Translate this page into:
A comprehensive yoga programme for weight reduction in children & adolescents with obesity: A randomized controlled trial
For correspondence: Dr Vandana Jain, Department of Pediatrics, Pediatric Endocrinology Division, All India Institute of Medical Sciences, New Delhi 110 029, India e-mail: drvandanajain@aiims.edu
-
Received: ,
This article was originally published by Wolters Kluwer - Medknow and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Background & objectives:
Obesity is a rising pandemic in childhood. There is scarcity of evidence on the efficacy of yoga in achieving weight loss in overweight/obese children. The objective of this study was to assess the efficacy of family-based comprehensive yoga intervention in the reduction of body mass index (BMI) in overweight/obese children, in comparison to standard dietary and lifestyle counselling and control group.
Methods:
This was an open-label randomized controlled study. Children aged 8-15 yr who were overweight or had obesity were randomized to one of the three arms for 18 wk; standard weight management (group 1), yoga with dietary modification (group 2) and control (no intervention; group 3). Reduction in BMI and improvement in physiological, biochemical and psychological parameters from baseline to 18 wk was compared between the three arms. Late follow up was also done at 6-12 months.
Results:
A total of 165 children with mean±standard deviation (SD) age of 11.6±1.8 yr and mean BMI 26.3±4.2 kg/m2 were enrolled. Outcome analysis at 18 wk was performed for 109 children. Improved diet quality and reduced intake were observed in both intervention arms. The median (IQR) reduction in BMI in standard and yoga arms was similar [−1.4 (−3.1, −0.5) kg/m2 and −1.2 (−2.3, −0.6) kg/m2, respectively], while it increased by +0.3 (−0.3, 0.1) in the control arm. In the yoga arm, mean systolic BP reduced from 118 (10) to 114 (8) mmHg, (P=0.019). In the standard arm, significant improvement in psychological scores was noted. In group 3, the mean fasting glucose increased from 93±10 to 102±12 mg/dl (P<0.001).
Interpretation & conclusions:
The findings of the present study suggest that yoga in conjunction with dietary modification is equally effective as the standard weight management for BMI reduction in the paediatric age group.
Keywords
Body mass index
body shape
diet
hypertension
insulin resistance
lifestyle
obesity
weight loss
India has the second-highest number of obese children and adolescents in the world1. Children and adolescents with obesity have a high prevalence of complications such as insulin resistance, dyslipidaemia, hypertension and psychological distress23. Obesity in adolescents tracks into adulthood and is associated with high risk of cardiovascular disease and type 2 diabetes4. Changes in dietary habits and lifestyle, if introduced in formative years are more likely to be sustained and effective, than if introduced later in life.
The current evidence-based management of paediatric obesity is primarily based on diet and lifestyle modifications5. However, their efficacy in achieving the reduction of body mass index (BMI) is not very high5. Parental involvement with the programme is also important in its success6. Many obesity management programmes fail to generate enough enthusiasm in the parents for them to actively encourage and help the child7.
Yoga is the ancient Indian science which emphasizes on the attainment of complete health and well-being through various physical postures (asanas), breathing techniques (pranayama) and meditation8. Yoga has both physiological and psychological benefits in healthy individuals as well as those with various chronic conditions91011. It is also effective in reducing stress12, and improving exercise tolerance1013.
The literature is, however, scarce from the paediatric age group12,14,15, and what is reported either has the limitations of small sample size or inadequate methodology. The present study was hence, undertaken with the objective of assessing the efficacy of a family-based comprehensive yoga intervention of 18 wk duration in achieving reduction in BMI, improvement in cardiometabolic risk profile, and psychological wellbeing in overweight/obese children and adolescents, in comparison to the standard dietary and lifestyle intervention, and a control group with no intervention.
Material & Methods
This was a three armed open-label randomized controlled study (RCT) conducted at the department of Pediatrics, All India Institute of Medical Sciences, New Delhi, India, between May 2016 and February 2019, after approval by the Institute Ethics Committee. The study was registered with the Clinical Trials Registry of India (CTRI/2016/04/006876).
Participant recruitment: Children aged 8-15 yr who were overweight or obese according to Indian BMI charts16 were enrolled, predominantly from the Paediatric OPD but also from families of the hospital staff, and those referred by families of children enrolled in the study. Children with obesity of syndromic or endocrine aetiology, any chronic medical illness, or any complication of obesity for which medications are needed, such as type 2 diabetes and stage 2 hypertension, were excluded. Written informed consent was taken from parents, and assent from the study participants. For each subject, one of the parents was also requested to participate in the study and follow the intervention assigned to the child.
Sample size: The sample size needed for the study was calculated as 37 per group (total n=111), taking a difference in BMI reduction of 1 kg/m2 between the groups as clinically relevant, with common standard deviation (SD) of 0.5 kg/m2, α as 0.05 and power as 90 per cent. Considering that high attrition has been reported in previous paediatric weight reduction trials17, we planned to enrol up to 50 per cent more subjects and in a 3:3:2 ratio, with a smaller number of subjects in the non-intervention arm.
Baseline evaluation of the subjects: Age, gender, socioeconomic and family history were recorded. Dietary assessment was done using a semi-quantitative food frequency questionnaire by the study dieticians18. The intake of various macro- and micro-nutrients was calculated by DietSoft nutrient calculator software (https://dietsoft.in/), based on the nutritive value of Indian foods19.
Height was measured using a stadiometer (Seca 213, Hamburg, Germany) and weight using an electronic scale (Seca 874dr, Hamburg, Germany) to an accuracy of 0.1 cm and 0.1 Kg, respectively, and BMI was calculated. Waist circumference (WC) was measured using a non-stretchable tape according to WHO guidelines20. Central adiposity was considered present if WC was >+2 Z score based on Indian reference ranges16, or more than the adult cut-offs of 90 and 80 cm for Asian males and females21, respectively. Blood pressure (BP) was measured three times after a 10 min rest, using an automated instrument (Omron HEM-7203, Kyoto, Japan) with appropriate sized cuff, in the seated position, and the two readings closest to each other were averaged. Hypertension was diagnosed as BP ≥95th centile or ≥130/80 (whichever was lower) for children under 13 yr and ≥130/80 in adolescents >13 yr of age22. Heart rate was measured at rest and after exercise using the 3 min Kasch Pulse Recovery test. During this, the participant climbed up and down a 12 inches step 24 times/min to the beat of a metronome set at 96 beats/min for three minutes. One minute after the test, the carotid pulse rate was counted for 30 sec in the seated position using a stopwatch23.
Fasting venous sample was obtained after a 12 h overnight fast for estimation of glucose, insulin, triglycerides (TG), total cholesterol (TC) and high-density lipoprotein cholesterol (HDL) levels. Subjects were asked to collect saliva by passive drooling about half an hour after waking up in the morning (after rinsing the mouth, and not eating/drinking anything other than water) and bring it with them. Glucose, TG, TC and HDL were estimated by clinical chemistry analyzer (Roche Cobas 6000, Roche Diagnostics, GmbH, Germany) and serum insulin and salivary cortisol by electrochemiluminescence (Roche Cobas e411, Roche Diagnostics, GmbH, Germany). Homeostatic model assessment of insulin resistance (HOMA-IR) was calculated as fasting insulin (µU/ml) × fasting glucose (mg/dl)/40524. Fasting glucose was considered impaired if ≥100 and <126 mg/dl25 and HOMA-IR was considered high if > 2.526. Age appropriate cut-offs were used to define abnormal values for TG, total, LDL and HDL cholesterol2728. Salivary cortisol >0.65 mcg/dl was considered as suggestive of stress29.
Three validated psychological questionnaires were used, Kindl R for assessing health-related quality of life (QoL)30, Body Shape Questionnaire-16 (BSQ) for assessing concern over physical appearance31, and Cohen’s Perceived Stress Scale (PSS) for assessing stress levels32. These were administered under the guidance of a clinical psychologist (RS).
Kindl R has 24 items and score <45 indicate suboptimal QoL30. BSQ has 16 items, with possible score from 16 to 96. Scores between 38-51, 52-66 and > 66 indicate mild, moderate and marked concern for shape, respectively31. PSS is a 10 item scale with possible score from 0 to 40. Scores < 13, 14-26 and >26 indicate low, moderate and high perceived stress, respectively32.
Randomization into groups: Subjects were randomized using stratified randomization using a computer-generated sequence according to age group (above or below 12 yr) and gender into one of the three groups for 18 wk. Randomization sequence was generated by a biostatistician (not a part of the study team). Group allocation was done by the study dietician (AS) at enrolment, based on the slip picked by the subject from the container according to his/her gender and age group.
Group 1 - Standard weight management group: Children and their parents were counselled by the study dieticians and individualized diet charts were given, with total caloric intake lower than the recommended dietary allowance for age and gender by 15-25 per cent (depending on BMI and physical activity level). Emphasis was laid on regular and balanced meals, increased intake of water, fiber, fruits and vegetables, and avoidance of sugar-sweetened beverages and processed foods. They were advised to undertake at least an hour of moderate-to-vigorous physical activity daily, have adequate sleep and restrict sedentary pursuits, especially screen time. A colourful printed booklet in Hindi was given educating them about healthy food choices and physical activity.
Group 2 - Comprehensive yoga programme group: This group also received detailed dietary counselling, advice on adequate sleep and restriction of sedentary pursuits as in group 1. In addition, they were enrolled in an intensive yoga programme, designed by yoga experts and previously validated at Integral Health Clinic (IHC), AIIMS, New Delhi9. The asanas and pranayama included in the protocol are summarized in Table I. There was an intensive phase during which subjects and participating parents had to attend a minimum of three but preferably five classes per week for two weeks at IHC. From wk 3 to 6, one class per wk, and from week seven to 18, one class every four weeks had to be attended. Classes of two hour duration were held daily by the yoga instructor employed for the study, and the time was adjusted according to the convenience of the families. From third week onwards, subjects were asked to practice yoga at home at least five times per week for an hour. Parents were asked to maintain a log. A compact disc with a video and a booklet (both prepared especially for the study) with detailed instructions for all asanas and pranayams in the study protocol were given to the subjects.
| 1. Humming in meditative posture: Vajrasana, padmasana or Sukhasana (5-10 min) |
| 2. Loosening exercises from head to toes: 3-5 repetitions on each side (5-10 min) |
| 3. Surya Namaskar |
| Standing: Ardhakatichakrasana, Padahastasana, Ardhachakrasana, Vrikshasana |
| Sitting: Konasana, Naukasana, Paschimotanasana |
| Lying prone: Dhanurasana, Makarasana, Bhujangasana |
| Lying supine: Uttitapadasana, Sarvangasana, Halasana |
| Starting with 2-3 repetitions, holding each pose up to 60 sec, gradually increasing to 10-15 repetitions (40-50 min) |
| 4. Pranayama (breathing exercises): 15-20 times each |
| 5. Relaxation in shavasana (5 min) |
Group 3 - Control (waitlisted) group: No specific physical activity/lifestyle counselling was provided to subjects in this group. After outcome analysis at 18 wk, they were given dietary and lifestyle counselling and also offered yoga training.
Measures to ensure compliance and reduce drop-outs: The dieticians maintained weekly telephonic contact with groups 1 and 2 subjects and the yoga teacher with group 2 subjects till 18 wk to motivate them and resolve queries. Follow up visits were scheduled at six and 12 wk to emphasize compliance. Group sessions were held separately for families in groups 1 and 2 to reinforce the advice using interactive games and quizzes. Families shared healthy recipes and the stories of their efforts. Small gifts (badminton rackets, skipping ropes, exercise mats, slogan tees, etc.) were given as incentives to children. Children in groups 1 and 3 were offered yoga training after study completion as an incentive to maintain participation.
Assessment of compliance till 18 wk: Compliance with dietary advice was assessed in both groups 1 and 2 by the dietician. Detailed assessment of the dietary intake was made at baseline and 18 wk. In group 2, compliance with yoga protocol was adjudged by: (i) percentage of classes attended out of maximum 17 (10 in intensive phase, 4 in weekly and 3 in monthly sessions); and (ii) regularity of yoga practice at home score of 0 was assigned if the practice was done for 0-2 days/wk, the score of 1 if practice done for 3-4 days/wk, and score of 2 if practice done for 5-7 days/wk. The scores for each week between the 3rd and 18th wks were added and expressed as percentage of the maximum possible score of 32. The final score was the average of these two percentage scores.
Outcomes: The primary outcome was the comparison of the change in BMI from baseline to 18 wk between the three groups. The secondary outcomes were comparisons of change in WC, BP, resting and post-exercise heart rate, biochemical parameters and the scores on psychological questionnaires from baseline to 18 wk. In addition, the persistence of the reduction in BMI was assessed at delayed follow up done between six and 12 months for the children in groups 1 and 2.
Statistical analysis: Data were analyzed by Stata 12.1 (Stata Corp 4905 College Station, Texas, USA). The categorical data are presented as frequency (percentage) and continuous data as mean±SD or median (interquartile range), as appropriate. Paired t test was done to assess the treatment effect within the groups from baseline to 18 wk. To assess the statistical significance of the difference in outcomes across the three study groups, the ANCOVA model was run with appropriate covariates and confounders. ANOVA model followed by Bonferroni adjustment was used to compare the change from baseline to 18 wk across the three intervention groups. Repeated measure ANOVA was also used to assess the sustainability of treatment effect at late follow up. Kruskal-Wallis or rank-sum tests were used for non-parametric data. Two-sided P<0.05 was considered significant.
Results
A total of 165 overweight/obese children (112 boys), with mean±SD age of 11.6±1.8 yr and mean BMI and BMI Z score of 26.3±4.2 and 1.8±0.7 kg/m2, respectively, were enrolled. At baseline, the mean systolic and diastolic BP of the enrolled subjects were 117±10 and 71±8 mmHg, respectively; mean fasting blood sugar was 92.3±12.7 mg/dl, and mean serum insulin and HOMA-IR were 15.1±10.6 mIU/l and 3.4±2.6, respectively. The mean serum triglyceride level was 127.7±55.7 mg/dl; and mean total, LDL and HDL cholesterol were 155.3±41.0, 88.4±34.3 and 41.0±11.7 mg/dl, respectively. Central obesity was present in 50 per cent, stage 1 hypertension in 26 per cent, impaired fasting glucose in 24 per cent, fasting hyperinsulinaemia in 37 per cent, elevated HOMA-IR in 45 per cent, elevated serum triglyceride, total and LDL cholesterol were present in 28, 13 and eight per cent, respectively, while low HDL was the most common dyslipidaemia, present in 50 per cent of the participants. The median (IQR) salivary cortisol was 0.07 (0.04, 0.17), with elevated level in five per cent. The mean score on Kindl QoL, PSS and BSQ were 84.8±11.5, 47.6±16.1 and 20.4±6.5, respectively. PSS score > 26 indicating high perceived stress, and BSQ score > 66 indicating marked concern with body shape were present in 17.6 and 17.4 per cent, respectively, while none of the subjects had low scores on QoL.
Fifty nine, 63 and 43 subjects were randomized to groups 1, 2 and 3, respectively. Table II presents the baseline clinical and anthropometric parameters of the subjects in the three groups. Primary outcome analysis at 18 wk could be done for 40, 41 and 28 subjects (total 109), with the total attrition being 34 per cent. Drop-out rate was similar in all the three groups. Delayed follow up (planned only for group 1 and 2) was done for 80 subjects out of the 81 for whom primary outcome analysis was done, at the median time of 8.3 (6.5, 13.5) months. The study flow chart is presented in the Figure, showing the reasons for attrition and the numbers for whom the results of various outcome parameters were available.
| Variables | Group 1 (standard weight management) | Group 2 (comprehensive yoga programme) | Group 3 (control) |
|---|---|---|---|
| n | 59 | 63 | 43 |
| Age (yr) | 11.5±1.9 | 11.7±1.7 | 11.4±1.8 |
| Male/female (n) | 38/21 | 43/20 | 31/12 |
| Weight (kg) | 56.8±13.6 | 58.9±16.6 | 54.5±12.6 |
| Height (cm) | 145.9±11.5 | 147.0±10.9 | 145.4±10.4 |
| BMI (kg/m2) | 26.3±3.6 | 26.8±4.7 | 25.8±3.9 |
| BMI Z score | 1.8±0.6 | 1.8±0.6 | 1.7±0.6 |
| Pubertal status (n) | |||
| Early/mid/late pubertal | 21/26/12 | 23/31/09 | 20/18/04 |
| Waist circumference (cm) | |||
| Girls | 84.6±9.4 | 89.6±13.7 | 85.5±10.9 |
| Boys | 84.3±8.6 | 88.9±10.9 | 85.2±10.2 |
| Central adiposity#, n (%) | 26 (44) | 37 (59) | 19 (44) |
| Parent’s BMI (kg/m2) | |||
| Mothers | 30.8±5.1 (n=41) | 29.9±4.9 (n=51) | 30.0±4.7 (n=32) |
| Fathers | 25.8±3.8 (n=17) | 30±1.7 (n=9) | 27.5±4.9 (n=6) |
| Resting HR (per min) | 83±9 | 84±9 | 84±11 |
| Post-exercise HR (per min) | 118±15 | 119±14 | 119±15 |
| Systolic BP (mm Hg) | 115±10 | 119±10 | 115±9 |
| Diastolic BP (mm Hg) | 70±7 | 72±9 | 72±8 |
| Hypertension, n (%) | 10 (17) | 24 (38) | 9 (21) |
#WC >2 SD for age and gender, or >90 cm in boys or >80 cm in girls; Data are presented as mean±SD unless specified. BMI, body mass index; HR, heart rate; BP, blood pressure; SD, standard deviation; WC, waist circumference
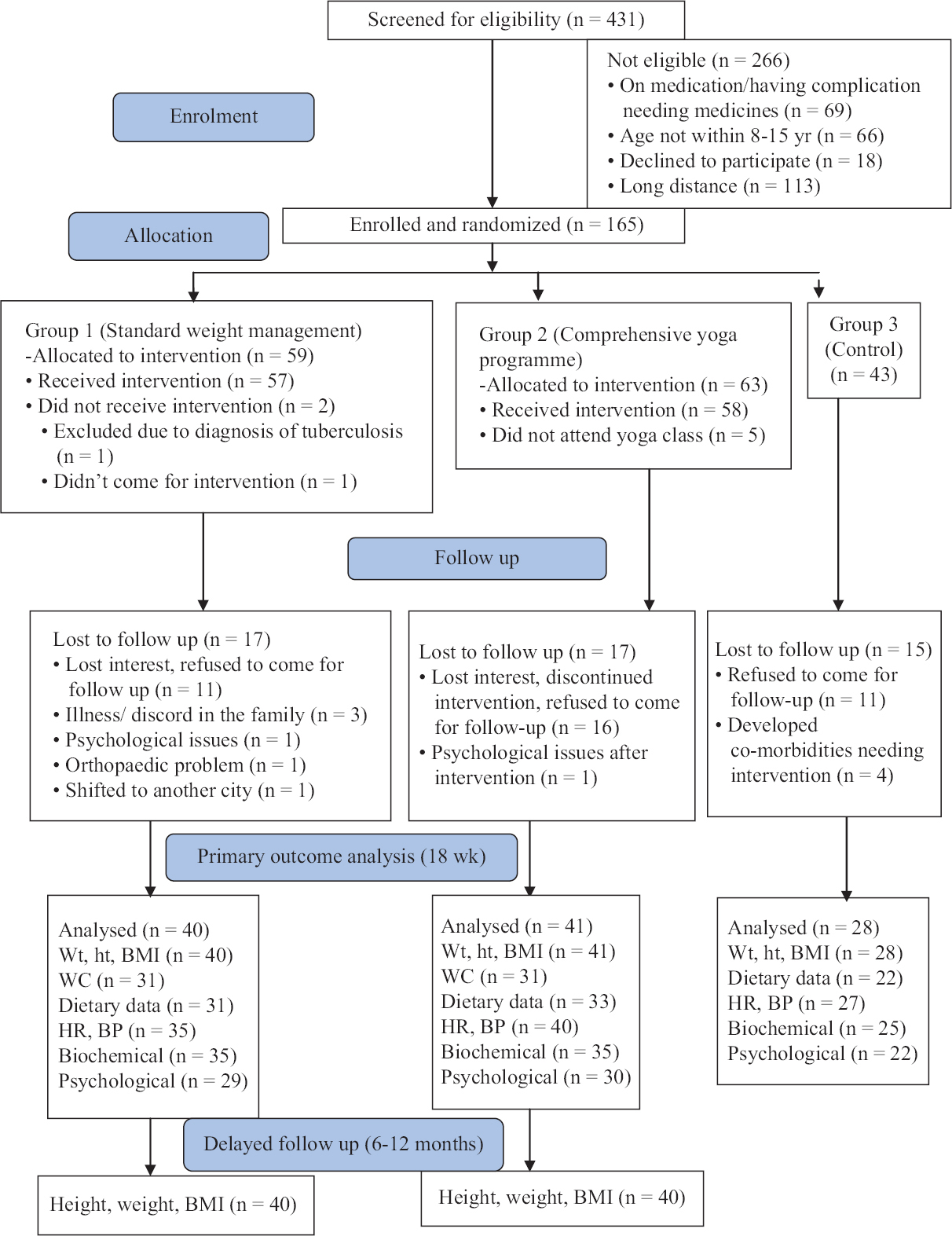
- Consolidated Standards of Reporting Trials diagram. Ht, Height; Wt, Weight; BMI, body mass index; WC, waist circumference; HR, heart rate; BP, blood pressure.
Table III presents the group-wise comparison of calorie and nutrient intake at baseline and 18 wk for all the subjects for whom detailed dietary assessment had been done at both these time points. Significant reduction in caloric intake and improvement in diet quality with increased fibre content, and reduced saturated fat, and free sugar intake was noted for subjects in both the intervention groups, indicating a good uptake of the dietary advice; while in group 3, there was no significant decrease in caloric intake.
| Variables | Mean daily intake at baseline | Mean daily intake at 18 wk |
|---|---|---|
| Group 1 (standard weight management, n=31) | ||
| Energyϯ | 2230±562 | 1602±329*** |
| Protein | 62±18 | 61±15 |
| Fat | 87±33 | 42±13*** |
| Saturated fatty acids | 22±13 | 7±7*** |
| Carbohydrate | 290±66 | 235±54*** |
| Sucrose | 29±18 | 9±7*** |
| Free sugar | 61±41 | 26±14*** |
| Fibre | 38±12 | 51±16*** |
| Group 2 (comprehensive yoga programme, n=33) | ||
| Energyϯ | 2432±486 | 1690±346*** |
| Protein | 69±17 | 69±16 |
| Fat | 87±26 | 40±17*** |
| Saturated fatty acids | 18±11 | 7±6*** |
| Carbohydrate | 327±83 | 248±55*** |
| Sucrose | 29±18 | 9±7*** |
| Free sugar | 61±33 | 23±9*** |
| Fibre | 42±17 | 54±16*** |
| Group 3 (control n=22) | ||
| Energyϯ | 2591±634 | 2210±583 |
| Protein | 69±21 | 64±16 |
| Fat | 95±31 | 81±34 |
| Saturated fatty acids | 19±11 | 21±11 |
| Carbohydrate | 320±85 | 289±66 |
| Sucrose | 37±28 | 25±14* |
| Free sugar | 72±44 | 35±20*** |
| Fibre | 38±12 | 39±8 |
ϯRepresents values in kcal per day; rest all values in grams per day. P *<0.05, ***<0.001. Paired t test was applied to compare the mean daily intakes at baseline and 18 wk for those subjects in whom intakes were recorded at both time points
The mean±SD number of yoga classes attended was 14±3, number of days/wk on which yoga practice at home was done was 3±1 and the yoga compliance score was 67±17 per cent. The reasons for missing classes and home practise included not enjoying yoga, practical difficulty and dependence on parents for coming to IHC for classes, and sub-optimal involvement of the parents. Subjects’ age, gender and BMI were not found to have any effect on compliance score. However, the compliance score was found to have a significant effect on the reduction of BMI between 18 wk and baseline by regression analysis (β 0.05, P<0.001). The mean reduction in BMI of subjects in the highest, intermediate and lowest tertiles of compliance score were 2.5±1.1, 1.2±0.8 and 0.6±0.5 kg/m2 (P<0.001), respectively.
Table IV presents the comparison of the change in BMI, BMI Z score, weight, and WC from baseline to 18 wk for all the three groups, and from baseline to late follow up in groups 1 and 2. Subjects in both the intervention groups had a similar reduction in median BMI, weight and WC between baseline and 18 wk, while these parameters increased in the control group during the same period. The mean BMI and BMI Z score at late follow up were 24.2±3.8 kg/m2 and 1.4±0.6 for group 1, and 25.2±4.8 kg/m2 and 1.5±0.7 for group 2 subjects. Repeated measures ANOVA showed that the reduction in BMI and BMI Z score was significant (P<0.001) for subjects in both the intervention groups over the three time periods. BMI reduction of ≥1 kg/m2 from baseline to 18 wk was seen in 25 (62.5%) subjects in group 1, 24 (60%) subjects in group 2, and in none of the subjects in group 3.
| Parameter | Time | Group 1 (standard) (n=40) | Group 2 (yoga) (n=41) | Group 3 (control) (n=28) | P1 | P2 | P3 |
|---|---|---|---|---|---|---|---|
| BMI (kg/m2) | Baseline | 26.4±3.4 | 26.8±4.8 | 26.4±3.8 | <0.001 | <0.001b, c | <0.001 |
| 18 wk | 24.6±4.0 | 25.4±4.7 | 26.8±4.0 | ||||
| Δ 0-18* | −1.4 (−3.1-−0.5) | −1.2 (−2.3-−0.6) | +0.3 (−0.3-0.1) | ||||
| BMI Z | Baseline | 1.8±0.6 | 1.8±0.6 | 1.9±0.6 | <0.001 | <0.001b, c | <0.001 |
| 18 wk | 1.4±0.6 | 1.5±0.7 | 1.9±0.6 | ||||
| Δ 0-18* | −0.4 (−0.7-−0.2) | −0.3 (−0.4-−0.2) | 0.0 (−0.1-0.1) | ||||
| Weight (kg) | Baseline | 57.3±12.8 | 58.4±15.1 | 57.4±13.3 | <0.001 | <0.001b | <0.001 |
| 18 wk | 54.6±13 | 57.3±14.9 | 59.6±13.3 | ||||
| Δ 0-18* | −1.8 (−5.0-0.4) | −0.9 (−3.2-0.6) | +2.5 (1.5-3.7) | ||||
| WC (cm) | Baseline | 85.5±9.1 | 88.4±11.7 | 87.5±9.9 | 0.008 | 0.012b | 0.007 |
| 18 wk | 81.9±11.4 | 85.7±11.5 | 88.4±9.3 | ||||
| Δ 0-18* | −3.9 (−7.5-−0.5) | −4.0 (−6.3-0.5) | +2.6 (−2.2-5.0) | ||||
| Change from baseline to late follow up (6-12 months) | |||||||
| Parameter | Group 1 (n=40) | Group 2 (n=40) | P4 | ||||
| BMI (kg/m2 Δ 0-L)* | −1.7 (−2.9-−0.5) | −1.1 (−2.8-−0.01) | 0.305 | ||||
| BMI Z (Δ 0-L)* | −0.3 (−0.5-−0.1) | −0.2 (−0.4-0.0) | 0.281 | ||||
| Weight (kg Δ 0-L)* | −1.6 (−4.7-1.6) | −0.1 (−3.0-2.4) | 0.190 | ||||
*Expressed as median (IQR); rest of the values expressed as mean±SD. Δ 0-18, Change in the parameter between baseline and 18 wk (i.e.; 18-wk value - baseline value) and Δ 0-L, Change in the parameter between baseline and late follow up; P1, ANCOVA was applied to compare the mean values in the three groups at 18 wk adjusting for baseline values of the respective parameters; age and gender; P2, ANOVA was applied to compare the mean change in each anthropometric parameter between baseline and 18 wk; followed by Bonferroni correction for pairwise comparisons (aGroup 1 vs. 2; bGroup 1 vs. 3; cGroup 2 vs. 3); P3, Kruskal–Wallis test was used to compare median Δ 0-18; P4, Rank–sum test applied to compare Δ 0-L. BMI, body mass index; BMI Z, BMI Z score; WC, waist circumference; SD, standard deviation; IQR, interquartile range
At late follow up, BMI reduction of ≥1 kg/m2 from baseline was present in 26 (65%) and 23 (57%) of the subjects in groups 1 and 2, respectively.
The results for some of the secondary objectives are presented in Table V. There was a significant reduction in systolic BP from baseline to 18 wk in group 2 subjects. The psychological scores showed a significant improvement only in group 1 subjects. None of the three groups showed a significant change in the salivary cortisol between baseline and 18 wk. No significant improvement was noted in the mean levels of any of the biochemical parameters in either group 1 or 2 (data not shown). In group 2, a significant decline in the percentage of children with elevated HOMA-IR was seen (66.7 to 40.7%, P=0.050). In group 3, the mean fasting glucose increased from 93.0±10.5 to 102.0±12.4 mg/dl (P<0.001), and the proportion with impaired fasting glucose from 20 to 65 per cent (P=0.004) from baseline to 18 wk.
| Physiological parameters | ||||||||
|---|---|---|---|---|---|---|---|---|
| Study groups | Resting HR (per min) | Post-exercise HR (per min) | Systolic BP (mm Hg) | Diastolic BP (mm Hg) | ||||
| Baseline | 18 wk | Baseline | 18 wk | Baseline | 18 wk | Baseline | 18 wk | |
| Group 1 (n=35) | 85±9 | 79±9 | 118±14 | 117±10 | 114±9 | 116±10 | 70±8 | 70±6 |
| Group 2 (n=40) | 84±9 | 81±8 | 119±15 | 116±9 | 118±10 | 114±8* | 73±10 | 71±7 |
| Group 3 (n=27) | 86±12 | 79±9* | 122±16 | 116±10 | 118±9 | 116±8 | 73±8 | 75±9 |
| Psychological parameters | ||||||||
| Study groups | Stress score | BSQ score | Kindl QoL | |||||
| Baseline | 18 wk | Baseline | 18 wk | Baseline | 18 wk | |||
| Group 1 (n=29) | 20.1±6.4 | 16.5±5.3** | 42.8±16.0 | 35.0±13.9* | 85.2±10.5 | 90.6±10.4* | ||
| Group 2 (n=30) | 19.2±5.0 | 17.5±5.8 | 46.0±17.0 | 43.2±16.6 | 84.8±12.3 | 86.0±13.2 | ||
| Group 3 (n=22) | 20.5±7.6 | 17.2±0.6 | 54.5±15.5 | 48.1±4.4 | 85.7±14.2 | 86.1±14.7 | ||
The values with significant difference between baseline and 18 wk (by paired t test) are marked by asterisks; P *<0.05, **<0.01. BSQ, body shape questionnaire; Kindl QoL, Kindl R questionnaire for assessing health-related quality of life
Discussion
We believe that the present study was the first RCT on the efficacy of a programme based on yoga and dietary modification in achieving reduction of BMI and improvement of various physiological, biochemical and psychological parameters in overweight/obese children from India. It was found to be as effective as the standard weight management strategies in achieving reduction in BMI Z score sustained over a median follow up duration of eight months. The attrition rate in our study was comparable to that reported previously in other paediatric weight loss RCTs7,17,33-35. The compliance with dietary counselling was good as seen by the significant reduction in caloric intake and improvement in diet quality seen in both the intervention groups. The compliance with yoga protocol, including attendance for classes as well as regularity of home practise was variable, and this had a bearing on the benefit derived from it. The subjects in the highest tertile of compliance had a mean reduction in BMI of 2.5 kg/m2, which was higher than that reported by previous paediatric dietary and lifestyle modification programmes7,33-35, thus illustrating the efficacy of the study protocol. The median decline in BMI in groups 1 and 2 was 1.4 kg/m2 and 1.2 kg/m2, respectively, and median reduction in WC was about 4 cm. In comparison, the children in control arm had a median weight gain of 2.5 kg and increase in WC by 2.6 cm, representing the natural course of obesity. In addition, a significant decline in systolic BP and prevalence of elevated HOMA-IR was observed in the children in the yoga arm, and significant improvement in psychological parameters in group 1; while the mean fasting glucose increased significantly in group 3.
So far, to the best of our knowledge, there is no RCT from India evaluating strategies for BMI reduction in children. A non-randomized study from Pune, found that school based interventions had no effect on BMI but led to improvement in lifestyle and fitness levels among children in the intervention arm36. In an RCT conducted in the UK, the median change in BMI Z score of only −0.005 and −0.114, respectively, were noted in overweight/obese children randomised to either a family-based intervention or usual care, with 28 per cent attrition7. In a Malaysian paediatric study focussing on diet and exercise, there was no reduction in weight; however, the weight gain was lower in intervention group compared to control35. In an Australian RCT, comparing parenting skills plus healthy lifestyle, or healthy lifestyle alone, median reduction in BMI Z score was 0.26 (similar in both arms), with 37 per cent attrition33. In Iranian adolescent girls with obesity, BMI change of −1.07 kg/m2 was observed in the diet and lifestyle arm, vs. +0.24 kg/m2 in the control arm34. Overall, the findings of these studies are in alignment with our study in terms of the percentage of children who completed the study, the magnitude of reduction in BMI, and the non-significant differences between the different interventions as long as dietary modification was done as part of the intervention. There are only a few studies on the efficacy for yoga for weight loss in children. In one study from Texas, USA, in which 20 children and adolescents participated in a 12 wk Ashtanga yoga programme, of these, 14 children aged 8-15 yr, completed the programme, and had an average weight loss of 2 kg12.
The present study assessed not only weight loss but also changes in several psychological, physiological and metabolic parameters. However, the limitations were that there was attrition, many children did not attend all the yoga sessions, and did not adhere to the guidelines for home-based yoga practice, with parents’ involvement also being sub-optimal. The other limitation was that few biochemical, physiological and psychological outcome variables were not available for all the participants, and those with missing values had to be excluded from the analysis.
Overall, the present study demonstrated that yoga in conjunction with dietary modification is effective in reduction of BMI, systolic BP and prevalence of insulin resistance in overweight/obese children. However, its efficacy in reduction of BMI was not superior to that of an efficiently delivered dietary and lifestyle intervention. Further studies with focus on enhancing the compliance to yoga by making the classes more enjoyable and accessible, will be helpful in bringing out the true potential of yoga in improving the health and well being in overweight/obese children.
Acknowledgment
The authors acknowledge Ms Babita Upadhyaya and Kajal Chauhan, project dieticians, department of Pediatrics, AIIMS, New Delhi, for help with subject enrolment and dietary assessment, and Aman Agarwal, biostatistician, CIMR, AIIMS, Delhi, for help with statistical analysis.
Financial support & sponsorship: This study was supported by a grant from Ministry of AYUSH, Government of India (Grant No. Z28015/257/2015/HPC (EMR)-A AYUSH-B).
Conflicts of Interest: None.
References
- Health effects of overweight and obesity in 195 countries over 25 years. N Engl J Med. 2017;377:13-27.
- [Google Scholar]
- Prevalence of metabolic syndrome in adolescents from a north Indian population. Diabet Med. 2007;24:195-9.
- [Google Scholar]
- Prevalence, clinical &biochemical correlates of non-alcoholic fatty liver disease in overweight adolescents. Indian J Med Res. 2018;148:291-301.
- [Google Scholar]
- Tracking of childhood overweight into adulthood:A systematic review of the literature. Obes Rev. 2008;9:474-88.
- [Google Scholar]
- Pediatric obesity-assessment, treatment, and prevention:An endocrine society clinical practice guideline. J Clin Endocrinol Metab. 2017;102:709-57.
- [Google Scholar]
- Family-based behavioral treatment for childhood obesity:Caretaker-reported barriers and facilitators. Ochsner J. 2017;17:83-92.
- [Google Scholar]
- Randomised controlled trial evaluating the effectiveness and cost-effectiveness of 'Families for Health', a family-based childhood obesity treatment intervention delivered in a community setting for ages 6 to 11 years. Health Technol Assess. 2017;21:1-180.
- [Google Scholar]
- A brief but comprehensive lifestyle education program based on yoga reduces risk factors for cardiovascular disease and diabetes mellitus. J Altern Complement Med. 2005;11:267-74.
- [Google Scholar]
- Modulation of cardiovascular response to exercise by yoga training. Indian J Physiol Pharmacol. 2004;48:461-5.
- [Google Scholar]
- A review of yoga programs for four leading risk factors of chronic diseases. Evid Based Complement Alternat Med. 2007;4:487-91.
- [Google Scholar]
- Ashtanga yoga for children and adolescents for weight management and psychological well being:An uncontrolled open pilot study. Complement Ther Clin Pract. 2009;15:110-4.
- [Google Scholar]
- Study of some physiological and biochemical parameters in subjects undergoing yogic training. Indian J Med Res 1981:74-120.
- [Google Scholar]
- Therapeutic effects of yoga for children:A systematic review of the literature. Pediatr Phys Ther 200820:66-80.
- [Google Scholar]
- Clinical applications of yoga for the pediatric population:A systematic review. Acad Pediatr. 2009;9:212-20.e1.
- [Google Scholar]
- Revised IAP growth charts for height, weight and body mass index for 5- to 18-year-old Indian children. Indian Pediatr. 2015;52:47-55.
- [Google Scholar]
- Attrition in paediatric weight management:A review of the literature and new directions. Obes Rev. 2011;12:e273-81.
- [Google Scholar]
- Development and evaluation of a semi-quantitative food frequency questionnaire for use in urban and rural India. Asia Pac J Clin Nutr. 2012;21:355-60.
- [Google Scholar]
- Indian Council of Medical Research. National Institute of Nutrition. In: Nutrient requirements and recommended dietary allowances for Indians. Hyderabad: ICMR-NIN; 2010.
- [Google Scholar]
- WHO STEPwise approach to chronic disease risk factor surveillance. Geneva: WHO; 2005.
- Metabolic syndrome –A new world-wide definition. A Consensus Statement from the International Diabetes Federation. Diabet Med. 2006;23:469-80.
- [Google Scholar]
- Subcommittee on screening and management of high blood pressure in children. Clinical practice guideline for screening and management of high blood pressure in children and adolescents. Pediatrics. 2017;140:e20171904.
- [Google Scholar]
- Cardiorespiratory fitness in children:A simple screening test for population studies. Pediatr Cardiol. 2015;36:27-32.
- [Google Scholar]
- Homeostasis model assessment:Insulin resistance and beta-cell function from fasting plasma glucose and insulin concentrations in man. Diabetologia. 1985;28:412-9.
- [Google Scholar]
- American Diabetes Association. Diagnosis and classification of diabetes mellitus. Diabetes Care. 2014;37(Suppl 1):S81-90.
- [Google Scholar]
- A study of insulin resistance by HOMA-IR and its cut-off value to identify metabolic syndrome in urban Indian adolescents. J Clin Res Pediatr Endocrinol. 2013;5:245-51.
- [Google Scholar]
- International diabetic federation:Criterion of metabolic syndrome in children and adolescents. J Pediatr. 2004;145:439-44.
- [Google Scholar]
- American Academy of Pediatrics. National Cholesterol Education program report of the expert panel on blood cholesterol levels in children and adolescents. Pediatrics. 1992;89:525-84.
- [Google Scholar]
- Determination of salivary cortisol in healthy children and adolescents. Acta Medica Iranica. 2005;43:32-6.
- [Google Scholar]
- Assessing health-related quality of life in chronically ill children with the German KINDL:First psychometric and content analytical results. Qual Life Res. 1998;7:399-407.
- [Google Scholar]
- Body shape questionnaire:Derivation of shortened “alternate forms”. Int J Eat Disord. 1993;13:315-21.
- [Google Scholar]
- A parent-led family-focused treatment program for overweight children aged 5 to 9 years:The PEACH RCT. Pediatrics. 2011;127:214-22.
- [Google Scholar]
- Effect of dietary behaviour modification on anthropometric indices and eating behaviour in obese adolescent girls. J Adv Nurs. 2009;65:1670-5.
- [Google Scholar]
- Randomized controlled trial of a good practice approach to treatment of childhood obesity in Malaysia:Malaysian Childhood Obesity Treatment Trial (MASCOT) Int J Pediatr Obes. 2011;6:e62-9.
- [Google Scholar]
- Effectiveness of a 5-year school-based intervention programme to reduce adiposity and improve fitness and lifestyle in Indian children;the SYM-KEM study. Arch Dis Child. 2016;101:33-41.
- [Google Scholar]






