Translate this page into:
A validation study of early warning system in high-risk pregnant women
For correspondence: Dr Reena Rani, Department of Obstetrics & Gynecology, NDMC Medical College & Hindu Rao Hospital, Malka Ganj, Delhi 110 007, India e-mail: dr.reena0310@gmail.com
-
Received: ,
This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
This article was originally published by Wolters Kluwer - Medknow and was migrated to Scientific Scholar after the change of Publisher.
Abstract
High-risk obstetric patients have chances of deterioration which can be detected by any early warning score. This study was aimed to assess the suitability of the Obstetrics National Early Warning System (ONEWS) for the pregnant women. This prospective study was conducted on 500 high-risk pregnant women attending a tertiary care teaching hospital. The ONEWS charts were plotted for each of them. The primary outcome measure was composite adverse maternal outcome (CAMO) in the form of one or more among mortality, severe maternal morbidity and intensive care unit admissions. Of the 500 women who participated, 200 (40%) had a score ≥3 (triggered an intervention). The CAMO among the triggered group [59.5% (n=119)] was significantly higher compared to that in the non-triggered group [13.3% (n=40) (P=0.001)]. The area under the receiver operating characteristic curve was 0.800 (95% confidence interval 0.752-0.847). The sensitivity of the ONEWS in predicting CAMO was 74.8 per cent, specificity 76.2 per cent, positive predictive value 59.5 per cent and negative predictive value 86.7 per cent at a cut-off score of 3. ONEWS appears to be a useful tool for predicting adverse maternal outcomes in high-risk pregnant women.
Keywords
Adverse maternal outcomes
early warning score
high-risk pregnancy
physiological parameters
severe maternal morbidity
Patients at a risk of rapid deterioration and critical illness often have preceding changes in their physiological parameters. Identifying such patients at an early stage using a simple protocol, based on physiological parameters may avoid maternal mortality. An early warning system (EWS) uses physiological parameters to track a patient's condition, detect deterioration early and trigger an increased level of care1. An EWS has three components: (i) Early warning score - a tool to aid the recognition and management of a pregnant women whose condition is deteriorating; (ii) Tracking - periodic observation and recording of physiological parameters on an observation chart; and (iii) Trigger - predetermined cut-off score will trigger the summoning of help, involving a timely response and an appropriate level of assistance1.
A variety of EWSs have been developed in non-obstetric adult populations, but none of these are validated for the obstetric population. Normal physiological changes during pregnancy may alter the significance of physiological parameters, and thus, application of these scores in pregnancy may need modification. The Confidential Enquiry into Maternal and Child Health UK Report 2003-2005 recommended the routine use of the modified early obstetric warning system2. There is a paucity of literature regarding the use of EWS in pregnant Indian women. Although many EWSs3456 have been described, the Obstetric National Early Warning System (ONEWS)7 used in Wales, UK, based on 10 physiological parameters for bedside evaluation in pregnant women was found suitable in the Indian context. The objective of this study was to validate and assess the suitability of ONEWS7 in high-risk pregnant Indian women.
This was a prospective observational study conducted at the department of Obstetrics and Gynecology, Maulana Azad Medical College and associated Lok Nayak Hospital, New Delhi, India, from October 2013 to April 2015. By assuming the prevalence of composite adverse maternal outcome (CAMO) as about 20 per cent, the minimum risk for CAMO was expected to be 2.5 times higher for a particular predictor (odds ratio 2.5)8. Further, assuming alpha and beta error as 5 and 10 per cent, respectively, to account for many confounders, multiple correlation coefficient was assumed to be 0.489. With these values, a sample size of about 500 (exactly 482) was required to get the predictors for CAMO.
The inclusion criteria were any pregnant women during pregnancy or within 42 days of delivery or termination of pregnancy who had any one or more of the following: high-risk pregnant woman admitted from obstetrics and gynaecology emergency, had undergone surgery within the last 24 h, and was already admitted in obstetrics ward and became sick. The women admitted directly to the intensive care unit (ICU) were excluded. The study protocol was approved by the Institutional Ethics Committee, and informed written consent was obtained from all participants. After a complete clinical evaluation, ONEWS7 was administered at the time of admission to the hospital.
The frequency of tracking was decided by the total score on admission. Women with a total score of 0-2 were monitored 12 hourly, a score of 3-5 every 2-4 hourly, a score of 6-8 every 1-2 hourly and with a score of ≥9 were continuously monitored with multiparameter monitor. These women were followed up until discharge from the hospital. The outcome measured was CAMO which included occurrence of one or more among severe maternal morbidity, ICU admission and maternal death. Severe maternal morbidity included those women with organ dysfunction who survived10.
The mean age was 26.03±3.82 yr; 61.8 per cent (n=309) were multiparous, 58 per cent (n=290) were literate and 86 per cent (n=430) belonged to a low socio-economic status. The incidence of severe maternal morbidity was 49.7 per cent in illiterate women. Of the 488 antenatal women, 336 delivered during the study period. Among the 500 women, 325 were booked while 175 were unbooked. CAMO was found in 61 (34.85%) unbooked and in 98 (30.15%) booked women.
CAMO was observed in 159 of 500 (31.8%) women. Of these, the incidence of CAMO was 22 of 158 (13.9%) women who had score of zero, 17 of 142 (11.9%) women who had score of 1-2, 44 of 111 (39.6%) women who had score of 3-4, 66 of 74 (89%) women who had score of 6-8 and 10 of 15 (66%) women who had with score of ≥9.
The area under receiver operating characteristic (AUROC) curve is shown in the Figure. The sensitivity of the ONEWS in predicting CAMO was 74.8 per cent, specificity 76.2 per cent, positive predictive value 59.5 per cent and negative predictive value 86.7 per cent at a cut-off score of 3. The AUROC for ONEWS in our study (0.80, 0.95% CI 0.752-0.847) was lower as compared to the results of other studies456, which ranged from 0.937 to 0.995. Out of 159 women in which CAMO was observed, major obstetric haemorrhage was observed in 29 (18%), pre-eclampsia/eclampsia in 96 (62.7%), renal dysfunction in 13 (8.49%), liver dysfunction in 14 (9.1%), cardiac arrest in seven (4.5%), pulmonary oedema in six (3.9%), acute respiratory dysfunction in five (3.2%), cerebrovascular event in one (0.65%), septicaemic shock in two (1.3%) and massive pulmonary embolism in three (1.9%) women.
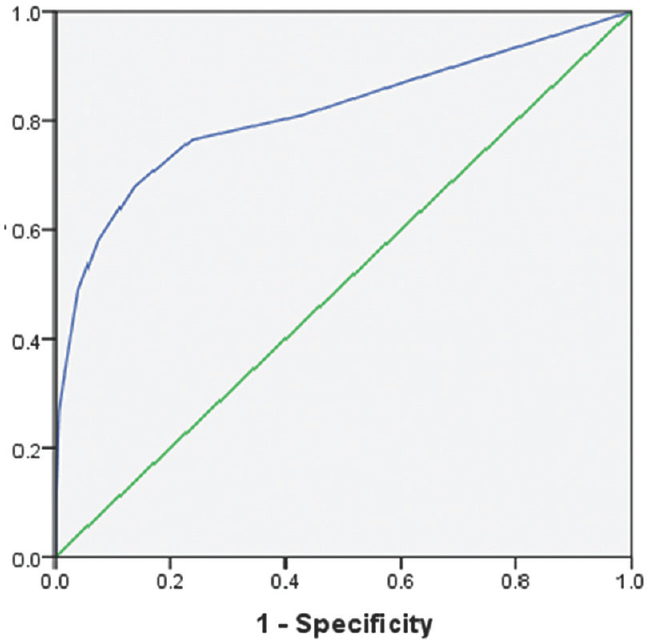
- ROC curve and corresponding AUC. ROC curves typically feature true-positive rate (sensitivity) on the Y-axis and false-positive rate (1-specificity) on the X-axis for different cut-off points of a parameter. The area under ROC curve was 0.800 (95% CI 0.752-0.847). The sensitivity of the ONEWS in predicting adverse maternal outcome was 74.8 per cent, specificity 76.2 per cent, positive predictive value 59.5 per cent and negative predictive value 86.7 per cent using a cut-off score of 3. Diagonal segments are produced by ties. ROC, receiver operating characteristic; AUC, area under the curve; CI, confidence interval; ONEWS, Obstetrics National Early Warning System.
The Table shows the distribution of patients according to trigger parameter and the relative risk of severe maternal morbidity with each parameter. The most frequent triggers were diastolic blood pressure (BP), followed by systolic BP and tachycardia, as reported earlier8. The relative risk for oxygen saturation, urine output and urinary protein was higher in our study as compared to the study by Singh et al8. The Scottish Confidential Audit10 of severe maternal morbidity revealed major obstetric haemorrhage as the most common severe maternal morbidity (5.0/1000 live birth), which was similar to (2.9/1000 live birth) our study. The most common cause of maternal death in our study was obstetric haemorrhage as compared to study conducted by Saravanakumar et al11, with the most common cause of maternal death being cardiac disease.
| Trigger parameter | Number of patients (%) (n=500) | Severe maternal morbidity (%) | P | Relative risk of severe adverse morbidity (95% CI) |
|---|---|---|---|---|
| Systolic BP >140 mmHg | 220 (44) | 90 (40.9) | <0.001 | 3.32 (2.2-5.0) |
| Diastolic BP >90 mmHg | 235 (47) | 98 (41.7) | <0.001 | 3.38 (2.2-5.0) |
| Pulse >100/min | 67 (13.4) | 28 (41.7) | <0.05 | 1.76 (1.0-2.9) |
| Respiratory rate >20/min | 16 (3.2) | 9 (56.2) | <0.05 | 3.02 (1.1-8.2) |
| Temperature >37.5°C | 12 (2.4) | 9 (75) | <0.05 | 5.34 (1.6-17.6) |
| SpO2 <95% | 9 (1.8) | 8 (88.8) | <0.05 | 16.5 (2.0-135.6) |
| Looks/feels unwell | 32 (6.4) | 9 (28.1) | <0.05 | 6.6 (2.9-14.6) |
| Neurological status AVPU | 7 (1.4) | 7 (100) | <0.05 | 3.3 (2.9-3.8) |
| Urine output <1 ml/kg/h | 6 (1) | 5 (83.3) | <0.05 | 11.6 (1.34-100.3) |
| Urinary protein-yes | 96 (19.2) | 96 (100) | <0.05 | 19.3 (11.2-33.3) |
CI, confidence interval; BP, blood pressure; AVPU (A-alert, V-responding to verbal commands, P-responding to painful stimulus, U-unresponsive)
There were a total of 23 maternal deaths. The causes were obstetric haemorrhage in eight women, sepsis in six, anaemia and hypertensive disease of pregnancy in one each and others (embolism and anaesthetic problems) in seven (30.4%). All women who died had a score of ≥3.
The ICU admissions in the triggered group (n=200) was 10 per cent (n=20) and in the non-triggered group (n=300) was 4.3 per cent (n=13), with the difference being significant (P<0.01). Of the total 33 (6.6%) women who were transferred to ICU, 17 (51.5%) died. The mean length of hospital stay was 8.7±6.5 days.
The major limitation of our study was that this was a single-centre study and might suffer from population bias. In a resource-limited country like India, it is difficult to monitor every high-risk patient in the ICU. Development of a system which can be applied with simple bedside techniques without need of high cost and maintenance equipment and can be performed by junior doctors or nurses is relevant. It would facilitate early identification of sick women and is expected to result in the reduction in maternal mortality and morbidity12. To conclude, ONEWS may be used for predicting CAMO in high-risk pregnant women. Further research may be directed to increase sensitivity and specificity by lowering the threshold at which morbidity is defined.
Financial support & sponsorship: None.
Conflicts of Interest: None.
References
- Reproducibility of physiological track-and-trigger warning systems for identifying at-risk patients on the ward. Intensive Care Med. 2007;33:619-24.
- [Google Scholar]
- The Confidential Enquiry into Maternal and Child Health (CEMACH) In: Lewis G, ed. Saving Mothers' Lives: reviewing maternal deaths to make motherhood safer - 2003-2005. The Seventh Report on Confidential Enquiries into Maternal Deaths in the United Kingdom. London: CEMACH; 2007.
- [Google Scholar]
- The patient-at-risk team: Identifying and managing seriously ill ward patients. Anaesthesia. 1999;54:853-60.
- [Google Scholar]
- Design and internal validation of an obstetric early warning score: Secondary analysis of the intensive care national audit and research centre case mix programme database. Anaesthesia. 2013;68:354-67.
- [Google Scholar]
- National early warning score (NEWS): Standardizing the assessment of acute illness severity in the NHS. Report of a working party. Available from: https://www.rcplondon.ac.uk/file/32/downloadhttp://www.rcpiondon.ac.uk/resources
- A national survey of obstetric early warning systems in the United Kingdom. Int J Obstet Anesth. 2009;18:253-7.
- [Google Scholar]
- A validation study of the CEMACH recommended modified early obstetric warning system (MEOWS) Anaesthesia. 2012;67:12-8.
- [Google Scholar]
- Quantifying severe maternal morbidity: A Scottish population study. BJOG. 2004;111:481-4.
- [Google Scholar]
- High dependency care in an obstetric setting in the UK. Anaesthesia. 2008;63:1081-6.
- [Google Scholar]
- A physiologically-based early warning score for ward patients: The association between score and outcome. Anaesthesia. 2005;60:547-53.
- [Google Scholar]






