Translate this page into:
A mini-review of Bunyaviruses recorded in India
Reprint requests: Dr. Devendra T. Mourya, Microbial Containment Complex, ICMR-National Institute of Virology, Sus Road, Pashan, Pune 411 021, Maharashtra, India e-mail: directorniv@gmail.com
-
Received: ,
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Newly emerging and re-emerging viral infections are of major public health concern. Bunyaviridae family of viruses comprises a large group of animal viruses. Clinical symptoms exhibited by persons infected by viruses belonging to this family vary from mild-to-severe diseases i.e., febrile illness, encephalitis, haemorrhagic fever and acute respiratory illness. Several arthropods-borne viruses have been discovered and classified at serological level in India in the past. Some of these are highly pathogenic as the recent emergence and spread of Crimean-Congo haemorrhagic fever virus and presence of antibodies against Hantavirus in humans in India have provided evidences that it may become one of the emerging diseases in this country. For many of the discovered viruses, we still need to study their relevance to human and animal health. Chittoor virus, a variant of Batai virus; Ganjam virus, an Asian variant of Nairobi sheep disease virus; tick-borne viruses such as Bhanja, Palma and mosquito-borne viruses such as Sathuperi, Thimiri, Umbre and Ingwavuma viruses have been identified as the members of this family. As Bunyaviruses are three segmented RNA viruses, they can reassort the segments into genetically distinct viruses in target cells. This ability is believed to play a major role in evolution, pathogenesis and epidemiology of the viruses. Here, we provide a comprehensive overview of discovery, emergence and distribution of Bunyaviruses in India.
Keywords
Animal virus
arthropods
Bunyavirus
CCHF
RNA virus
zoonosis
Introduction
Globally, emerging viral infections constitute a major public health challenge. About 350 viruses, most of which are arthropod borne, are classified in the Bunyaviridae family. Bunyaviridae is one of the largest families of animal viruses. Individuals infected by different Bunyaviruses exhibit a range of mild-to-severe diseases i.e., febrile illness, encephalitis, haemorrhagic fever and acute respiratory illness. Earlier, many Bunyaviruses have been isolated and characterized at the serological level in India, for example, Ingwavuma virus (INGV), Thottapalayam virus (TPMV), Umbre (UMB), sandfly fever virus (SFV), Nairobi sheep disease virus/Ganjam virus (GANV), etc1234. There is a need to understand the members of this family at molecular level which may help to understand their disease profile in nature.
Bunyavirus is named after Bunyamwera, Uganda, where the virus was first found in mosquitoes5. The particles of Bunyaviridae family of viruses are spherical and of 80-120 nm in diameter. These have a common genetic organization of three segmented negative-stranded RNA (S, M and L segments). These are subdivided into five genera on the basis of antigenic, genetic and ecological relatedness. Except for the genus Tospovirus which is pathogenic in plants, Orthobunyavirus, Hantavirus, Nairovirus and Phlebovirus genera consist of enzootic viruses and some of these cause zoonotic diseases in humans. Of the more than 537 known arboviruses, more than 350 known viruses belong to these four genera. About 174 of these are listed under the genus Orthobunyavirus and include about half of the nearly 60 viruses of the family Bunyaviridae causing human diseases. Humans act as accidental dead-end hosts for these viruses in a zoonotic transmission cycle that alternates between arthropods and mammals (mostly rodents)67.
Chittoor Virus (Chitv)/batai Virus (Batv)
Chittoor virus (CHITV) was first isolated in 1957 from Anopheles barbirostris collected from Brahmanpalli, Chittoor district, Andhra Pradesh, India8. Subsequently, several isolates of this virus were obtained from Anopheles and Culex mosquitoes as well as from a piglet in India910. This virus was placed in Bunyamwera group based on serological characterization11. It was found to be antigenically related to Calovo virus and Batai virus (BATV) isolated from Slovakia and Malaysia, respectively12. Repeated isolations of CHITV and seroprevalence in several States suggest that the virus has been circulating in India for a many years13. However, this virus has not caused any outbreak or exhibited any disease symptoms involving humans. Its ability to replicate in vertebrates and mosquitoes may be the cause of concern for public health as it is related to severe fever with thrombocytopenia. A reassortant between Ngari virus and BATV was found to be associated with febrile human illness in Sudan14. This emphasizes that, though BATV on its own may not cause human or animal disease, it has the potential to cause febrile illness after reassortment with other viruses of the Bunyamwera group.
CHITV was isolated from Anopheles mosquitoes (An. barbirostris and An. subpictus from Andhra Pradesh and Karnataka, respectively), Culex mosquitoes (Cx. tritaeniorhynchus and Cx. pseudovishnui from Karnataka) and swine (Sus scrofa from Karnataka)15. A phylogenetic study based on S, M and L segments of CHITV isolated from India showed that a genetically uniform strain of CHITV is circulating in India, despite being isolated from different hosts i.e., mosquitoes and pigs. Moreover, the strains isolated in the 1960s and 1980s have not changed genetically, indicating the conserved nature of the virus even after several years of circulation in nature16.
A novel BATV NM/12 strain was isolated from bovine serum collected in inner Mongolia, China, and based on the L segment, it was found to be most closely related to the Chittoor strain17.
Umbre Virus (Umbv)
Umbre virus (UMBV) was first isolated in 1955 from Cx. vishnui group of mosquitoes, collected at Umbre, in Kolar district of Maharashtra, India1819, and was classified as Orthobunyavirus (Turlock serogroup which includes three other viruses, namely, M'opoko virus from Africa, Lednice virus from Europe and Turlock virus from America; https://wwwn.cdc.gov/arbocat/VirusDetails.aspx?ID=499&SID=5). Even though UMB virus is classified as a Bunyavirus, it cross-reacts by complement fixation (CF) and haemagglutinin inhibition (HI) assays with Barmah forest virus, an alpha virus from Australia18. Eight isolates obtained from Culex mosquitoes were characterized based on partial glycoprotein (G2) gene. The differences within these isolates at nucleotide and amino acid levels were 26 and 17 per cent, respectively. Phylogenetic analysis of 345 bp of glycoprotein gene G2, of UMBV and other Orthobunyaviruses, showed six distinct lineages, namely, Bunyamwera, Simbu, California encephalitis, Group C, Kaeng Khoi (KK) and UMBV. On comparing partial M gene, four lineages, excluding Group C viruses and Simbu group of viruses, were seen suggesting that UMBV represents a distinct group within the genus Orthobunyavirus19. UMBV has so far not been isolated from humans or animals and it is not known whether it causes any disease in humans or animals.
Kaikalur Virus
This virus was isolated from a mosquito pool comprising 100 Cx. tritaeniorhynchus collected in a cattle shed at Kaikalur town, Krishna district, Andhra Pradesh, in 197120. The virus belongs to Simbu group and is closely related to Shuni virus isolated in Nigeria by CF and neutralization tests. In 2008, it was shown by Yamakawa et al21, that Aino virus isolated from Japan was closely related to Kaikalur virus. Aino and Kaikalur viruses were found to be indistinguishable by CF or neutralization tests22. These results indicate a broader global distribution pattern of the virus. Although Aino virus is known to cause developmental disorders in foetus of ruminants2324, the pathogenic potential of Kaikalur virus to humans and animals is not reported.
Thimiri Virus
This was isolated from North Arcot district (currently named Vellore district), Tamil Nadu, in 1962 from Ardeola grayii, paddy bird25. Based on serology and sequencing data of partial S gene, though this virus was found to belong to Simbu serogroup of arboviruses26, it was not closely related to other Simbu viruses and was placed in its own complex. Thimiri virus is associated with birds in south India, Egypt and midges in Australia27. The pathogenic potential of Kaikalur virus to humans and animals is not known.
Sathuperi Virus (Satv)
This virus was isolated from a pool of Cx. vishnui in 1957 from a place called Sathuperi village, North Arcot district, Tamil Nadu, India27. This virus has been registered in the International Arboviruses catalogue and has been shown to belong to Simbu group28. Sathuperi virus (SATV) was also identified in Japan in 1999, isolated from cattle and Culicoides biting midges29. During an outbreak investigation of ruminants in Northern Europe caused by Schmallenberg virus, sequencing of genomic RNA segments of the virus showed that the M gene RNA of Schmallenberg virus was very similar to SATV. Phylogenetic analysis further indicated that Schmallenberg virus is a reassortant, with the M gene RNA segment from SATV29. Human disease caused by SATV virus is not known so far.
Ingwavuma Virus
In India, INGV was isolated in 1963 from a paddy bird A. grayii (Sykes) (from Balagodu village) in Shimoga district in the then Mysore state (at present Karnataka) of South India1. The isolations from pig were made from Tumkur district, whereas the isolations from humans were made from Kolar district in Karnataka State. However, no studies have been done to understand its epidemiology in this country1. Human disease caused by INGV is not known so far.
INGV belongs to Simbu serogroup in genus Orthobunyavirus. It was first isolated in 1959 on the banks of ‘Ingwavuma river’ near the village of Ndumu, South Africa, from a passerine bird Hyphanturgus (Ploceus) ocularis and from mosquitoes such as Ae. circumluteolus, Cx. guiarti, Cx. neavei and Cx. vishnui30. Later on, its presence was recorded from several countries in Africa and Asia1313233. Pigs are considered to be the natural vertebrate host in Thailand, but isolations from wild birds in Africa and India suggested a natural bird-mosquito cycle also27.
In spite of many reports of INGV worldwide, complete genome sequence of INGV is not available till date. No information is available about the disease caused, natural cycle of the virus or its molecular characterization. The study of virus pathology and its role in involvement in human disease is needed.
Phylogenetic study of nucleocapsid gene and glycoprotein gene of four viral isolates from India showed that Simbu viruses have evolved into at least five lineages and INGV from India had been clustered into third lineage16.
Ganjam Virus (Ganv)
Ganjam virus was initially isolated from adult Haemaphysalis intermedia and H. wellingtoni ticks and Cx. vishnui mosquitoescollected from goats in Ganjam district, Odisha, Shimoga district, Karnataka, and Vellore, North Arcot district, Tamil Nadu, respectively34. The presence of GANV was again reported in 1977 during an investigation of acute febrile illness shown by fever, anorexia and lumbar paralysis of sheep in Chittoor district of Andhra Pradesh, India35. GANV was isolated from adult H. intermedia and R. hemaphysaloides ticks infecting domestic animals in some villages near Pune, Maharashtra, between 2000 and 200235.
Based on the documented evidence of isolation of GANV from ticks, mosquitoes, sheep and humans, it can be stated that the virus is prevalent in different parts of India. In addition, GANV antibodies were detected in sheep and goat serum samples in Verrapuram during an episode of febrile illness in 199436. Neutralizing antibodies for the virus were found in human samples based on serological surveys conducted in Tamil Nadu and Jammu and Kashmir. Human laboratory-acquired infection of GANV with febrile illness, abdominal pain, back pain, headache, nausea, vomiting and conjunctival infection has been reported36.
The genome S RNA segment of Nairobi sheep disease virus (NSD) and GANVs has been shown to differ by only 10.1 and 3.3 per cent at the nucleotide and amino acid levels, respectively. Therefore, GANV may be an Asian variant of NSD virus. Further, GANV and NSD are more closely related than other characterized Nairoviruses, no evidence of reassortment was found37.
Crimean-Congo Haemorrhagic Fever (Cchf) Virus
CCHF virus causes severe acute febrile illness and haemorrhagic fever with an overall case fatality of 9-50 per cent. It belongs to family Bunyaviridae and genus Nairovirus. CCHF was first detected in the Crimean peninsula in the mid-1940s38. It was first isolated from a patient in Kisangani, the Democratic Republic of Congo, in 195638. Direct exposure to blood or other secretions resulting in person-to-person transmission and instances of nosocomial transmission has been documented. Ixodid ticks, particularly those belonging to the genus Hyalomma, are known vectors of CCHF. The virus is capable of persisting in the tick throughout its life cycle by transstadial transmission. It can also be passed onto the offspring by transovarial transmission38. Cattle and goats play an important role in the natural cycle of the virus. CCHFV replicates to high titres in the lung, liver, spleen and reticuloendothelial system in other organs in these animals. Unlike humans, it generally causes only subclinical disease in cattle. Human infections show high levels of viral replication occurring in all major organs, including the liver accompanied by haemorrhagic manifestations38.
Although CCHF had been detected in neighbouring countries such as Pakistan and China, it was confirmed for the first time in India in 201139. Nosocomial human infections with haemorrhagic manifestations were reported from a tertiary care hospital in Ahmadabad, Gujarat, in 201139. Domestic animals from Kolat and Ahmadabad were also found to be positive for anti-CCHF IgG antibodies. The possible sources of CCHFV infection were virus-infected Hyalomma ticks and livestock at the rural residence of the index case. In addition, a retrospective sample analysis showed the prevalence of CCHFV in Gujarat and Rajasthan before this outbreak40. So far, there is no evidence of circulation of multiple strains of the virus in the country. Though the 2011 outbreak may not have resulted from a very recent introduction, the probability of a recent re-introduction from any of the neighbouring countries during thoroughfare of livestock needs to be considered41.
In addition, a CCHF case was also confirmed from Sirohi, Rajasthan State, in 2014, and during 2015, a nosocomial outbreak was recorded in a private hospital of Rajasthan which affected nursing staff. This indicated that trade of livestock and consequent movements of domestic animals infested with infected ticks may be the reason for the spread of CCHFV to newer areas42. Further, a cross-sectional serosurvey of CCHFV in livestock from 22 States and one Union Territory reported that this virus was widespread in the livestock population of India43. With the increasing spread of CCHFV to newer regions of the country, it becomes imperative to conduct regular surveillance programmes for human and animals. Increased awareness about the disease and its spread among at-risk population such as abattoir workers, people working in proximity with livestock and medical personnel working in CCHF-endemic areas is needed.
Bhanja Virus (Bhav)
Bhanja virus (BHAV) was first isolated from a pool of ticks H. intermedia collected from a goat displaying lumbar paralysis in Bhanjanagar (district Ganjam, Odisha, India) in 1954. It was named based on the region of the isolation44. BHAV causes fever and symptoms indicating the central nervous system affection in young ruminants (lambs, kids, and calves). Bhanja virus has been isolated in India, various parts of Africa, former USSR and Europe45. Metastriate ticks of the genera Haemaphysalis, Dermacentor, Hyalomma, Rhipicephalus, Boophilus and Amblyomma transmit this arbovirus. Sheep, goat, cattle, African hedgehog Atelerix albiventris and African ground squirrel Xerus erythropus are vertebrate hosts of BHAV. It is so far not known to cause disease in humans. The complete genome sequence of BHAV has helped in phylogenetically placing the virus in the genus Phlebovirus in the Bunyaviridae family45.
Sandfly Fever Virus (Sfv)
The activity of SFV in India was suspected for many years on the basis of clinical diagnosis. Twenty isolates of this virus were obtained from India out of which 11 were identified as Naples and nine as Sicilian type, from human serum samples and wild caught sandflies46. The disease is usually self-limiting. However, sometimes, neurological involvement resulting in morbidity is seen47. New antigenically distinct serotypes have been identified from Europe, Southeast Asia, central Asia and Africa48.
Malsoor Virus (Mv)
Malsoor virus (MV) was isolated from Mahabaleshwar, Maharashtra, from bats belonging to Rousettus species. Malsoor is the first Phlebovirus to be isolated from Rousettus bat species. So far, this virus is not known to cause human infections. The virus infects several different mammalian cell types49.
Experimental studies showed pan cytotrophic property of the virus for different mammalian and insect cell lines in vitro. High-resolution transmission electron microscopy studies have been carried out to characterize the fine structure and morphogenesis of this novel Phlebovirus50. Detailed ultrastructural studies on MV particles showed heterogeneous morphology. Majority of the virions (80%) were round, having well-defined envelope projections (6±1 nm) with an average size of 70 nm. A subclass of virions (15%) showed pleomorphism. Interestingly, the envelope projections on the virions were tightly packed and not fragile to staining. Virus-infected cells showed several interesting features not commonly reported for Bunyaviruses. These included frequent detection of multiple inclusion bodies, distinct cytoplasmic membrane-associated virus replication sites and presence of autophagy50. Recently, a human serosurvey was conducted in Mahabaleshwar region (the region from which the virus was first isolated), Maharashtra State, India to detect the presence of anti-Malsoor IgG antibodies, and all the tested samples were found to be negative for the same (NIV unpublished data).
Hantavirus
Hantavirus are a family of rodent-borne viruses (roboviruses) and are responsible for haemorrhagic fever with renal syndrome in Europe and Asia and Hantavirus cardiopulmonary syndrome in America. Hantavirus cases have not been reported from India515253. A pilot study from south India conducted with serum samples obtained from individuals with acute febrile illness and voluntary blood donors indicated 14.7 per cent of samples positive for anti-Hantavirus IgM antibodies5455. This indicated that Hantavirus infections may be present in population and further studies need to be conducted to understand its seroprevalence. In another study, the presence of Hantavirus-specific IgG antibodies was evaluated in 661 individuals. The individuals included tribal population, warehouse workers, patients with chronic renal disease and voluntary blood donors. Nearly 74 per cent of the tested samples were positive for anti-Hantavirus IgG antibodies56. These reports are an indication of Hantavirus prevalence in the country, and further studies need to be conducted to assess the threat of the disease.
Thottapalayam Virus (Tpmv)
TPMV (family Bunyaviridae and genus Hantavirus) was isolated from an Asian house shrew (Suncus murinus) in Tamil Nadu, India2. In fact, this was the first Hantavirus to be isolated in cell culture. Except TPMV, all other known Hantavirus members have been isolated or detected in murid rodents. Whether the shrew (S. murinus) is a primary reservoir or a ‘spillover’ host infected through contact with a primary host is not known. TPMV has also been reported from Nepal57 and China58.
The complete genome sequence analyses of S, M and L segments has confirmed that TPMV is a distinct virus in all the three segments compared to other Hantavirus members. Phylogenetic tree of all the three segments showed that this virus was unique compared to other rodent-borne Hantavirus members (Sigmodontinae, Muridae and Arvicolinae)59.
Many shrew-borne Hantavirus members have been reported from different parts of the world, suggesting that shrews may play a greater role in the ecology and transmission of zoonotic diseases60. Virus sequences were obtained from two Asian house shrews captured in Indonesia60. In addition, anti-TPMV antibodies were detected from a febrile patient from Thailand60. In the light of recent reports of Hantavirus seropositivity, careful surveillance of TPMV is required in different States of India to ascertain whether this virus is involved in causing diseases in humans. The proximity of Asian house shrews with human habitation may result in TPMV infection in humans.
Kaisodi Virus
The Kaisodi virus was isolated from ectoparasite of birds H. turturis, H. spinigera and H. wellingtoni61. This virus was isolated from Kyasanur forest disease (KFD)-affected area (Mysore, Karnataka State). Some cross-reactivity has been observed between Kaisodi and Malayan viruses isolated from Ixodes granulatus61.CF and HI tests confirmed it to be an Arbovirus. No human disease is known so far.
Wanowrie Virus (Wan)
Wanowrie (WAN) virus is an ungrouped Arbovirus having morphogenetic characteristics in common with Bunyavirus. It was isolated for the first time in 1955 from a pool of four adult ticks; Hyalomma marginatum isacci collected from sheep at Wanowrie, near Pune, Maharashtra62, and was subsequently isolated from a human sample. Isolation of the virus was also reported from the human brain suspension at the Virus Research Centre, Pune, in 196662.
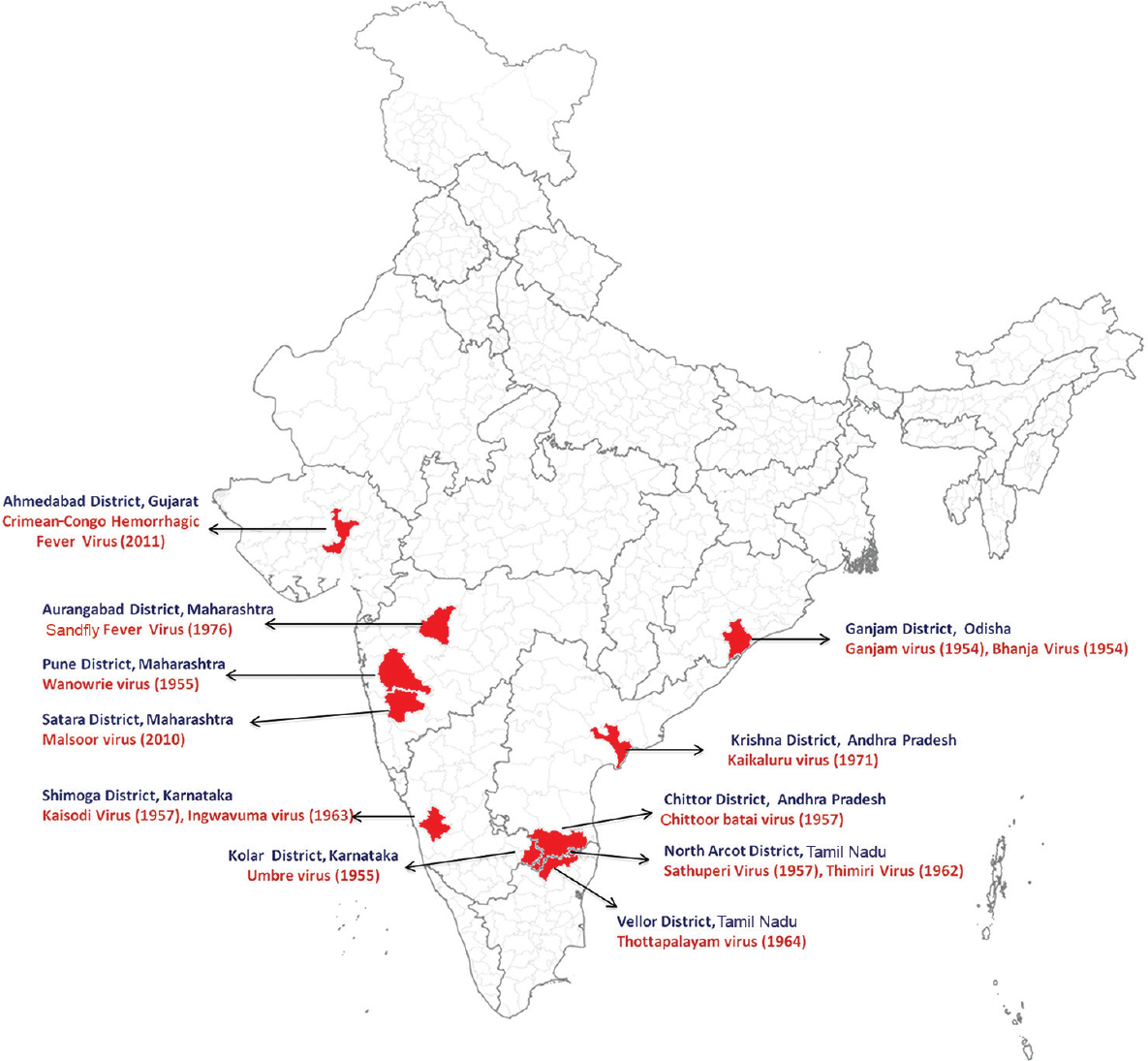
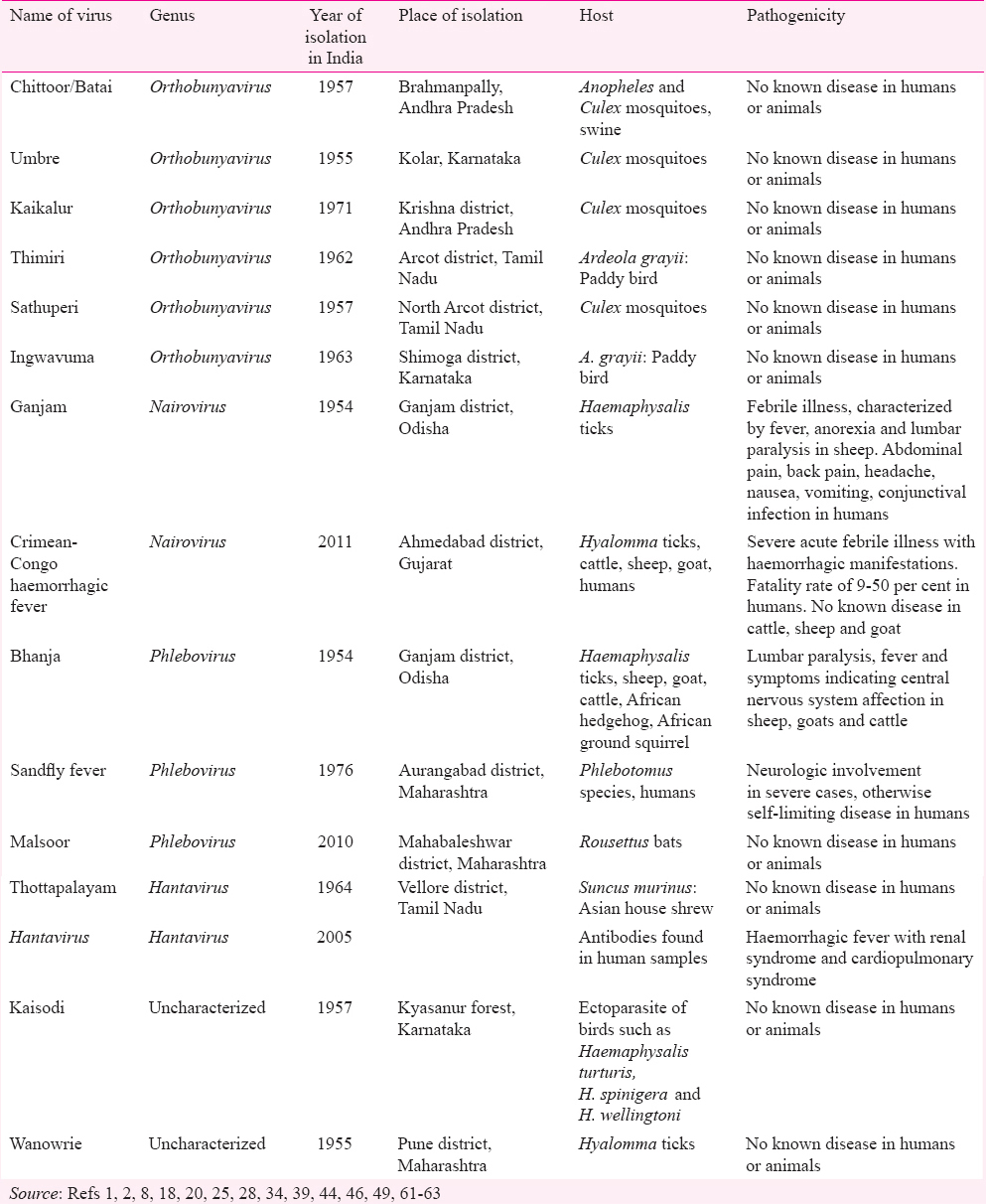
No haemagglutinin was produced, but the virus was sensitive to sodium deoxycholate. Wanowrie virus was pathogenic in suckling mice by the intracerebral and intraperitoneal routes but produced only occasional deaths in adult mice inoculated intracerebrally. The virus was pathogenic for seven day old chick embryos and produced cytopathic effects in Baby Hamster Kidney 21 cell line cultures, but no cytopathic effect or evidence of virus multiplication was elicited in an Ae. albopictus larval cell line. Wanowrie virus had no serological relationship to a very large variety of arboviruses. Only two of the 116 goat serum samples had evidence of neutralizing antibodies against the virus; no antibodies were detected in sheep, cow and buffalo serum62. A brief summary of all Bunyaviruses isolated in India is given in the Table. The Figure shows the places from where these Bunyaviruses were first isolated.
Conclusion
With advanced knowledge and technologies, many viruses have been identified and placed taxonomically in family Bunyaviridae. Under proactive research, the presence of CCHF and MV was detected from humans and animals, respectively43. Several Bunyaviruses are known worldwide for causing severe infections, diseases and mortality in humans and animals. Many of these cause severe economic loss (CCHFV, Rift Valley fever virus, SFTS virus, La Crosse encephalitis virus, etc.). In India, though many Bunyaviruses do not cause disease in humans or animals, their genetic similarity to other disease-causing viruses of the same family is of concern, especially in case of formation of reassortant viruses. On the other side of the spectrum are diseases such as CCHF and sandfly fever which cause severe disease in humans. The clinical signs and symptoms of CCHF are very similar to other viral haemorrhagic fevers such as Omsk haemorrhagic fever, dengue and KFD38. Therefore, proximity to livestock, presence of ticks or travel to endemic regions are factors which play a role in suspecting CCHFV infection. With the CCHF, it is necessary to understand bunyavirus prevalence in India.
Most of the viruses described have been discovered during the 1960s/1970s. With better understanding of biosafety concerns, the work regarding discovery and identification of newer viruses began after the establishment of biosafety level three laboratory (BSL3) at the National Institute of Virology (NIV), Pune, in 200563. Viruses such as CCHFV and MV have been identified in India after the establishment of BSL3 and BSL4. Further systematic searches for identification of viruses are ongoing and are necessary for understanding the emerging infectious diseases and identification of disease hot spots. A special emphasis needs to be laid on exploring animal, bird, arthropod and human viruses.
The current review is an attempt to concisely present information about various Bunyaviruses that were isolated from various insects, birds and animals and are circulating in the country. This information would help in preparedness in case of emergence of novel infections. Timely action could also be taken in case infections from these viruses are seen in either human or animal population. The available information will help not only in making new diagnostic tools but also in monitoring the emergence of diseases.
Conflicts of Interest: None.
References
- Balagodu virus, a new arbovirus isolated from Ardeola grayii (Sykes) in Mysore State, South India. Indian J Med Res. 1969;57:758-64.
- [Google Scholar]
- Thottapalayam virus: A presumptive arbovirus isolated from a shrew in India. Indian J Med Res. 1971;59:1758-60.
- [Google Scholar]
- Virus isolations from mosquitoes collected in North Arcot district, Madras state, and Chittoor district, Andhra Pradesh between November 1955 and October 1957. Indian J Med Res. 1969;57:1420-6.
- [Google Scholar]
- Ganjam virus: A new arbovirus isolated from ticks Haemaphysalis intermedia Warburton and Nuttall, 1909 in Orissa, India. Indian J Med Res. 1969;57:799-804.
- [Google Scholar]
- A neurotropic virus isolated from Aedes mosquitoes caught in the Semliki forest. Am J Trop Med Hyg. 1946;26:189-208.
- [Google Scholar]
- Rapid detection of human pathogenic orthobunyaviruses. J Clin Virol. 2003;41:3299-305.
- [Google Scholar]
- Isolation of Chittoor virus from mosquitoes and demonstration of serological conversions in sera of domestic animals at Manjri, Poona, India. Indian J Med Res. 1966;54:220-4.
- [Google Scholar]
- Isolation of Batai virus from sentinel domestic pig from Kolar district in Karnataka State, India. Acta Virol. 1994;38:239-40.
- [Google Scholar]
- Isolation of Chittoor virus from mosquitoes and demonstration of serological conversions in sera of domestic animals at Manjri, Poona, India. Indian J Med Res. 1966;54:220-4.
- [Google Scholar]
- A new antigenic group of arthropod-borne viruses: The Bunyamwera group. Am J Trop Med Hyg. 1960;9:73-7.
- [Google Scholar]
- The Calovo virus – The second virus isolated from mosquitoes in Czechoslovakia. J Hyg Epidemiol Microbiol Immunol. 1962;6:186-92.
- [Google Scholar]
- Distribution of antibodies reacting with Chittoor virus in humans and domestic ungulates of India. Indian J Med Res. 1966;54:225-8.
- [Google Scholar]
- Batai and Ngari viruses: M segment reassortment and association with severe febrile disease outbreaks in East Africa. J Virol. 2006;80:5627-30.
- [Google Scholar]
- Culex gelidus: An emerging mosquito vector with potential to transmit multiple virus infections. J Vector Borne Dis. 2014;51:251-8.
- [Google Scholar]
- Molecular characterization of Chittoor (Batai) virus isolates from India. Indian J Med Res. 2012;136:792-8.
- [Google Scholar]
- Isolation and complete nucleotide sequence of a Batai virus strain in Inner Mongolia, China. Virol J. 2014;11:138.
- [Google Scholar]
- Characterization of Barmah forest virus: An alphavirus with some unusual properties. Virology. 1984;133:416-26.
- [Google Scholar]
- Kaikalur virus – A new arthropod-borne virus belonging to the Simbu group isolated in India from Culex tritaeniorhynchus (Giles) Indian J Med Res. 1977;66:719-25.
- [Google Scholar]
- Molecular epidemiological analyses of the teratogenic Aino virus based on the sequences of a small RNA segment. Vet Microbiol. 2008;129:40-7.
- [Google Scholar]
- Antigenic relationships among Simbu serogroup (Bunyaviridae) viruses. Am J Trop Med Hyg. 1981;30:1307-18.
- [Google Scholar]
- Developmental disorders of the fetus in some arthropod-borne virus infections. Am J Trop Med Hyg. 1981;30:660-73.
- [Google Scholar]
- Arthrogryposis, hydranencephaly and cerebellar hypoplasia syndrome in neonatal calves resulting from intrauterine infection with Aino virus. Vet Res. 2004;35:531-8.
- [Google Scholar]
- Kammavanpettai, Kannamangalam, Sembalam and Thimiri viruses: Four unrelated new agents isolated from birds in India. Indian J Med Res. 1971;59:1708-11.
- [Google Scholar]
- Phylogeny of the Simbu serogroup of the genus Bunyavirus. J Gen Virol. 2001;82(Pt 9):2173-81.
- [Google Scholar]
- Beran GW, ed. Handbook of Zoonoses (2nd ed). Sec. B. Boca Raton, FL; New York: Viral Zoonoses; CRC Press; 1994.
- Oropouche virus. I. A review of clinical, epidemiological, and ecological findings. Am J Trop Med Hyg. 1981;30:149-60.
- [Google Scholar]
- Genetic reassortment between Sathuperi and Shamonda viruses of the genus Orthobunyavirus in nature: Implications for their genetic relationship to Schmallenberg virus. Arch Virol. 2012;157:1611-6.
- [Google Scholar]
- Ingwavuma strain SA An 4165 isolate. 2006. ICTVdB – The universal virus database, Ver. 4. New York, USA: Columbia University; Available from: http://www.ictvdb.mirror.ac.cn/ICTVdB/index.htm
- [Google Scholar]
- Ingwavuma virus in Thailand. Infection of domestic pigs. Am J Trop Med Hyg. 1974;23:251-7.
- [Google Scholar]
- An annotated checklist of pathogenic microorganisms associated with migratory birds. J Wildl Dis. 2004;40:639-59.
- [Google Scholar]
- Ingwavuma virus (Simbu group) from Culex and Mansonia mosquitoes (Diptera: Culicidae) in Indonesia. J Med Entomol. 1985;22:339-42.
- [Google Scholar]
- Isolation of Ganjam virus from a human case of febrile illness: A report of a laboratory infection and serological survey of human sera from three different states of India. Indian J Med Res. 1969;57:975-82.
- [Google Scholar]
- Isolation of Ganjam virus from ticks collected off domestic animals around Pune, Maharashtra, India. J Med Entomol. 2005;42:204-6.
- [Google Scholar]
- Emerging viral infections with special reference to India. Indian J Med Res. 1996;103:177-200.
- [Google Scholar]
- Genomic analysis reveals Nairobi sheep disease virus to be highly diverse and present in both Africa, and in India in the form of the Ganjam virus variant. Infect Genet Evol. 2011;11:1111-20.
- [Google Scholar]
- Detection, isolation and confirmation of Crimean-Congo hemorrhagic fever virus in human, ticks and animals in Ahmadabad, India, 2010-2011. PLoS Negl Trop Dis. 2012;6:e1653.
- [Google Scholar]
- Genetic characterization and molecular clock analyses of the Crimean-Congo hemorrhagic fever virus from human and ticks in India, 2010-2011. Infect Genet Evol. 2013;14:223-31.
- [Google Scholar]
- First confirmed case of Crimean-Congo haemorrhagic fever from Sirohi district in Rajasthan State, India. Indian J Med Res. 2015;142:489-91.
- [Google Scholar]
- Cross-sectional Serosurvey of Crimean-Congo Hemorrhagic Fever Virus IgG in Livestock, India, 2013-2014. Emerg Infect Dis. 2015;21:1837-9.
- [Google Scholar]
- Bhanja virus: A new arbovirus from ticks Haemaphysalis intermedia Warburton and Nuttall, 1909, in Orissa, India. Indian J Med Res. 1969;57:793-8.
- [Google Scholar]
- Genetic characterization of Bhanja virus and Palma virus, two tick-borne phleboviruses. Virus Genes. 2012;45:311-5.
- [Google Scholar]
- Isolation of Phlebotomus (Sandfly) fever virus from sandflies and humans during the same season in Aurangabad District, Maharashtra State, India. Indian J Med Res. 1976;64:57-63.
- [Google Scholar]
- Clinical and laboratory findings of a sandfly fever Turkey Virus outbreak in Ankara. J Infect. 2011;63:375-81.
- [Google Scholar]
- Malsoor virus, a novel bat phlebovirus, is closely related to severe fever with thrombocytopenia syndrome virus and heartland virus. J Virol. 2014;88:3605-9.
- [Google Scholar]
- Ultrastructure and morphogenesis of malsoor virus: A novel phlebovirus genetically related to the severe fever with thrombocytopenia virus. J Hum Virol Retrovirol. 2015;2:26.
- [Google Scholar]
- Hemorrhagic fever with renal syndrome and other Hantavirus infections. Rev Med Virol. 1994;4:177-84.
- [Google Scholar]
- A pilot study for serological evidence of Hantavirus infection in human population in South India. Indian J Med Res. 2005;122:211-5.
- [Google Scholar]
- First evidence of fatal hantavirus nephropathy in India, mimicking leptospirosis. Nephrol Dial Transplant. 2006;21:826-7.
- [Google Scholar]
- Seroepidemiological study on Hantavirus infections in India. Trans R Soc Trop Med Hyg. 2008;102:70-4.
- [Google Scholar]
- Molecular evolution of Azagny virus, a newfound Hantavirus harbored by the West African pygmy shrew (Crocidura obscurior) in Côte d'Ivoire. Virol J. 2011;8:373.
- [Google Scholar]
- Biodiversity and evolution of Imjin virus and Thottapalayam virus in Crocidurinae shrews in Zhejiang Province, China. Virus Res. 2014;189:114-20.
- [Google Scholar]
- Thottapalayam virus is genetically distant to the rodent-borne Hantaviruses, consistent with its isolation from the Asian house shrew (Suncus murinus) Virol J. 2007;4:80.
- [Google Scholar]
- Development of serological assays for Thottapalayam virus, an insectivore-borne Hantavirus. Clin Vaccine Immunol. 2007;14:173-81.
- [Google Scholar]
- Kaisodi virus, new agent isolation from Haemaphysalis spinigera in Mysore state, South India. Indian J Med Res. 1966;15:961-3.
- [Google Scholar]
- Wanowrie virus: A new arbovirus isolated from Hyalomma marginatum isaaci. Indian J Med Res. 1970;58:985-9.
- [Google Scholar]
- Establishment of Biosafety Level-3 (BSL-3) laboratory: Important criteria to consider while designing, constructing, commissioning & operating the facility in Indian setting. Indian J Med Res. 2014;140:171-83.
- [Google Scholar]