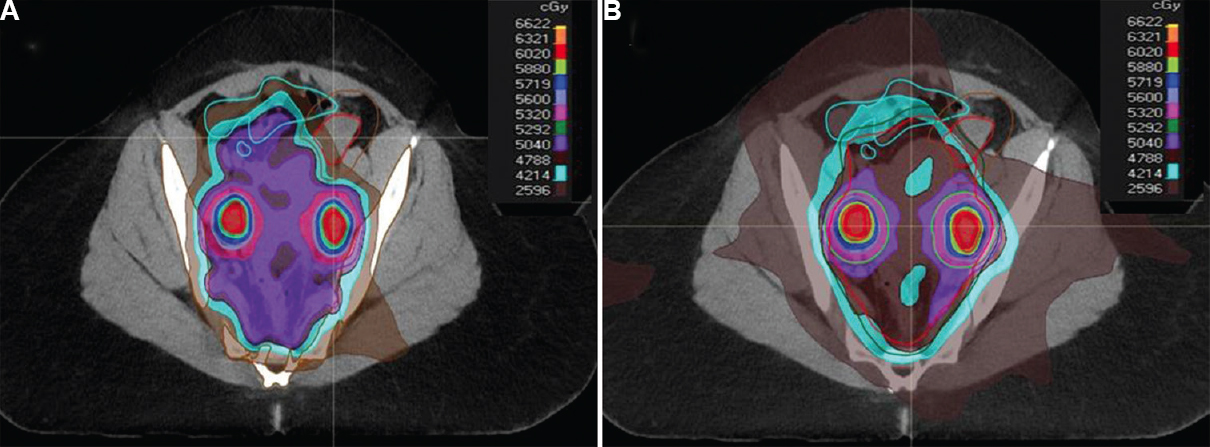
- Ovarian sparing radiotherapy (prescription dose 50.4 Gy, nodal boost 60.2 Gy, 28 fraction simultaneous integrated boost). (A) Intensity-modulated proton therapy plan with pencil beam scanning technique, mean ovarian dose 20 Gy, small bowel V15 Gy = 120 cc and V45 Gy = 10 per cent, bone marrow V20 Gy = 64 per cent, V40 Gy = 22 per cent. Isodose colour wash as shown in dose level legend. (B) Volumetric modulated arc therapy plan, mean ovarian dose 30 Gy, small bowel V15 Gy = 196 cc and V45 Gy = 12 per cent, bone marrow V20 Gy = 78 per cent, V40 Gy = 29 per cent.
There are emerging clinical data to support the use of proton therapy for gynaecological malignancies. A clinical study reported results for 11 women who were treated with pencil beam scanning IMPT following hysterectomy for gynaecologic cancers42. Toxicity profile was favourable with only one grade 3 acute GI toxicity and no grade 3 or higher genitourinary toxicity. Ongoing efforts are trying to elucidate the role of PBT in patients with post-operative uterine or cervical cancers through prospective studies (NCT03184350)43. Future research is required to validate long-term oncological outcomes of PBT in large patient population compared to IMRT-based approaches.
Systemic chemotherapy with radiation therapy: In GOG 12022, six cycles of weekly 40 mg/m2 cisplatin during CRT had equivalent OS to cisplatin/5-fluorouracil/hydroxyurea22, and Lanciano et al44 demonstrated the benefit of cisplatin alone versus 5-fluorouracil alone. To date, there has not been a trial comparing cisplatin alone with cisplatin and 5-fluorouracil. A total dose of greater than 200 mg cisplatin has been demonstrated to increase DFS45. A phase II trial examining weekly cisplatin versus three weekly cisplatin demonstrated improved OS and decreased grade 3 and 4 neutropenia, leading to a phase III TACO trial (NCT01561586) comparing these regimens46. Two meta-analyses have demonstrated an improvement in OS, PFS and locoregional relapse for cisplatin-based doublet regimens compared to weekly cisplatin4748. Another area of systemic therapy intensification is seen in the phase III NRG-GY006 trial (NCT02466971) investigating the addition of triapine, a ribonucleotide reductase inhibitor which works as a radiosensitizer, to the standard concurrent cisplatin RT with a primary end point of OS. A phase II trial by Dueñas-Gonzálex et al49 demonstrated that concurrent and adjuvant gemcitabine/cisplatin versus standard concurrent cisplatin in combination with RT, resulted in improved PFS, OS and time to progression at the cost of increased grade 3 and higher toxicities from 46.3 to 86.5 per cent. The implementation of this protocol was limited by the concerns over treatment toxicity in addition to lack of clarity if the observed benefits were from the concurrent and/or adjuvant component of doublet chemotherapy49.
Adjuvant chemotherapy: Following definitive CRT, most patients with locally advanced cervical cancer achieve complete response. However, locoregional or distant recurrence is noted in 30 per cent of patients50. Three prior randomized controlled trials (RCTs) investigating adjuvant chemotherapy following definitive CRT showed conflicting results495152. Two of these studies showed significant OS benefit with the addition of adjuvant chemotherapy4951. The experimental arms in these studies varied in that they used either combination chemotherapy for CRT followed by adjuvant chemotherapy49 or neoadjuvant chemotherapy followed by CRT plus adjuvant therapy51. These factors made it challenging to establish the incremental benefit resulting from the addition of adjuvant chemotherapy to the control arm (concurrent cisplatin radiotherapy). In an RCT by Tangjitgamol et al52 standard cisplatin CRT was compared with definitive CRT followed by three cycles of adjuvant paclitaxel and carboplatin in patients with stages IIB-IVA cervical cancer. This study was stopped early due to futility. At a median follow up of 27.4 months, there was no significant improvement in PFS or OS52. OUTBACK (NCT01414608) and INTERLACE (NCT01566240) studies testing the addition of adjuvant and neoadjuvant chemotherapy to definitive CRT might help answer questions relating to benefit with additional systemic therapy.
It has been shown that the persistence of human papilloma virus (HPV) positivity following definitive CRT is associated with worse local DFS and OS53. Therefore, detectable HPV DNA following CRT is a potential biomarker that can help select patients for adjuvant therapy. An ongoing Chinese RCT is investigating whether adjuvant chemotherapy (4 cycles of docetaxel and nedaplatin) can reduce recurrence rate and improve relapse-free survival (RFS) compared with observation in patients with persistent HPV after CRT/RT(ChiCTR-IIR-17012655).
Brachytherapy (BT)
Image-guided brachytherapy: Image-guided brachytherapy (IGBT) is the gold standard in the definitive management of locally advanced cervical cancer. IGBT evolved from the (GYN) GEC-ESTRO working group, where clinicians from European IGBT centres standardized prescribing and reporting MRI-based IGBT. The GEC-ESTRO recommendations I-IV54555657 have since been used as a framework for the implementation of IGBT and are incorporated into the recent International Commission on Radiation Units and Measurements (ICRU) 89 report28. These guidelines address the importance of optimal tumour and OAR nomenclature, MRI-based delineation, dosimetry and standardized reporting of results. To evaluate the impact of MRI-based IGBT, GEC-ESTRO has launched two studies. The first study (EMBRACE-I) prospectively examined the role of MRI-based IGBT following CRT58. On the other hand, retroEMBRACE was a retrospective study evaluating outcomes of patients treated with IGBT before the launch of EMBRACE-I study59.
Two-dimensional versus three-dimensional BT planning: In the French STIC multicentre prospective study that compared 2-dimensional (2D) low-dose-rate or pulsed dose rate (PDR) cervix BT with 3D PDR BT (mainly CT based), three different treatment regimens were defined60. In group 3, patients received CRT followed by BT. At 24 months, local RFS was better in the 3D cohort (73.9 vs. 78.5%, P=0.003)61. At the same time, a significant reduction was noted in the 3D cohort wth respect to two-year grade 3-4 GU/GI toxicity (Group 3; 22.7 vs. 2.6%, P=0.02)61.
Sturzda et al59 reported the outcomes of retroEMBRACE study which included 731 women treated with IGBT following EBRT ± chemotherapy. About 40.5 per cent had lymph node involvement and 50.4 per cent had FIGO stage IIB disease. Mean EBRT dose was 46.0±2.5Gy. Majority received concomitant chemotherapy (77.4%). MRI-based IGBT was used in 80.9 per cent, and combined intracavitary/interstitial approach was used in only 23.0 per cent. The mean high-risk clinical target volume (HRCTV) was 37±24 cm3, and the mean D90 (dose to 90% of the target) for HRCTV was 87±15 Gy. Mean HRCTV D90 decreased with advancing stage. The five-year actuarial local control (LC), pelvic control (PC), cancer-specific survival (CSS) and OS were 89, 84, 73 and 65 per cent, respectively. Five-year grade 3-5 GU, GI and vaginal toxicity was five, seven and five per cent, respectively. When compared to historical control, improvement in LC and PC was associated with OS and CSS benefit of around 10 and 14 per cent, respectively59. The improvement in PC was seen across all the stages, with the greatest absolute benefit seen among stage IVA patients59. Unfortunately, the improvement in OS was similar across all stages and not proportional to the benefit seen in PC due to the competing risk of systemic disease59.
Although MRI is the gold standard for IGBT, widespread applicability is challenging in resource-limited settings. To overcome uncertainties associated with CT-based contouring, IBS-GEC-ESTRO ABS has recently proposed new consensus guidelines to facilitate accurate CT-based contouring and reliable prescription and reporting of radiotherapy dose62.
New benchmark for outcomes: EMBRACE-I is a multicentre, prospective, observational international study in which patients with stage IB-IVA or IVB restricted to para-aortic nodes were treated with chemoradiotherapy (weekly cisplatin and 45-50 Gy external beam radiotherapy using 3D conformal RT or IMRT), followed by MRI-based IGBT58. Around 25 per cent of the patients had stage III-IV disease. Actuarial five-year LC for the entire group was 92 per cent, and it was >90 per cent for stage III and stage IV disease. The five-year cumulative incidence of grade 3-5 GU, GI and vaginal toxicity were 6.8, 8.5 and 5.7 per cent, respectively. This has set a new benchmark for the management of locally advanced cervical cancer58.
Factors affecting local control (LC): RetroEMBRACE has shown that following three factors were associated with worse LC following IGBT: higher HRCTV volume, lower HRCTV D90 and increase in overall treatment time (OTT)63. A HRCTV D90 of ≥85 Gy delivered in seven weeks, resulted in a three-year LC >90 per cent for small-sized (HRCTV <20 cm3) and intermediate-sized targets (HRCTV 20-30 cm3), while it was >86 per cent for large targets (HRCTV up to 70 cm3). Further dose escalation from 85 Gy to 90-95 Gy could potentially improve LC by 1-4 per cent based on tumour size63. An increase in OTT by one week beyond the optimal time of 49 days was equivalent to a HRCTV D90 decrease of 5 Gy, while an increase in HRCTV volume by 10 cm3 could be overcome by an increase of HRCTV D90 by 5 Gy to achieve an equivalent LC at three years63.
In a study from University of Pittsburgh Medical Center (UPMC)64 evaluating outcomes in 239 women following five fractions of MRI-based IGBT, the five-year LC was 90.5 per cent. On multivariate analysis, adenocarcinoma histology and patients with HRCTV >40 cm3 had the worst LC, despite D90 to HRCTV being >85 Gy64. In summary, dose escalation could not fully compensate for unfavourable tumour biology.
Patterns of failure: In retroEMBRACE study, at a median follow up of 43 months, disease progression was noted in 30 per cent and the predominant pattern of failure was systemic (systemic failure: 17%, pelvic failure: 6%, both pelvic and systemic: 7%)65. This was in contrast to conventional BT studies, where the most common location of failure was pelvis (systemic failure: 9-12%, pelvic failure: 16-17%, both pelvic and systemic: 7-13%)66. Among patients that progressed in the retroEMBRACE study, 20.7, 56.8 and 22.5 per cent had isolated pelvic failure, distant failure and combined pelvic and distant failures, respectively65. These reports highlight the need for effective regimens to control micro-metastases and in turn improve survival outcomes.
Node-positive patients had higher rates of regional failure (8.2 vs. 3.0%, P=0.0002), paraaortic nodal (PAN) relapse (10.2 vs. 6.4%, P=0.001) and distant failure (27.05 vs. 14.7%, P<0.0001) when compared to node-negative patients65. Other factors associated with local, regional, and systemic failure included MRI primary tumour size ≥5 cm, non-squamous histology and high-risk group (stage III-IVA or node-positive patients). Majority of these failures (85.2%) occurred within the first three years following treatment completion, 40-50 per cent occurring within the first year65.
In EMBRACE-I study, the five-year LC, PC, DFS and OS were 92, 87, 68 and 74 per cent respectively58. The five-year nodal control in node-negative and node-positive patients was 93 and 81 per cent, respectively58.
Hybrid brachytherapy (BT): A modified ring applicator allows the implantation of interstitial needles (IS) in parallel with the intrauterine tandem. From anatomical point of view, each additional needle in the ring applicator can increase the coverage by 10 mm in the lateral direction which corresponds to medial parametrium. Introduction of these applicators have facilitated higher conformality in dose distributions, especially in tumours with significant parametrial extension, eccentric tumours, or large tumours. Another advantage with these hybrid applicators is a reduction in the dose to OARs while maintaining adequate target coverage. Overall, institutions with IC/IS expertise have reported using hybrid applicator in approximately 40-50 per cent of BT patients67.
In EMBRACE-I study, use of IC/IS was associated with a significant improvement in target doses while reducing the dose to OAR68. In retroEMBRACE, systematic use of IC/IS led to an increase in HRCTV D90 from 83±14 Gy to 92±13 Gy. The three-year LC rate of patients with HRCTV >30 cm3 was 10 per cent better in the IC/IS group when compared to intracavitary applicator (P=0.02). This was not accompanied by an increase in late toxicity.
Rectal, bowel, bladder, ureteral and vaginal morbidity: In EMBRACE-I study, acute and late toxicities were scored using the CTCAEv3.0 criteria. Rectal morbidity report from EMBRACE-1 has suggested that the risk of late grades 1-4 rectal toxicity was 20.1, 6.0, 1.6 and 0.1 per cent, respectively. Dosimetric analysis has shown that D2 cm3 <65 Gy was associated with two times lower risk of proctitis when compared to D2 cm3 ≥65 Gy (P=0.032). D2 cm3 ≥75 Gy was associated with a 12.5 per cent risk of rectal fistula when compared to 0-2.7 per cent for patients with a rectal D2 cm3 <75 Gy (P>0.001)69. EMBRACE-I study has also reported a 5.9 per cent actuarial late grade 3-4 bowel toxicity, with a 2.6 per cent incidence of late stenosis/stricture/fistula70. Grade 1-2 toxicity was most prevalent, with diarrhoea and flatulence being the most common toxicities70. Grade 1-2 bowel incontinence gradually worsened with time. In PROs, diarrhoea and difficulty controlling bowel movements gradually worsened with time70. In a recent report from EMBRACE-I, the following CRT factors were associated with grade 2 or higher diarrhoea: 50 Gy EBRT dose versus 45 Gy, V43 Gy >3000 cc, V57 Gy ≥165 cm3 (lymph node boost) and para-aortic nodal RT. Rectum D2 cm3 >70 Gy and V60 Gy >288 cm3 were also associated with a higher risk of grade 2 or higher diarrhoea71.
In EMBRACE-I study, the crude incidence of grade 2 or higher urinary fistula, bleeding and cystitis was 0.7, 2.7 and 88 per cent, respectively. Approximately 16 and 14 per cent of patients reported significant pain and difficulty in voiding, respectively. A higher bladder D2 cm3 was associated with a high risk of grade 2 or higher cystitis (13% at 80 Gy and 8% following 75 Gy)72. The crude incidence of grade 2 or higher urinary frequency and incontinence was 13 and 11 per cent respectively. A higher ICRU bladder point dose was associated with higher risk of urinary incontinence (11 vs. 20% for point dose of <65 Gy vs. >75 Gy)73.
At five years, actuarial grade 3-4 ureteral stricture from EMBRACE-I study was 2.1 per cent. Advanced tumour stage with hydronephrosis at diagnosis was the only factor associated with the increased risk of grade 3-4 ureteral stricture74. In a recent MRI-based IGBT study, the estimated risk of developing grade 3 or higher ureteral stenosis in patients without pre-existing hydronephrosis was 4.4 per cent. Dose to 0.1 cm3 of ureter greater than 77 Gy was noted to correlate with high grade ureteral stenosis75.
In a report from EMBRACE-I study evaluating vaginal toxicity in 630 patients, the two-year actuarial estimate for grade ≥2 vaginal stenosis was 21 per cent. Factors associated with grade ≥2 vaginal stenosis were rectovaginal reference point dose, EBRT dose higher than 45 Gy in 25 fractions and tumour extension into the vagina76. The estimated risk of grade ≥2 toxicity was 20, 27 and 34 per cent for rectovaginal reference point doses of 65, 75 and 85 Gy, respectively. One way of achieving this dosimetric constraint was by reducing the ring loading during BT to 33 per cent, thereby reducing the dose to ICRU rectovaginal reference point. The lack of standardized reporting of vaginal EBRT doses makes it difficult to compare dosimetric constraints across different studies. As a result a new dose reporting system with reference to posterior inferior border of pubic symphysis has been recommended in EMBRACE II77.
Recently, EMBRACE-I has reported the incidence of late substantial treatment-related patient-reported symptoms (LAPERS) in 1047 patients treated with IGBT78. LAPERS events were defined as the presence of substantial EORTC symptoms (quite a bit/very much) for at least half of the assessments (persistence) and progression beyond baseline condition (treatment-related). The median proportion of patients with LAPERS events was 4.6 per cent, with rates of urinary frequency, neuropathy, menopausal symptoms, insomnia, and fatigue greater than 10 per cent78.
Response assessment: 18F-fluorodeoxyglucose (FDG) PET-CT is used widely to assess disease response following definitive CRT and IGBT. Initial reports indicated incomplete metabolic response in up to 20-30 per cent of patients. Schwarz et al79 have shown that patients with incomplete metabolic response have worse CSS and PFS when compared to those with a complete response on PET-CT. Kalash et al80 evaluated the role of diffusion-weighted MRI (DW-MRI) in patients with residual PET-positive disease following completion of definitive treatment. In these patients, 81.8 per cent with positive DW-MRI had histologically confirmed local progression80. In patients with negative DW-MRI, only 12.5 per cent developed local recurrence. Patients with positive DW-MRI also had worse two-year OS (36 vs. 83%, P=0.049)80. This makes DW-MRI an ideal imaging modality to evaluate disease status in patients with positive PET-CT.
Ongoing studies and advances in IGBT: EMBRACE II is an interventional and observational multicentre study that intends to demonstrate high levels of local, regional and systemic control while minimizing morbidity28. This study uses sophisticated EBRT and BT contouring protocols, standardized dose prescription and advanced EBRT (IMRT and IGRT) and BT (IC/IS) techniques. This study has translational research component incorporating imaging and tissue biomarkers. Relevant dose constraints for both CRT component and IGBT are explained in detail in EMBRACE II protocol28.
Another technical advance in IGBT is the introduction of Venezia applicator (Elekta, Sweden), which allows additional degree of freedom by permitting insertion of a second row of needles parallel/oblique to the first row of needles on Vienna applicator. This improves the conformity of prescription doses to disease within the lateral parametrium while sparing adjacent OARs. A study using this applicator has shown encouraging dosimetric results81. A recent study from University of Pittsburgh Medical Center has reported complete imaging response at three months in 85 per cent of locally advanced cervical cancer patients treated using hybrid applicators (Vienna/Venezia). In this study, despite stage IV disease in four per cent, grade 3 or higher GU/GI toxicity was limited to only 5.7 per cent82.
Antiangiogenic agents
In cervical cancer, HPV influences angiogenesis via p53 inhibition and hypoxia-inducible factor-1α stabilization83. These factors ultimately result in the increased expression of vascular endothelial growth factor (VEGF), resulting in increased vascular permeability and endothelial cell proliferation83. GOG 240 is a two-by-two factorial phase III study that examined the efficacy and toxicity of two factors: non-platinum chemotherapy and bevacizumab84. This study showed that addition of bevacizumab to chemotherapy was associated with improvement in OS (17.0 vs. 13.3 months, P=0.004), PFS and response rate84. This study also identified vaginal fistula as a unique toxicity along with the known bevacizumab-related toxicities such as hypertension, proteinuria and venous thromboembolism. Incidence of grade 3 or higher rectovaginal/vesicovaginal fistula in the bevacizumab arm was six per cent, and this only occurred in patients with prior pelvic radiation. Bevacizumab in combination with platinum-based doublet is now a national comprehensive cancer network (NCCN) category 1 recommendation for recurrent/metastatic cervical cancer84.
CIRCCa is a phase II randomized clinical trial that tested addition of cediranib (oral VEGFR1-3 TKI) to paclitaxel/carboplatin85. This study was closed early due to cediranib shortage. Cediranib improved PFS (8.1 vs. 6.7 months, P=0.032) at the cost of increased grade ≥3 toxicities such as diarrhoea, hypertension and febrile neutropenia85.
Immunotherapy
Cytotoxic T lymphocyte associated antigen 4 (CTLA-4) inhibitor: CTLA-4 regulates T-cell activation amplitude and prevents overstimulation of the immune system. Ipilimumab, a fully humanized IgG1K antibody, was the first immune check point inhibitor that was approved for the treatment of melanoma86. In a multicentre study of metastatic cervical cancer patients that had progressed through first-line platinum agent, single agent ipilimumab failed to show significant response87.
Radiotherapy may initiate anti-tumour response that kills clonogens distant to the primary target, a rare phenomenon known as abscopal effect. GOG 9929 is a phase I trial of sequential ipilimumab following concurrent chemoradiotherapy for locally advanced cervical cancer patients including those with positive para-aortic lymph nodes. Initial report demonstrated a one-year DFS of 74 per cent88. Maximum tolerated dose of ipilimumab was 10 ml/kg, and no major late toxicities were reported88.
PD-1 and PDL-1 inhibitors: Programmed death-1/programmed cell death ligand-1 (PD-1/PDL-1) signalling activation suppresses T-cell mediated immune response in the peripheral tissues to decrease effector T-cell responses89. During homoeostasis, this process protects tissues from immune-mediated damage, also known as immune tolerance. The interaction between PD-1/PDL-1 results in the suppression of T-cell proliferation, migration and secretion of cytotoxic mediators and inhibits cell killing89. Therefore, inhibitors of PD-1 and PDL-1 reverse suppression of T-cells and increase anti-tumour activity. PD-1/PDL-1 pathway can be targeted by molecules specific for either PD-1 (nivolumab, pembrolizumab) or PDL-1 (avelumab, durvalumab and atezolizumab)89.
The results of phase 2 KEYNOTE-158 Cohort E study led to pembrolizumab being approved for PDL1–positive cervical cancer patients following first-line chemotherapy. Overall response rate in PDL-1–positive (>1% expression) was 14.6 per cent, and in this subset, 91 per cent of patients experienced a durable response90. A phase I/II study of nivolumab in recurrent or metastatic HPV-associated cancers including cervical cancer has shown an overall response rate of 26.3 per cent91. There are multiple ongoing phase II studies investigating PD-1/PDL-1 blockade for locally advanced cervical cancer (NCT02635360 and NCT03612791) in the concurrent and adjuvant setting.
Radiotherapy and hyperthermia in cervical cancer
Therapeutic hyperthermia (HT) involves artificial increase in tissue temperature to 40-44°C, which, in addition to causing direct cytotoxicity of cancer cells, results in impaired repair of radiation damage to cellular DNA, resulting in radiosensitization92. Improved regional blood flow further helps to improve radiotherapy response in hypoxic tumours93. The role of HT in the management of gynaecological cancers continues to be unclear due to mixed results shown in randomized studies.
In the Dutch Deep Hyperthermia Trial, 114 patients with locally advanced cervical cancer were randomized to radiotherapy with or without weekly HT. At 12 yr follow up, addition of HT resulted in nearly 20 per cent improvement in LC (37 vs. 56%, P=0.01) and 17 per cent improvement in survival (20 vs. 37%, P=0.03) without any increase in grade 3 or higher toxicity94. In the International Atomic Energy Agency multi-institutional randomized study with 110 patients, no improvement in LC or survival was seen with the addition of weekly HT to RT without chemotherapy95. A paradoxical detriment was seen in stage IIB disease. Increase in acute grade 2-3 toxicity was also reported without any change in late toxicity95.
The RADCHOC randomized trial attempted to test CRT versus HRT in cervical cancer patients96. The study was closed prematurely due to poor accrual with 87 out of planned 376 patients revealing comparable event-free survival (primary end point), pelvic recurrence-free survival and OS in the two arms. Subsequently, a Japanese multicentre study evaluated CRT versus CRT + HT in patients with stage IB (bulky)-IVA cervical cancer97. Among 101 patients, the addition of HT resulted in improved complete response rates (88 vs. 77.6%, P=0.047). Though an improvement in five-year OS and DFS was noted, this was not significant97.
Interstitial HT has also been evaluated in patients undergoing interstitial brachytherapy for cervical cancers. In a randomized trial, however, additional interstitial HT did not result in improved oncological outcomes98. Some institutions add interstitial HT to high-dose rate interstitial brachytherapy in patients with locally advanced cancers with any one of the three factors: bulky disease at presentation, poor response or in the recurrent/re-irradiation setting.
Future directions
Microbiome: There has been a substantial interest in the role of the microbiome in cervical cancer99100. Multiple studies have demonstrated increased bacterial diversity in HPV-infected patients, a prerequisite in most cases for cervical cancer development101102. The rate of HPV clearance has been shown to be associated with certain microbiome compositions102. Furthermore, cancer treatment for gynaecological malignancies was shown to affect the vaginal microbiome103. In a study of cervical, rectal and sigmoid cancer patients, the administration of probiotics concurrent with RT decreased grade ≥3 radiation-induced diarrhoea and decreased daily bowel movements104. The microbiome therefore appears to be an attractive area that can be explored in future cervical cancer studies.
Cervical cancer genome: The role of HPV, E6 and E7 in cervical cancer is well established105. In 2017, the Cancer Genome Atlas Research Network performed a genomic and molecular analysis of cervical cancer106. This has revealed three distinct genomic/molecular subtypes in cervical cancer: keratin-low squamous, keratin-high squamous and adenocarcinoma-rich clusters. These three subgroups have unique molecular/protein alterations that could serve as potential targets for future therapeutics. Overall, the phosphoinositide-3-kinase, mitogen-activated protein kinase (PI3K-MAPK) and transforming growth factor beta (TGFβ) signalling pathways were altered in more than 70 per cent of cervical cancers thereby representing potential targets106. Further research into these subtypes may lead to better risk stratification and targeted therapies.
Financial support & sponsorship: None.
Conflicts of Interest: SB is the Assistant Medical Director of Elsevier Clinical Pathways Via Oncology, XOFT DSMB and is an employee of Varian.






