Translate this page into:
A scoping review on the errors in medical certification of the cause of death in India
For correspondence: Dr Divya Khanna, Department of Preventive Oncology, Mahamana Pandit Madan Mohan Malaviya Cancer Centre and Homi Bhabha Cancer Hospital, Tata Memorial Centre, Varanasi 221 005, Uttar Pradesh & Homi Bhabha National Institute, Mumbai 400 094, Maharashtra, India e-mail: dkhannakgmc@gmail.com
-
Received: ,
Abstract
Medical certification of the cause of death provides epidemiological information for developing cause-specific mortality and disease trends, guiding the monitoring of health programmes and allocating health resources. Therefore, providing correct information on the cause of death is essential. This study describes the errors in medical certification of the cause of death in India. We conducted a scoping review through a systematic inquiry in four databases, PubMed, ProQuest, Google Scholar and EBSCO, for all published articles reporting errors in medical certification of cause of death in India between December 31, 1998 and December 31, 2020. The review outcomes were the proportion of major and minor certification errors reported. Out of 135 screened studies, 20 were included based on the eligibility criteria. We observed a high proportion of certification errors and a large proportion of variation. Major certification errors were in the form of incorrect underlying cause of death (8.5-99.2%) and incorrect chain of events leading to death (12-64.7%). Minor certification errors in the form of missing clerical details, abbreviations and illegible handwriting were 0.3-100 per cent. The proportion of incomplete death certificates ranged between 12-100 per cent. Absence of time intervals was the most common type of certification error (62.3-99.5%). Training of doctors to accurately certify the medical cause of death and its addition to medical education is urgently needed to ensure accurate information for mortality-related statistics. A uniform methodology for auditing and reporting errors in medical certification of cause of death should be adopted.
Keywords
Audit
cause of death
curriculum
death certificate
ICD-10
mortality
training programmes
A death certificate (DC) is a medico-legal record stating the medical cause, time, place and manner of an individual’s death. The medical certification of cause of death (MCCD) provides epidemiological information for developing cause-specific mortalities and disease trends. Policymakers require this information to prioritize health and research resources distribution, and monitor the impact of health programmes1,2. The effects of DCs on families, learning programmes, health-related policies, monitoring, research and indicators are substantial3,4.
Geographical coverage of mortality registration ranges from nearly 100 per cent in Europe to ∼50 per cent in Asia-Pacific, and less than 10 per cent in Africa5. In India, only 20 per cent of deaths are registered, and 50-60 per cent of the registrations are incorrect4,6. The time series data on MCCD in India (1991-2015) demonstrates a significant but gradual increase in the frequency of medically certified cases. During this period, the proportion of registered deaths that were medically certified fluctuated between 12.7 to 22 per cent. In addition, since all deaths do not occur in hospitals, hospital-based mortality statistics cannot reflect the actual scenario. Hence, the verbal autopsy is used in the sample registration system7.
It is not uncommon to find MCCD having errors due to illegible handwriting, incompletely filled certificates, incorrect medical causes and manners of death. Despite poor medical certification status in India, less importance is given to teaching death certification in undergraduate medical courses8. However, several studies have reported certification errors in MCCD from different parts of India. A comprehensive review of all these published studies that can report the burden and pattern of certification errors is still lacking. With this background, we aimed to describe the status of MCCD in India regarding the proportion and types of certification errors reported in previous Indian studies and the methodology adopted by these studies for identifying errors in death certification.
Material & Methods
Literature search methodology
We conducted a systematic inquiry in four databases, namely PubMed, ProQuest, Google Scholar and EBSCO, with the MeSH and free text words such as ‘cause of death’ or ‘medical cause of death certificate’ or ‘death registration’ or ‘death audit’ or ‘death certification’ or ‘hospital deaths’ or ‘vital statistics’ or ‘quality of death certificates’ or ‘validation of cause of death’ or ‘death certificate’ and ‘India’, published between December 31, 1998 and December 31, 2020. We did not attempt to search for any unpublished data. The bibliography list of all included studies was also cross-referenced to ensure a full literature search. Authors of the articles for which full text was not accessible online were requested, and the full text thus obtained was included in this inquiry.
Eligibility criteria
Criteria for inclusion
This study included published investigations (in English) conducted on the cause of death (COD) certification in India and reported the frequency of certification errors.
Criteria for exclusion
Mortality studies from India that were not evaluating death certification errors were excluded such as knowledge, attitude and practice studies of the certifying physicians9, survival studies10, disease registry11, verbal autopsy-based studies12, 14 etc. Studies for which full text was not accessible and news or media reports that were not published in scientific journals were also excluded (Figure).
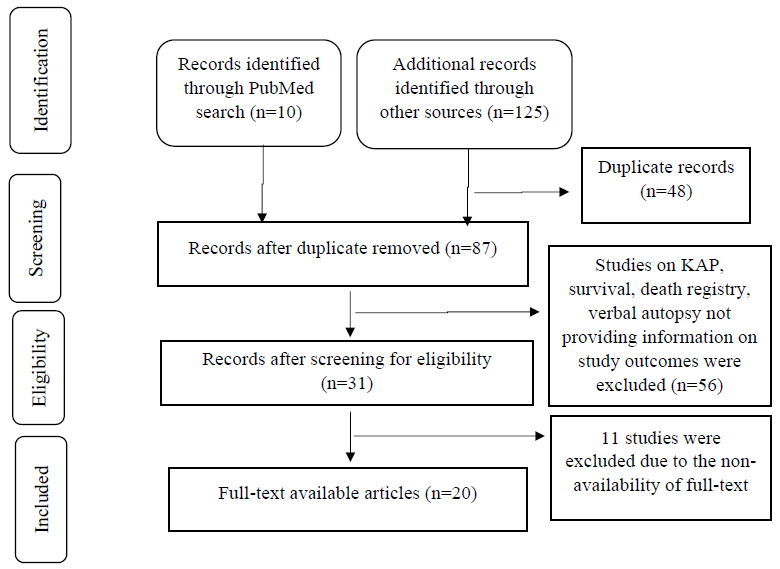
- PRISMA flowchart showing the process of articles selected for the review.
Article selection and data extraction
Articles/titles/abstracts with the keywords were screened by two independent investigators based on the defined eligibility criteria. Two researchers independently screened all headings, abstracts and full-text documents and resolved disagreements by consensus or consulting with the third researcher. Subsequently, information for the following was abstracted from the included studies: (i) place of study, (ii) study design, (iii) number of death certificates assessed, (iv) types and percentage of errors in MCCD, (v) completeness of the death certificate, (vi) methodologies adopted in the audit of death certificates.
Outcome measures
Definitions of cause of death
The World Health Organization (WHO) defines the cause of death (COD) in relation to writing MCCD15. The underlying cause of death (UCOD) is ‘the disease or the injury which initiated the train of morbid events leading directly to the death or the circumstances of the accident or violence that produced the fatal injury’15. Immediate cause of death (ICOD) is ‘disease or condition directly leading to death’15. Antecedent cause of death is ‘morbid conditions, if any, giving rise to the immediate cause of death’15. Contributory conditions are ‘all other diseases or conditions believed to have unfavourably influenced the course of the morbid process and thus contributed to the fatal outcome but which were not related to the disease or the condition directly causing death’15. Disease-related symptoms and modes of dying, such as cardiac and respiratory arrest, are not included in these definitions15.
The outcome measure was the proportion of certification errors reported in the included studies, which were categorized as major and minor based on the method of audit described by Myers and Farquhar16. Major errors were the errors that could influence the correct identification of the underlying cause of death, such as: (i) the mechanism of death or non-specific condition mentioned as an underlying cause of death, (ii) improper sequence of events leading to death, (iii) mentioning two or more causally unrelated, aetiology-specific diseases (competing causes) in part I of MCCD, and (iv) based on the clinical review of medical records it was found that the COD was not acceptable. Minor errors were: (i) use of abbreviations, (ii) absence of time-intervals in parts I and II of the MCCD, (iii) technical or clerical errors in the form of wrong or missing personal identifiers (age, gender and place of residence), incomplete certifying physician details, illegible handwriting and incomplete or wrong clerical details in the MCCD. Many studies reported incomplete information in part I and/or part II of the MCCDs. We categorized this as a major error (Table I)16.
| Type of error | Definition |
|---|---|
| Major errors | |
| Mechanism of death listed without an underlying cause | A mechanism or nonspecific condition is listed as the underlying cause of death |
| Improper sequencing | The sequence of events does not make sense; the underlying cause of death is not listed on the lowest completed line of part I |
| Competing causes | Two or more causally unrelated, etiologically specific diseases listed in part I |
| Unacceptable cause | Wrong cause of death based on the review of clinical records or any one of the above errors (either alone or in combination) |
| Incomplete MCCD | MCCD information in part I and/or II is incomplete |
| Minor errors | |
| Abbreviations | Abbreviations used to identify diseases |
| Absence of time intervals | No time intervals are listed in parts I or II |
| Mechanism of death followed by a legitimate underlying cause of death | Use of a mechanism but qualified by an etiologically specific cause of death |
| Technical or clerical errors | Mentioning wrong personal identifiers (such as age, gender, & place of residence), incomplete certifying physician details, illegible handwriting, and incomplete or wrong clerical details in the MCCD |
MCCD, medical certification of cause of death. Source: Ref.16
Data analysis
Data collected during the review was entered and analyzed using Microsoft Excel. Descriptive statistics in frequencies and proportions were reported for the outcome variables.
Results
A total of 135 studies were screened, and 20 studies6,8,17, 34, were included in the review based on the eligibility criteria. Studies for which the full text was not available (n=11) were excluded (Figure). The abstracted information from the included studies is mentioned in Table II.
|
Author/yr/ place of study |
Study design | Sample size | Key findings | Type of study setting & qualifications of the certifying doctors |
|---|---|---|---|---|
|
Patel et al6 (2017); Madhya Pradesh |
Observational | 53 death certificates | Not a single certificate was error-free. The immediate, antecedent, & underlying cause of death were inaccurate in 79.2, 75.5, & 67.9% of DCs, respectively | Tertiary teaching medical college. Physicians’ qualification NA, Ward setting details NA |
|
Pandya et al8 (2009); Gujarat |
Interventional: The frequency of major & minor errors in death certificates was examined before & after conducting 3 workshops, each of 90 min, for the post-graduate residents | 198 death certificates | Significant decrease in major certification errors post-intervention | Tertiary teaching hospital. All clinical residents. Qualification & ward settings details NA |
|
Prakash et al17 (2010); Delhi |
Observational | 259 death certificates | 32% had an incorrect cause of death. Among these, 27% mentioned the mode of dying as COD | Referral oncology center with surgical, radiation, medical, & palliative oncology doctors. Qualification & ward settings details NA |
|
Agarwal et al18 (2010); Gujarat |
Observational | 296 death certificates | In 86% of DCs, the immediate cause of death was mentioned as a mode of death | Tertiary teaching hospital. Qualification & ward settings details NA |
|
Patel et al19 (2011); Gujarat |
Observational | 45 death certificates | Not a single certificate was error-free. Major errors in 57.5% DCs. Minor errors in 92.5% of DCs. 80% of DCs reported mode of death as the immediate cause of death | Tertiary teaching hospital. Casualty, Intensive care unit, medical ward, & others (not specified), Qualification detail NA |
|
Shah et al20 (2012); Gujarat |
Observational | 3212 death certificates | Major errors: The accuracy of immediate cause, antecedent cause, & underlying cause was 44, 55, & 69.9%, respectively. Only 1.2% of the certificates were accurate | Tertiary health institute. Qualifications & ward settings details NA |
|
Lanjewar et al21 (2013); Not mentioned |
Observational | 229 death certificates | 58% of DCs were completely filled. Out of completely filled certificates, 82.7% had an accurate COD | Medicine & allied, surgery & allied, pediatrics, forensic medicine, obstetrics, & gynecology departments. Qualifications details NA |
|
Dash et al22 (2014); Odisha |
Observational | 151 death certificates | Major errors : The antecedent cause was filled in 27%, & the underlying cause was filled in only 0.8%. Most MCCD forms were incomplete (96.19%). Gender was missing in 45.7% | Tertiary care teaching institute. Qualifications & ward settings details NA |
|
Azim et al23 (2014); Uttar Pradesh |
Interventional; pre & post-intervention audit conducted for reporting death certification errors. The intervention included an interactive educational programme for residents training for super speciality | 150 death certificates | Significant decrease in major certification errors post-intervention | Tertiary care teaching institute. Resident doctors are undergoing subspecialty training in Critical Care Medicine. Ward setting details NA |
|
Ganasva et al24 (2015); Gujarat |
Observational | 1942 death certificates | Immediate, antecedent, & underlying causes were reported in 95.9, 27, & 0.8% of the DC, respectively. Only 1.1% were completely filled | Private practitioners from 12 wards of Municipal Corporation. Qualifications & ward settings details NA |
|
Pokale et al25 (2016); Maharashtra |
Observational | 98 death certificates | Two major errors were combined in 35.6% of DCs, three major errors in 8.6%, & at least one minor error in 99.3% of DCs. The most common error was the absence of a time interval (98.9%) | Tertiary care hospital. The majority are issued by the medicine department. Qualifications details NA |
|
Ahir et al26 (2018); Gujarat |
Observational | 523 death certificates | Only 20.1, 26.8, & 28.9% of MCCD forms were accurate in determining the immediate cause, antecedent cause, & UCOD | Tertiary care teaching hospital. Qualifications & ward settings details NA |
|
Uplap et al27 (2019); Maharashtra |
Observational | 410 death certificates | All DCs were incomplete & inaccurate. Mode of dying mentioned as immediate or antecedent cause of death in 86 & 41%, respectively. Multiple causes in 56% DCs | Tertiary care hospital. Resident medical officers. Qualifications & ward settings details NA |
|
Patil et al28 (2019); Maharashtra |
Observational | 278 death certificates | Completeness for the immediate, antecedent, & underlying cause of death was 99.7, 98.3, & 88%, respectively. Sequencing errors in 64.7%, Unacceptable COD in 37.8% | Tertiary care teaching hospital. Qualifications & ward settings details NA |
|
Sudharshan et al29 (2019); Tamil Nadu |
Interventional; pre- & post-assessment of accuracy in writing MCCD for case-based scenarios given before & after a lecture on writing MCCD. | 80 physicians | Significant decrease in major & minor certification errors post-intervention | Teaching hospital. Teaching faculty, post-graduates, junior residents, & interns (who have completed medicine & surgery postings). Ward setting not applicable |
|
Raje30 (2011); Maharashtra |
Observational | 353 death certificates | 19% of deaths were in the incorrect sequence. Multiple COD: 25%. Use of abbreviations: 68%. Illegible name & signature of certifying physician: 85% | The teaching hospital attached a Medical College. Qualifications & ward settings details NA |
|
Sheikh et al31 (2012); Telangana |
Observational | 156 death certificates | Modes of death reported as COD in 37.8 certificates | General Hospital. Medical doctors. Qualifications & ward settings details NA |
|
Gupta et al32 (2013); Chandigarh |
Observational | 1251 death certificates | Any error: 97.1% vs. 73.3% (P<0.05). Any major error: 61.9% vs. 45.0% (P<0.05). Any minor error: 96.5% vs. 92.6 (P<0.05) | Tertiary pediatric hospital. Qualifications details NA |
|
Srinivasulu et al33 (2014); Andhra Pradesh |
Observational | 110 death certificates | Not a single form was error-free 47% reported major errors, 21% minor errors | Rural medical college hospital. Qualifications & ward settings details NA |
|
Jain et al34 (2015); Gujrat |
Observational | 7392 death certificates | Only 2% of certificates were completely filled. Modes of death were COD in 82.2%. Completeness for the immediate, antecedent, & underlying cause was 95.56, 66.67, & 40%, respectively | Municipal Corporation’s Registrar Birth & Death office. The doctors’ qualifications are not accessible. Ward setting details NA |
DC, death certificate; COD, cause of death; NA, not available
Characteristics of the studies included
The included studies assessed a total of 17,106 DCs and the number of DCs covered in each study was in the range of 45 DCs19 to 7392 DCs34. Most of these studies were conducted in Gujarat State (7 studies)8,18, 20,24,26,34 followed by Maharashtra (4 studies)25,27,28,30 and the rest were from Delhi17, Chandigarh32, Uttar Pradesh23, Odisha22, Madhya Pradesh6, Andhra Pradesh33, Telangana31 and Tamil Nadu.29 Majority of the studies were observational (17 studies)6,17, 22,24, 28,30, 34 and three were interventional8,23,29. The interventional studies conducted death certification training for resident doctors and teaching faculty and assessed the effect on the post-intervention quality of death certification. All interventional studies reported a reduction in certification errors post-intervention. Interventions were in the form of seminars, training sessions and participatory workshops. One study29 provided case-based scenarios before and after intervention in the form of training on death certification and compared the certification errors for the case scenarios; these studies were conducted at tertiary care teaching hospitals6,8,18, 20, 22,23,25, 30,33 (Table II).
Major certification errors
The included studies reported substantial errors in the UCOD (8.5-99.2%), the ICOD (0.3-79.9%) and the chain or sequence of events preceding death (12-64.7%). Modes or mechanisms of death, such as cardiopulmonary arrest, were incorrectly mentioned as the COD in the range of 8.9-86 per cent. An unacceptable COD was reported in the range of 13.2-92.9 per cent (Table III)20, 36. Out of the 12 studies that evaluated the completeness of the DC, all but one reported a very high proportion of incompleteness in DCs (Table III)20, 36.
| Category | Number of studies describing the certification error | Proportion of errors (%) |
|---|---|---|
| Minor certification errors | ||
| Wrong personal identifiers21,24,25,29,30,31,32 | 7 | 0.3 - 100 |
| Incomplete certifying physician details20,23,24,27,28,32,35 | 7 | 0.5 - 64.2 |
| Use of abbreviations21,24,25,29,30,31,32 | 7 | 29.3 - 98 |
| Illegible handwriting21,24,30 | 3 | 15 - 52.3 |
| Absence of time intervals8,10,20, 21,22,24,25,26,27,29,30,31,34,35 | 14 | 62.3-99.5 |
| Incomplete/wrong clerical details in the MCCD22,29,30,32 | 4 | 2.7 - 100 |
| Major certification errors | ||
| Incorrect underlying cause of death8, 10,21,24,25,26,29,34,35 | 9 | 8.5 - 99.2 |
| Incorrect immediate cause of death8,20,24,26,29,30,32,35 | 8 | 0.3 - 79.9 |
| Incorrect chain/sequence of events8,10,21,25,32,34 | 6 | 12 - 64.7 |
| Modes of dying as a cause of death8,21,22,33,35 | 5 | 8.9 - 86 |
| Others (not acceptable cause of death)10,25,30 | 3 | 13.2 - 92.9 |
| Incompleteness of MCCD in part I & part II of MCCD21,22, 25,26,27,29,30,31,32,34,35,36 | 12 | 21-100 |
Minor certification errors
Missing time intervals for COD was the most reported certification error in the included studies (62.3-99.5%). Other reported errors were wrong personal identification (0.3-100%), incomplete certifying physician details (0.5-64.2%), abbreviations (29.3-98%) and illegible handwriting (15.0-52.3%) (Table III)20, 36.
Patterns of reporting certification errors
Death certification audit studies have been reported from only selected States in India, such as Gujarat, Maharashtra, Uttar Pradesh, Odisha, Tamil Nadu, Andhra Pradesh, Telangana, Delhi and Chandigarh. Published data for death certification errors was lacking from many other States.
We found that the pattern of reporting death certification errors was not uniform. The outcomes for reporting certification errors varied in the included studies (Tables II and III). We reviewed the included articles for their adopted methodologies to audit death certification. Ten studies described the standardized definitions or guidelines used for reporting certification errors6,8,20,21,23,26,30,32, 34. All studies except for four17,18,24,31 mentioned using the WHO-prescribed format for reporting the MCCD in their study settings. Eight studies mentioned reviewing the deceased’s medical records during the evaluation of MMCD8,17,18,22,24,32,33,34. Six studies described the process of MCCD in their study settings6,8,17,19,19,33. The conduction of training of reviewers for death certification was mentioned in six studies18,23,24,25,32,33. Two studies mentioned the independent reviewing of the DCs by two investigators and the method of resolving the disagreements in the death certification assessment8,32. Three studies assessed the International Classification of Disease (ICD-10) coding for the COD6,19,34. One study29 assessed certification errors in the case-based scenarios before and after intervention in the same training session.
Discussion
Globally, a more significant proportion of deaths are contributed by the low- and middle- income countries, which have weak COD registration systems and high death certification errors that potentially hinder establishing disease control priorities and evaluating the impact of existing health programmes35,36. We conducted a scoping review of studies reporting certification errors in MCCD in India between December 31, 1998 and December 31, 2020. This review describes the proportion and types of errors and the methodology adopted by these studies for identifying errors in death certification. As per authors’ knowledge, no other review existed that utilized the findings of the MCCD assessment studies across India to understand the burden and pattern of certification errors.
We identified large proportions of major and minor certification errors and wide variations in reporting the certification errors among the included studies. Researchers have reported similar observations working in other countries and with other sub-populations37, 39. This review detected 12 types of certification errors (6 major and 6 minor) in the included studies. The highest proportion of reported major certification errors was for incompleteness, where the MCCDs had incomplete information for part I and part II (21-100%), followed by inaccurate UCOD (8.5-99.2%) and not acceptable COD (13.2-92.9%); of the 12 studies examining the completeness regarding part I and part II of the MCCD majority reported a very high percentage of incompleteness. Incomplete DCs can affect the selection of the accurate UCOD, leading to an underestimation of the actual disease burden and affecting policy-making and resource allocation for prevention and control40. Checking the completeness of the MCCD as part of quality control and developing a tracking mechanism to ensure the completion of such incomplete MCCDs is required in every hospital setting39.
A global systematic review reported that the highest rates of wrong UCOD were reported in India and Pakistan39. UCOD initiates the chain of events leading to death and the most crucial COD from a public health perspective41. The correct identification of UCOD is a critical step for developing and monitoring strategies for diseases of public health importance. Additionally, an accurate UCOD is mandatory for completeness and accurate death registration reporting and comparison at national and international levels39. We observed that incorrectly assigning mechanisms/modes of death, such as cardio-respiratory arrest as a UCOD, ranged between 8.9 and 86 per cent. In line with this, the systematic review also reported that the highest rates of this error were reported in India and Greece39. Data regarding mechanisms of death are of no analytical value and may also cause ambiguity and misinterpretation of the COD. The ICD codes assigned for such CODs are often regarded as ‘garbage codes’ that are not useful for public health analysis. When such errors are large, it may often lead to bias in the actual mortality pattern42, 44. This form of certification error is a significant challenge in LMICs, where most deaths occur without any medical attention at the time of death35.
We observed that minor certification errors in the form of clerical mistakes in the personal information of the decedents ranged from 0.3-100 per cent. The included studies reported that MCCDs had incomplete or incorrect information regarding the age, sex and place of residence of the deceased. Inaccurate age and sex-related reporting will impact age and sex-specific mortality statistics45. Similarly, incorrect or missing details of the place of residence can affect the understanding of the geospatial distribution of the diseases46,47. Such clerical errors may also cause technical difficulties in claims related to insurance, pensions and inheritance4.
We observed that errors in abbreviations and illegible handwriting were reported in high proportions. Abbreviations and illegible handwriting though generally regarded as minor certification errors48, 50, some authors have argued that these can be considered major certification errors39. DCs are legal documents often intended for audiences with non-medical backgrounds, such as coders, family members, judicial authorities and other public health stakeholders and researchers39. Hence, using abbreviations and illegible handwriting can cause misinterpretation of COD, inaccurate ICD coding and false statistics. A recent systematic review reporting common errors in MCCD reported that abbreviations and illegibility led to serious coding errors39. Therefore, physicians should entirely refrain from writing abbreviations and illegible handwriting when compiling the DCs.
We observed that 8 (40%) studies had reviewed the MCCD with the medical records of the decedents. To conduct a validation study of the COD data from hospitals, the gold standard procedure will be an autopsy51. However, the frequency of autopsies is decreasing due to operational factors, growing distrust and mostly reserved for medico-legal cases52. Hence, validating the MCCD by reviewing the medical records and developing gold standard diagnoses for the diseases should be a practice to understand the type of errors in MCCD and formulate remedial measures. These methods for validation are rarely applied in Indian hospital settings. The systematic review performed by Rampatige et al53 has proposed a framework for conducting medical records reviews, which researchers can use for death audit-related studies53. However, the application of this framework will be limited by lack of good medical record keeping in many hospitals. Recently, the Indian Council of Medical Research (ICMR) published a detailed framework for conducting an audit of the MCCD at a health facility, which would help the health facilities minimize errors and ensure completeness and timely submission of the MCCD data. The framework will also help establish a death certification review system in facilities54.
We observed that blinding or independent reviewing of the DC was mentioned in two studies8,32. Blinding makes intentional or unintentional bias difficult, thereby enhancing the reliability of study findings55. Several studies have adopted the strategy to blind the reviewers for the original MCCD and, based on their review of medical records, generate the chain of events and the COD report56,57. About 6 (30%) studies mentioned the conduction of training for review of death certification13,14,15,18,19,24. WHO recommends orientation and training for conducting mortality and morbidity reviews for the personnel involved in mortality and morbidity audits to improve the quality of healthcare58. We observed that a strategy for resolving the disagreement was reported in only two studies. When more than one reviewer abstracts data from the same medical records, there is a chance of disagreement and an explicit procedure should be identified to resolve such disagreement59.
We identified a wide range of certification errors, which reflected the lack of a uniform pattern of MCCD and the process of auditing the MCCD. The reviews conducted in several countries have reported such variations in certification errors. These variations may affect the generalizability of the study findings as well as inter-state comparisons. Hence, training certifying physicians for MCCD and adopting a uniform, systematic assessment approach to audit MCCD across all hospitals is critical to improving the quality of MCCD and death audits53. Though most of the included studies mentioned the prescribed WHO format for MCCD, it has been reported that many health settings, especially in rural and remote regions, do not use the standardized format for death certification. All hospitals should uniformly use the WHO-prescribed format for COD certification and auditing purposes. The WHO has also laid down guidelines for auditing facility-based paediatric and maternal deaths58. Similarly, there is a need to develop standardized guidelines for other disease-specific death audits to improve the quality of care.
Findings from the included interventional studies highlighted the usefulness and feasibility of training physicians for MCCD, which could raise the quality of death certification and the nation’s vital registration systems. Previous interventional studies from India8,23,29, the United States of America (USA)60,61, Peru62 and Spain63 have demonstrated that training of certifying physicians for the COD certification improves the quality of DCs and reduces both major and minor certification errors. A workshop-led educational intervention study from five teaching hospitals in the USA showed that the intervention group improved death certification more than the printed-handout group. The workshop group demonstrated a significant reduction in identifying inaccurate cardiac causes as COD from 56 to 6 per cent (P<0.001)60. A meta-analysis assessing the effectiveness of training in improving the quality of MCCD reported a substantial reduction in errors among participants who received training, with pooled risk differences in the range of 15-33 per cent. The study also reported reduced diagnostic errors through refresher training and regular dissemination of MCCD quality assessment findings64.
There are several limitations to the study. We found that the included studies had a very heterogeneous population, where some studies were conducted exclusively for the paediatric population32 and others on cancer patients17. Also, in the interventional studies, the time duration and method of the training interventions varied. We could not find any randomized interventional studies. We also observed varied subjectivity in the assessment of MCCD, which could have affected our study outcomes. Furthermore, we observed a lack of a standardized method for reporting the death certification errors in the included studies, which resulted in difficulty in comparing the results over time and among different regions. We could not find many studies that utilized strategies to limit the bias by blinding the investigators or validating the MCCD with the deceased’s medical records. Lastly, we defined the study period as December 31, 1998 and December 31, 2020 and did not include the published articles in the last three years. In the year 2020, the world witnessed the unprecedented impact of the COVID-19 pandemic on healthcare, which led to several discussions at national and international forums regarding the under-reporting as well as excess mortality reporting due to misclassification related to COVID-19 infection globally65,66.The government of India took several interventions to counter these errors in death reporting, where ICMR developed several guidelines and software for COD reporting since the onset of the pandemic67,68.
A high proportion of errors in the medical certification as the cause of death have been reported in the reviewed studies from India. There is a pressing need to ensure accurate information in the medical certification of the cause of death, which will impact mortality statistics, public health policy, research and learning. Therefore, teaching medical certification of cause of death must be incorporated into medical education. There is a need to follow a standardized approach for auditing death certificates as well.
Financial support & sponsorship
None.
Conflicts of Interest
None.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that no artificial intelligence (AI)- assisted technology was used to assist in the writing of the manuscript and no images were manipulated using AI.
References
- Problems with proper completion and accuracy of the cause-of-death statement. Arch Intern Med. 2001;161:277-84.
- [CrossRef] [PubMed] [Google Scholar]
- Death certification errors at an academic institution. Arch Pathol Lab Med. 2005;129:1476-9.
- [CrossRef] [PubMed] [Google Scholar]
- International statistical classification of diseases and related health problems. (10th revision, Fifth edition). Available from: https://apps.who.int/iris/handle/10665/246208, accessed on January 10, 2021.
- Medical certification of cause of death. Med J Armed Forces India. 2004;60:261-72.
- [CrossRef] [PubMed] [Google Scholar]
- Global and regional causes of death. Br Med Bull. 2009;92:7-32.
- [CrossRef] [PubMed] [Google Scholar]
- How to evaluate the medical certification of death in a hospital: An analysis of 53 death certificates at AIIMS, Bhopal, India. Int J Commun Med Public Health. 2017;4:797-802.
- [CrossRef] [Google Scholar]
- Report on medical certification of cause of death. Available from: https://censusindia.gov.in/2011-Documents/mccd_Report1/MCCD_Report-2018.pdf, accessed on February 4, 2021.
- Educational intervention to improve death certification at a teaching hospital. Natl Med J India. 2009;22:317-9.
- [PubMed] [Google Scholar]
- A cross-sectional study on the knowledge and practice of medical certification of cause of death among junior doctors in a tertiary hospital in North-East India. Int J Commun Med Public Health. 2020;7:3659-64.
- [CrossRef] [Google Scholar]
- Potential gain in life expectancy after partial and complete elimination of specified causes of death: An analysis of medical certification of causes of death data in India and its selected states. Int J multidiscip Res Dev. 2015;2:508-12.
- [Google Scholar]
- Registration of cancer mortality data in a developing area: Chennai (Madras, India) experience. Cancer Causes Control. 1998;9:131-36.
- [CrossRef] [PubMed] [Google Scholar]
- Cause-specific mortality in under-fives in the urban slums of Lucknow, north India. J Trop Pediatr. 1998;44:358-61.
- [CrossRef] [PubMed] [Google Scholar]
- Verbal autopsy of 80,000 adult deaths in Tamilnadu, South India. BMC Public Health. 2004;4:1-7.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Accuracy of WHO verbal autopsy tool in determining major causes of neonatal deaths in India. PLoS One. 2013;8:e54865.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Medical certification of cause of death: instructions for physicians on use of international form of medical certificate of cause of death, 1979. Available from https://apps.who.int/iris/handle/10665/40557, accessed on February 4, 2021.
- Improving the accuracy of death certification. CMAJ. 1998;158:1317-23.
- [PubMed] [PubMed Central] [Google Scholar]
- Characteristics and pattern of mortality in cancer patients at a tertiary care oncology center: Report of 259 cases. Asian Pac J Cancer Prev. 2010;11:1755-9.
- [PubMed] [Google Scholar]
- A Study on appraisal of effectiveness of the MCCD scheme. J Indian Acad Forensic Med. 2010;32:318-20.
- [Google Scholar]
- Assessment of medical certificate of cause of death at a new teaching hospital in Vadodara. Natl J Commun Med. 2011;2:349-53.
- [Google Scholar]
- Evaluation of medical certification of cause of death in one of the teaching hospitals of Ahmadabad. Innovative J Med Health Sci. 2012;2:118-21.
- [Google Scholar]
- Medical certification of cause of death in a tertiary care centre, A matter of concern? Int J Sci Res. 2013;2:1-3.
- [Google Scholar]
- Accuracy in certification of cause of death in a tertiary care hospital-A retrospective analysis. J Forensic Leg Med. 2014;24:33-36.
- [CrossRef] [PubMed] [Google Scholar]
- Impact of an educational intervention on errors in death certification: An observational study from the intensive care unit of a tertiary care teaching hospital. J Anaesthesiol Clin Pharmacol. 2014;30:78-81.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Accuracy in completion of death certificate in Vadodara Municipal Corporation of Gujarat, India. Int J Med Sci Public Health. 2016;5:1148-52.
- [CrossRef] [Google Scholar]
- Knowledge of medical certificate of cause of death amongst doctors and errors in certification. Indian J Forensic Community Med. 2016;3:156-62.
- [CrossRef] [Google Scholar]
- Assessment of medical certification of cause of death at medical college hospital, Bhavnagar, Gujarat. Int J Preven Curat Comm Med. 2018;4:6-8.
- [CrossRef] [Google Scholar]
- Assessment of medical certificate of cause of Death at a tertiary care centre in Mumbai, India. Indian J Forensic Community Med. 2019;6:70-4.
- [CrossRef] [Google Scholar]
- Audit of medical certificate of cause of death at a tertiary care teaching hospital. J Indian Acad Forensic Med. 2019;41:197-200.
- [CrossRef] [Google Scholar]
- Assessment of standards in issuing cause of death certificate before and after educational intervention. IJFMT. 2019;13:25-8.
- [CrossRef] [Google Scholar]
- Evaluation of errors and its etiological relevance with variables associated with death certificate. J Indian Acad Forensic Med. 2011;33:50-6.
- [Google Scholar]
- Medical certification of cause of death at general hospital nalgonda. IJFMT. 2012;6:130-2.
- [Google Scholar]
- Errors in filling WHO death certificate in children: lessons from 1251 death certificates. J Trop Pediatr. 2014;60:74-8.
- [CrossRef] [PubMed] [Google Scholar]
- Analytical Study of medical certification of cause of death. Indian J Forensic Med Toxicol. 2014;8:153-6.
- [CrossRef] [Google Scholar]
- Situational analysis of medical certification of cause of death (MCCD) scheme in municipal corporation of Ahmedabad. Indian J Forensic Community Med. 2015;2:95-9.
- [Google Scholar]
- Adult mortality studies around the world and in India: Data Challenges, Research questions, and novelty of the present study. In: Adult Mortality in India: Trends, Socio-economic Disparities and Consequences. Springer, Singapore: Sustainable Development Goals Series; 2023.
- [Google Scholar]
- Nationwide mortality studies to quantify causes of death: Relevant lessons from India’s million death study. Health Aff (Millwood). 2017;36:1887-95.
- [CrossRef] [PubMed] [Google Scholar]
- Medical certificates of cause of death for people with intellectual disabilities: A systematic literature review. J Appl Res Intellect Disabil. 2018;31:659-68.
- [CrossRef] [PubMed] [Google Scholar]
- Death certification status in Eastern Mediterranean Region: A systematic review. Death Stud. 2022;46:2100-9.
- [CrossRef] [PubMed] [Google Scholar]
- Common errors in reporting cause-of-death statement on death certificates: A systematic review and meta-analysis. J Forensic Leg Med. 2021;82:102220.
- [CrossRef] [PubMed] [Google Scholar]
- The effect of incomplete death certificates on estimates of unintentional opioid-related overdose deaths in the United States, 1999-2015. Public Health Rep. 2018;133:423-31.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Death certification: Errors and interventions. Clin Med Res. 2020;18:21-26.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Garbage codes in the Norwegian cause of death registry 1996-2019. BMC Public Health. 2022;22:1-5.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Algorithms for enhancing public health utility of national causes-of-death data. Popul Health Metrics. 2010;8:9.
- [CrossRef] [Google Scholar]
- Public health utility of cause of death data: Applying empirical algorithms to improve data quality. BMC Med Inform Decis Mak. 2021;21:17.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Demography and public health. In: Detels R, Gulliford M, Karim AQ, Tan CC, eds. Oxford textbook of global public health (6th ed). Oxford, UK: Oxford University Press; 2015. p. :718-735.
- [Google Scholar]
- Stony Brook COVID-19 Research consortium. geospatial distribution and predictors of mortality in hospitalized patients with COVID-19: A cohort study. Open Forum Infect Dis. 2020;7:ofaa436.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Geospatial distribution of under-five mortality in Alexandria, Egypt: a cross-sectional survey. Egypt Pediatric Association Gaz. 2023;71:75.
- [CrossRef] [Google Scholar]
- The impact of errors in medical certification on the accuracy of the underlying cause of death. PloS One. 2021;16:e0259667.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Death certification errors and the effect on mortality statistics. Public Health Rep. 2017;132:669-75.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Improving medical certification of cause of death: Effective strategies and approaches based on experiences from the data for health initiative. BMC Med. 2020;18:74.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Handbook of Autopsy Practice (4th ed). Human Press; 2009. p. :3-7.
- Verbal autopsy as a tool for defining causes of death in specific healthcare contexts: Study of applicability through a traditional literature review. Int J Environ Res Public Health. 2022;19:11749.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Systematic review of statistics on causes of deaths in hospitals: Strengthening the evidence for policymakers. Bull World Health Organ. 2014;92:807-16.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Framework for audit of medical certification of cause of death at health facility. Available from: https://www.ncdirindia.org/All_Reports/MCCD_Frmwrk/Framework_MCCD_Audit.pdf, accessed on February 15, 2023
- Blinding in clinical trials and other studies. BMJ. 2000;321:504.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Death certification errors and the effect on mortality statistics. Public Health Rep. 2017;132:669-75.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Cause of death for patients with breast cancer: Discordance between death certificates and medical files, and impact on survival estimates. Arch Public Health. 2021;79:1-8.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Improving the quality of paediatric care: An operational guide for facility-based audit and review of paediatric mortality. Available from https://www.who.int/publications/i/item/9789241515184, accessed on February 4, 2021.
- Cochrane handbook for systematic reviews of interventions version 6.3 (updated February 2022). Cochrane. Available from: www.training.cochrane.org/handbook, accessed on February 4, 2021.
- Improving death certificate completion: A trial of two training interventions. J Gen Intern Med. 2007;22:544-48.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- An Intervention to improve cause-of-death reporting in New York City Hospitals, 2009-2010. Prev Chronic Dis. 2012;9:120071.
- [Google Scholar]
- Saving lives through certifying deaths: Assessing the impact of two interventions to improve cause of death data in Perú. BMC Public Health. 2018;18:1-11.
- [Google Scholar]
- Evaluating an educational intervention to improve the accuracy of death certification among trainees from various specialties. BMC Health Serv Res. 2007;7:1-6.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Effectiveness of training interventions to improve quality of medical certification of cause of death: Systematic review and meta-analysis. BMC Med. 2020;18:1-22.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Estimating excess mortality due to the COVID-19 pandemic: A systematic analysis of COVID-19-related mortality, 2020-21. Lancet. 2022;399:1513-36.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- The WHO estimates of excess mortality associated with the COVID-19 pandemic. Nature. 2023;613:130-7.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Guidance for appropriate recording of COVID-19 related deaths in India. National Centre for Disease Informatics and Research. Available from: https://ncdirindia.org/Downloads/CoD_COVID-19_Guidance.pdf, accessed on December 15, 2023.
- NCDIR e-mortality software (NCDIR e-Mor). Available from: http://ncdirindia.org/e-mor/, accessed on December 15, 2023.






