Translate this page into:
A randomized controlled study of bedside electrocardiograph-guided tip location technique & the traditional chest radiography tip location technique for peripherally inserted central venous catheter in cancer patients
For correspondence: Dr AiMin Li, Department of Oncology, Lymphoma Diagnosis & Treatment Centre of Henan Province, The First Affiliated Hospital of Zhengzhou University, Zhengzhou, PR China e-mail: aimin_li68@sina.com
-
Received: ,
This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Background & objectives:
The peripherally inserted central catheter (PICC) has the advantages of higher safety, lower infection rate and longer retention time than peripherally inserted catheter. This study was aimed to evaluate the accuracy and safety of bedside electrocardiograph (ECG)-guided tip location technique in PICC in cancer patients, and compared with traditional chest radiography tip location technique.
Methods:
Patients were randomly assigned into two groups: The ECG test group patients underwent PICC insertion with ECG-guided tip location, while the control group patients had PICC insertion by the conventional method. The precision of tip location was verified by chest radiography in both groups. The groups were compared with regard to the accuracy of tip placement, anxiety levels before and after the procedure; medical cost and incidence of complications at one week, three months and six months after PICC insertion.
Results:
Accurate tip location was achieved in 99.30 per cent in the ECG test group vs 92.30 per cent in the control group (P <0.001). At 24 h after the procedure, the anxiety level was significantly lower in the ECG test group. The presence of thrombogenesis was significantly lower in the ECG test group at both three months and six months after the procedure (P=0.04 and P=0.03, respectively).
Interpretation & conclusions:
The ECG-guided PICC tip location technique was accurate and caused fewer procedure-related complications and less anxiety in patients compared to chest radiography tip location technique. Radiographic confirmation of PICC tip position may not be needed when ECG guidance is used and thus it can help avoid radiation exposure.
Keywords
Anxiety
chest radiograph
complications
electrocardiograph-guided
tip location
Compared to the traditional central venous catheter, the peripherally inserted central venous catheter (PICC), inserted through an upper extremity peripheral vein, has the advantages of higher safety, lower infection rate and longer retention time12. It is useful for providing long-term parenteral nutrition and intravenous chemotherapeutic drugs and antibiotics34. Appropriate tip placement of the PICC is important. Racadio et al5 found complication rate was 3.8 per cent if tip location resided in the superior vena cava; however, complication rate rose to 28.8 per cent if tip location resided in other places, which increased the risk of complications. Serious complications with PICC include tip migration, infection, thrombosis and phlebitis67.
At present, the main techniques of PICC insertion include blind puncture, Seldinger technique and ultrasound-guided modified Seldinger technique8. The electrocardiograph (ECG)-guided PICC tip location technique is easy to perform, allows real-time adjustment of tip position and does not involve radiation exposure9, which makes it the ideal technique. However, there have been a few studies on the safety and efficacy of bedside ECG-guided PICC tip location in cancer patients. Liu et al10 and Zhao et al11 studied 85 and 116 Chinese patients with ECG-guided PICC, respectively, and reported high accuracy of tip localization, but they did not examine the precision of tip location, procedure related anxiety and PICC-associated complications. This study was aimed to explore the accuracy, precision, safety, procedure-related anxiety and complications associated with bedside ECG-guided PICC tip location compared to traditional chest radiography tip location technique.
Material & Methods
From June 1, 2014 to April 30, 2016, 294 patients in the Oncology department of the First Affiliated Hospital of Zhengzhou University, Henan, PR China, were approached to participate voluntarily in this randomized controlled clinical trial (Fig. 1). The study was approved by the Ethics Committee of the First Affiliated Hospital of Zhengzhou University (Scientific Research No. 33, 2014). All participants gave written informed consent.
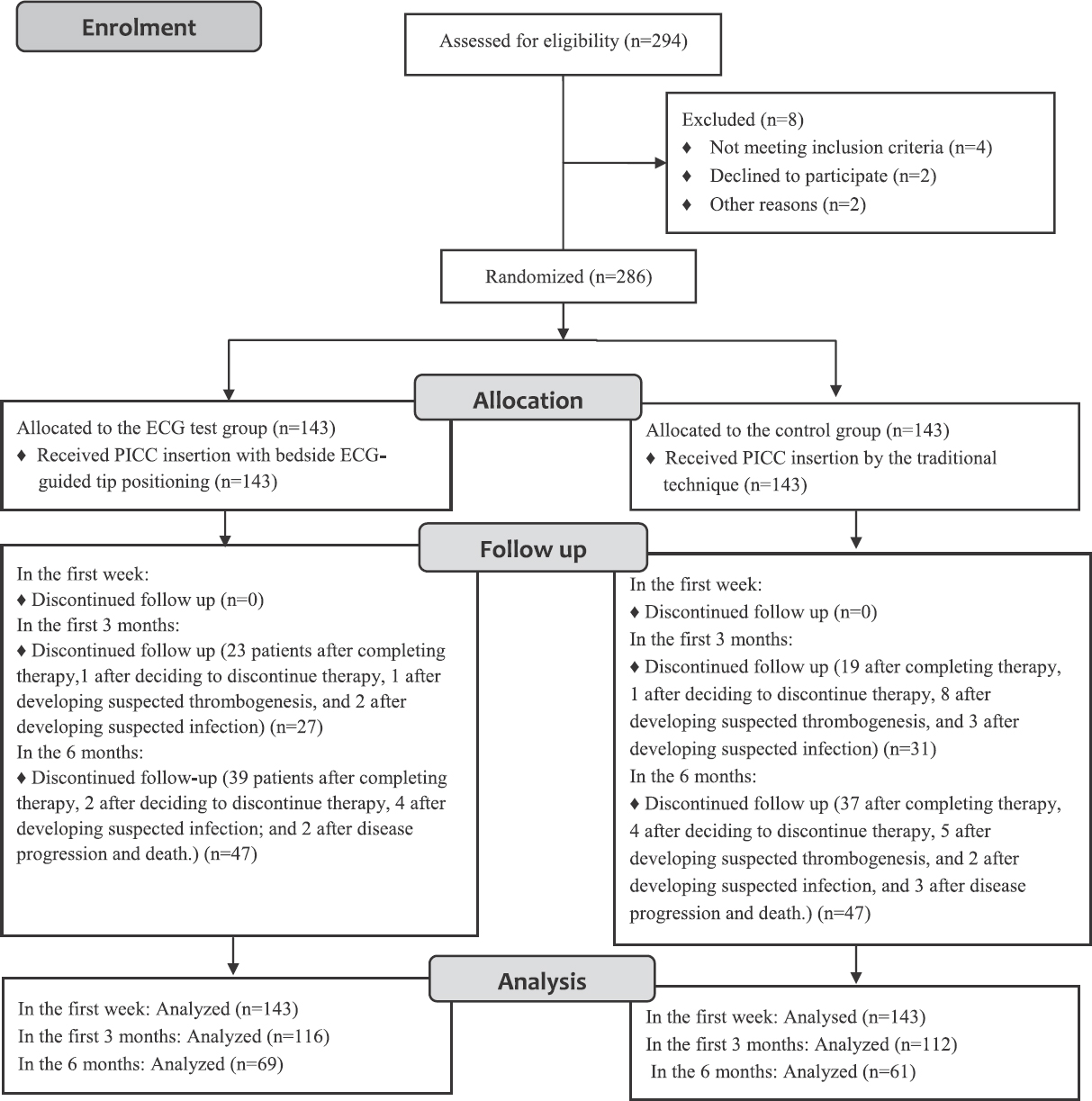
- Flowchart showing the study design. PICC, peripherally inserted central venous catheter; ECG, electrocardiograph.
Patients were eligible for inclusion if they were inpatients and cancer patients. Patients were excluded if they had (i) serious bloodstream infection or systemic infection before catheterization; (ii) superior vena cava compression syndrome; (iii) serious cardiovascular disease (e.g., atrial fibrillation, pulmonary heart disease with abnormal P waves, or severe heart block); (iv) they were ≥18 yr old, and (v) they were on pacemakers and using implantable defibrillators. Four patients did not meet inclusion criteria, two patients declined to participate and two patients excluded because of other reasons, so 286 participants were found to be eligible for inclusion in the study.
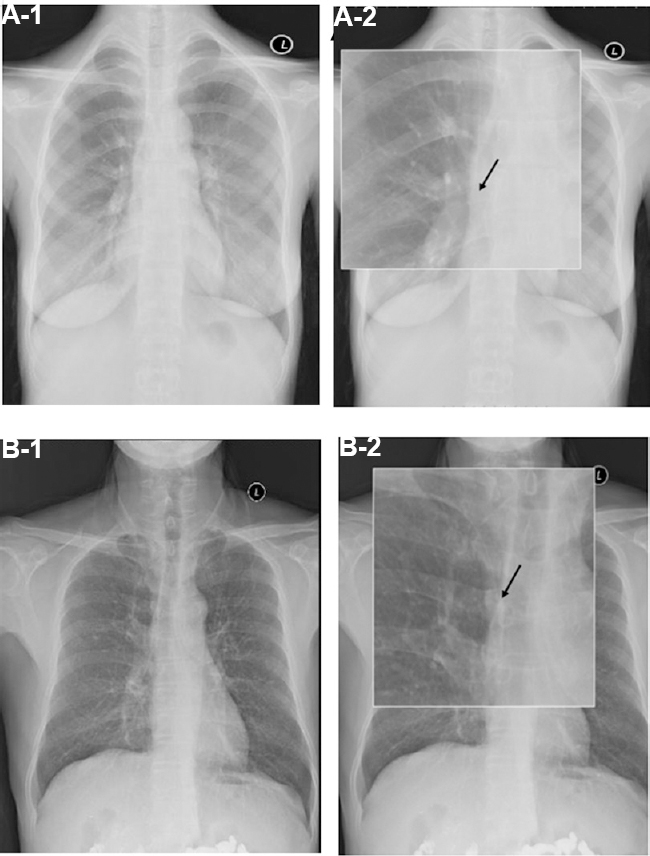
Using a random number table, participants were separated into two groups: (i) the ECG test group (n=143), who underwent PICC insertion with bedside ECG-guided tip positioning, and (ii) the control group (n=143), who underwent PICC insertion by the traditional technique. There were no significant differences between the groups in age, gender, height, weight, upper arm circumference, educational level, diagnosis, co-morbidities, history of prior central venous catheter, history of PICC insertion, platelet count and the prothrombin time (Table I).
According to the pilot study result, the appropriate tip location rate of the control group was 89.0 per cent; the ECG test group was 98.4 per cent. PASS software (NCSS, LLC, USA) was used to calculate the sample size, and a sample size of 143 participants of each group was calculated with the statistical performance of 0.9093.
Methods
Catheterization technique: In all patients, the 18G (4Fr) × 65 cm, BD First PICC™ Kits (Becton Dickinson Infusion Therapy Systems Inc., USA) were used. The catheters were inserted by the same specialist nurses with the PICC qualification in a specially confined PICC puncture chamber and maintained in hospital by nurse PICC teams. The distance from the venepucture point to the right sternoclavicular joint, plus 5-7 cm, was the estimated catheter insertion length. The upper arm circumference was measured 10 cm above the elbow crease. Before ultrasound-guided venepuncture, the arm was cleaned and sterilized three times using 75 per cent alcohol and chlorhexidine.
The basilic vein was the first choice for venepunture. During the procedure, the length of the catheter in the body, the presence of resistance to removal of the guidewire within the catheter and the time taken for the procedure (from skin disinfection to application of the sticking plaster) were recorded.
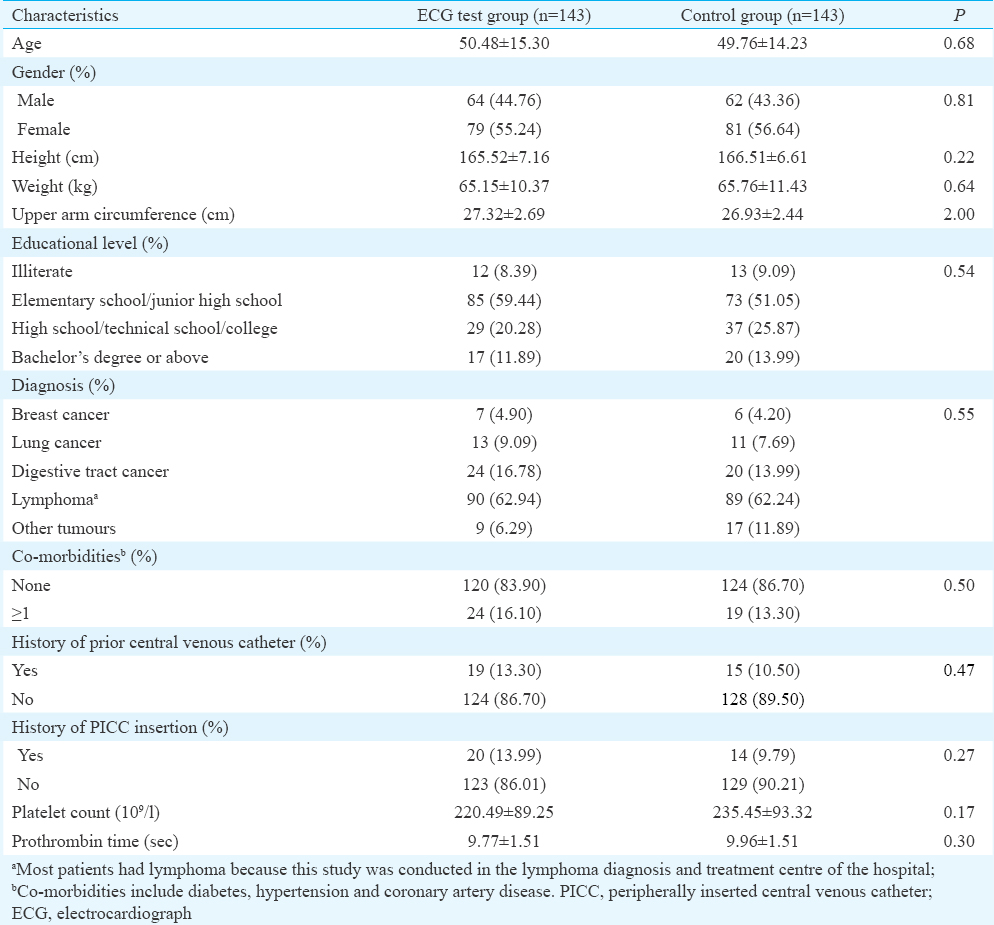
In the ECG group patients, the four limb leads of the ECG machine were attached and normal P waves and sinus rhythm were confirmed on the lead II tracing. When the catheter was inserted almost up to the estimated length, the right arm lead was removed, the clamps sterilized and then attached to the guide wire. The guide wire was now advanced slowly, 0.5-1 cm at a time, while observing the P wave changes on the monitor. Three ECG P waveforms were obtained during the course of the catheterization: (i) the blunt short P wave of normal sinus rhythm; (ii) the biphasic P waves indicating tip location in the right atrium and (iii) high-amplitude P waves indicating tip location at the junction of the superior vena cava and the right atrium (P-wave amplitude 80% of QRS) or tip location in the lower one-third of the superior vena cava (P-wave amplitude 50% of QRS).
Chest radiography verification: For verification of tip position, chest radiography is generally accepted to be the gold standard12, and accordingly, chest radiographs were taken in all patients to confirm correct tip position. The ideal position was defined as the middle and lower one-third of the superior vena cava or the junction of the superior vena cava and the right atrium.
Anxiety levels before and after PICC: The State-Trait Anxiety Inventory (STAI) prepared by the Gaudry et al13 is a commonly used measure of trait and state anxiety and translated into Chinese in 198814. Each item is graded on a scale of 1 to 4 (1: no, 2: some, 3: moderate and 4: obvious), and the total score ranging from 20 to 80 can be used to quantify an unpleasant short-term emotional experience1516. The Chinese version of the STAI had a Cronbach's alpha of 0.8817; in our study, Cronbach's alpha of the STAI was 0.89. The Chinese version of the inventory was used to assess anxiety levels in patients 24 h before and 24 h after catheterization.
PICC-related complications: PICC-related complications after one week, three months and six months were recorded in all patients who had been on regular catheter infusion therapy, with regular maintenance of the catheter. The patients were followed up every two weeks for their health status and the condition of the catheter.
Statistical analysis: SPSS 17.0 software (SPSS Inc., Chicago, IL, USA) was used for data analysis. Quantitative data (age, height, weight, upper arm circumference, platelet count, prothrombin time, activated partial thromboplastin time, cost and anxiety level) were expressed as the means±standard deviation. Qualitative data (gender, educational level, diagnosis, co-morbidities, history of prior central venous catheter, history of PICC insertion and complications) were compared using the chi-square test.
Results
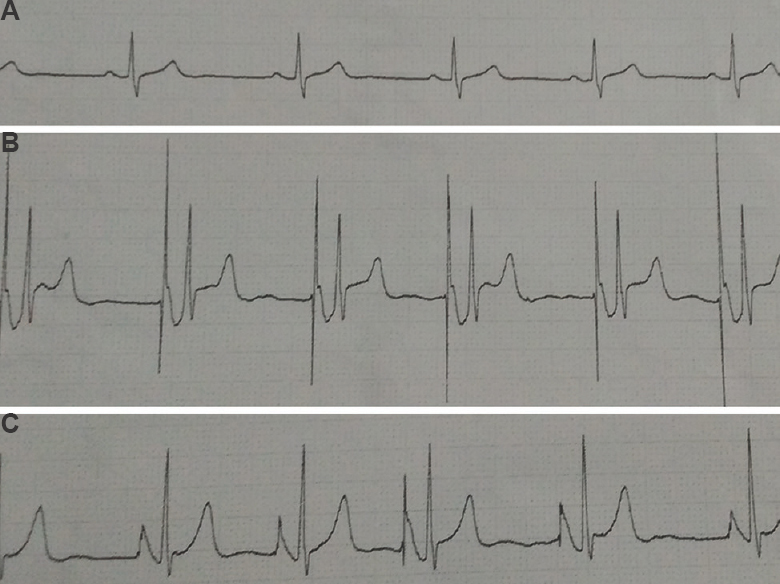
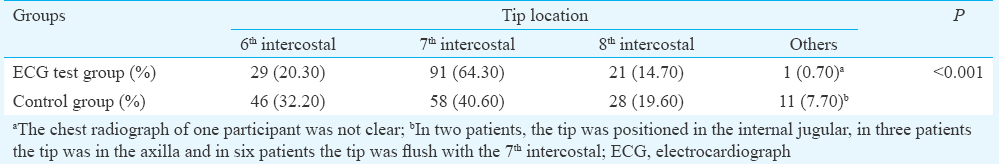
Accuracy and precision of tip positioning: Accurate catheter tip positioning was achieved in 99.3 per cent in the ECG test group versus 92.3 per cent in the control group (P=0.003; Fig. 2). The catheter tips flush with the 6th, 7th and 8th intercostal were 20.30, 64.30 and 14.70 per cent, respectively, in the ECG test group versus 32.20, 40.60 and 19.60 per cent, respectively, in the control group and the difference was significant (Fig. 3 and Table II).
- Three electrocardiograph P wave forms seen during catheterization in the electrocardiograph test group. (A) Blunt, low-amplitude, P waves. (B) Biphasic P waves. (C) High-amplitude P waves (50 or 90% of QRS amplitude).
- Chest radiographs of patients from the two groups. Arrow indicates the position of the catheter tip. Tip location flush with the 7th intercostal in a patient from the electrocardiograph test group. A-1 (chest radiograph); A-2 (magnified image). Tip location flush with the 5th intercostal in a patient from the control group. B-1 (chest radiograph); B-2 (magnified image).
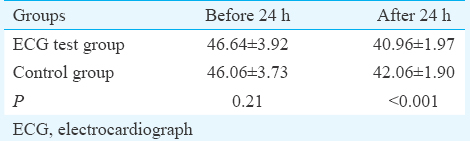
PICC-associated anxiety: The anxiety scores 24 h before catheterization in the two groups were not significantly different. However, 24 h after catheterization, the anxiety score in the ECG test group was significantly (P <0.001) lower than that in the control group (Table III).
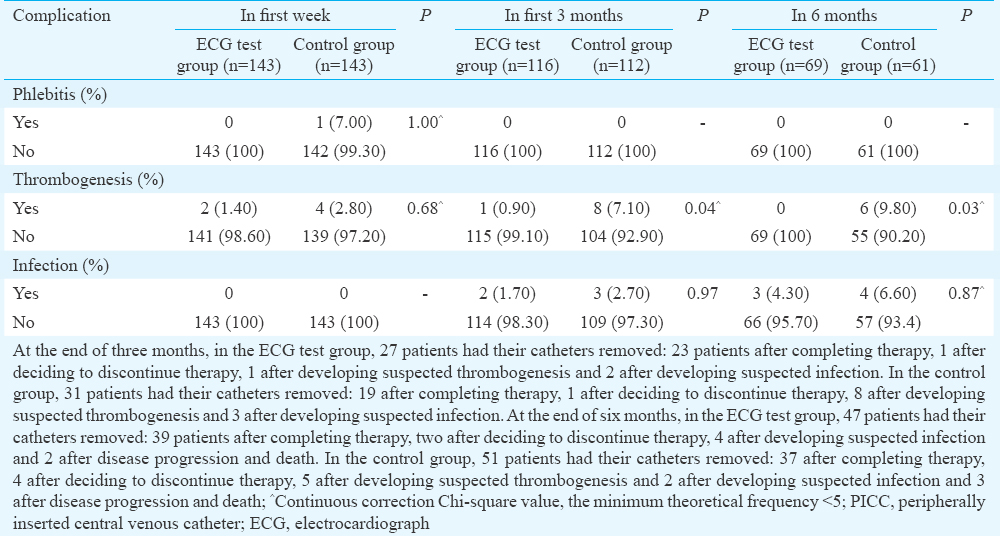
Procedure-related complications: In the first week, two patients had thrombogenesis in the ECG test group versus four patients in the control group. No patient in either group had chest discomfort, arrhythmia, or infection. At the end of three months and six months, the incidence of thrombogenesis in the ECG test group was significantly lower than that in the control group. (P=0.04 and P=0.03, respectively) (Table IV).
Discussion
There have been only a few studies to date on the precision of different techniques for PICC tip location. Consistent with other studies1819, our study showed that the accuracy of the ECG-guided method was better than that of the traditional method. In the ECG test group patients, real-time adjustment of PICC tip position was possible by observing the lead II P wave morphology on the monitor. In the traditional method, a chest radiograph is necessary to confirm correct tip position whenever the PICC tip is readjusted. In this study, 11 patients in the control group needed adjustment of PICC tip position followed by repeat chest radiography to confirm correct positioning. This increased the radiation exposure to the patient.
Patients experience anxiety during PICC insertion procedure20, so anxiety levels were assessed 24 h after PICC insertion; anxiety levels were 40.96±1.97 and 42.06±1.90, respectively. It could be possible that the patients in the ECG test group were reassured by the information provided to them at enrolment that they would be receiving a technologically advanced treatment with high success rates. Moreover, radiological confirmation of success at the end of the procedure would have allayed anxiety further. Once the precision of the ECG-guided technique is established, confirmation with chest radiography will not be necessary, and the cost of the procedure will be correspondingly less; Bream and Gu21 and Walker et al22 have also suggested the same.
PICC-related complications need to be minimized as they may affect, or even interrupt, the treatment of the patient's underlying condition23. In our study, the incidence of procedure-related complications was low and not significantly different between the two groups in the first week after PICC insertion. No patient had chest discomfort, arrhythmia or infection. To secure the safety usage of PICC and reduce the PICC-related complications, the strict rules of handling, the skill and experience of operator and cooperation of patients are necessary24. However, at the end of three and six months, the cases with thrombogenesis were found to be significantly lower in the ECG test group. In the control group, some patients needed repeated adjustment of PICC tip location; this may have caused damage to the vein wall and led to the higher incidence of thrombogenesis.
Our study had some limitations. First, only adult cancer inpatients were included in the study, and thus our findings might not apply to other types of patients (e.g., children, outpatients, or peripheral blood stem cell transplantation patients). Second, most of our study participants were lymphoma patients (because this study was conducted in the lymphoma diagnosis and treatment centre of the hospital).
In conclusion, the bedside ECG-guided PICC insertion method was found to be accurate, it allowed real-time adjustment of the PICC tip, and avoided radiation exposure. Significantly lower post-procedure anxiety levels and fewer postoperative complications are other advantages. With nurses trained in ECG-guided PICC tip location, it can be expected to become the preferred technique for patients without serious cardiovascular disease.
Acknowledgment
Authors thank Prof. Chen Wei in the Nutrition department of Peking Union Medical College Hospital for guidance on PICC operation techniques in this study.
Financial support & sponsorship: None.
Conflicts of Interest: None.
References
- Catheter-associated bloodstream infections and thrombotic risk in hematologic patients with peripherally inserted central catheters (PICC) Support Care Cancer. 2015;23:3289-95.
- [Google Scholar]
- A role for peripherally inserted central venous catheters in the prevention of catheter-related blood stream infections in patients with hematological malignancies. Int J Hematol. 2014;100:592-8.
- [Google Scholar]
- Peripherally inserted central catheters in non-hospitalized cancer patients: 5-year results of a prospective study. Support Care Cancer. 2015;23:403-9.
- [Google Scholar]
- Pediatric peripherally inserted central catheters: Complication rates related to catheter tip location. Pediatrics. 2001;107:E28.
- [Google Scholar]
- Impact of a surgeon-led peripherally inserted central venous catheter team on peripherally inserted central venous catheter-related complications and costs. Surg Infect (Larchmt). 2016;17:352-6.
- [Google Scholar]
- The incidence of peripheral catheter-related thrombosis in surgical patients. Thrombosis. 2016;2016:6043427.
- [Google Scholar]
- Comparison of ultrasound-guided modified seldinger technique versus blind puncture for peripherally inserted central catheter: A meta-analysis of randomized controlled trials. Crit Care. 2015;19:64.
- [Google Scholar]
- Intravenous electrocardiographic guidance for placement of peripherally inserted central catheters. J Electrocardiol. 2010;43:274-8.
- [Google Scholar]
- Evaluating ECG-aided tip localization of peripherally inserted central catheter in patients with cancer. Int J Clin Exp Med. 2015;8:14127-9.
- [Google Scholar]
- Clinical evaluation of the use of an intracardiac electrocardiogram to guide the tip positioning of peripherally inserted central catheters. Int J Nurs Pract. 2016;22:217-23.
- [Google Scholar]
- Central venous pressure measurements: Peripherally inserted catheters versus centrally inserted catheters. Crit Care Med. 2000;28:3833-6.
- [Google Scholar]
- Validation of the state-trait distinction in anxiety research. Multivariate Behav Res. 1975;3:331-41.
- [Google Scholar]
- Depression and anxiety trajectories among women who undergo an elective cesarean section. PLoS One. 2014;1:1-8.
- [Google Scholar]
- Late pregnancy thyroid-binding globulin predicts perinatal depression. Psychoneuroendocrinology. 2016;65:84-93.
- [Google Scholar]
- Characteristics of schizophrenia suicides compared with suicides by other diagnosed psychiatric disorders and those without a psychiatric disorder. Schizophr Res. 2014;155:59-65.
- [Google Scholar]
- Auricular acupressure relieves anxiety and fatigue, and reduces cortisol levels in post-caesarean section women: A single-blind, randomised controlled study. Int J Nurs Stud. 2016;53:17-26.
- [Google Scholar]
- The intracavitary ECG method for positioning the tip of central venous access devices in pediatric patients: Results of an italian multicenter study. J Vasc Access. 2015;16:137-43.
- [Google Scholar]
- Evaluation of the correct position of peripherally inserted central catheters: Anatomical landmark vs. electrocardiographic technique. J Vasc Access. 2015;16:394-8.
- [Google Scholar]
- Use of an ECG-based confirmatory technique for bedside placement of reverse-tunneled cuffed dialysis catheters in three morbidly obese patients. Kidney Int. 2015;88:633-6.
- [Google Scholar]
- Effectiveness of electrocardiographic guidance in CVAD tip placement. Br J Nurs. 2015;24:S4-S6. S8-12
- [Google Scholar]
- Complication rates among peripherally inserted central venous catheters and centrally inserted central catheters in the medical Intensive Care Unit. J Crit Care. 2016;31:238-42.
- [Google Scholar]
- Malposition of peripherally inserted central catheter: Experience from 3012 cancer patients. Int J Nurs Pract. 2014;20:446-9.
- [Google Scholar]






