Translate this page into:
Kimura's disease: A diagnostic dilemma
*For correspondence: navin2k1@gmail.com
-
Received: ,
This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
This article was originally published by Wolters Kluwer - Medknow and was migrated to Scientific Scholar after the change of Publisher.
A 19 yr old male† patient presented to the Surgical Oncology outpatient department, All India Institute of Medical Sciences (AIIMS), New Delhi, India, in December 2018, with the chief complaints of painless progressive swelling of right-sided face for seven years. On clinical examination (Fig. 1), there was a solitary large soft cystic swelling measuring 16 ×16 cm in the right parotid region. Computed tomographic scan revealed subcutaneous oedema and fat reticulations in the right parotid region (Fig. 2). Core biopsy histopathology was suggestive of Kimura's disease (KD)/angiolymphoid hyperplasia (Fig. 3). The patient was treated with neoadjuvant radiotherapy (50.4 Gy, 28 fractions, six weeks) followed by surgical excision of the mass lesion and superficial parotidectomy with pectoralis major myocutaneous flap reconstruction. Final specimen histopathology rendered lymphoid hyperplasia. After nine months of follow up, the patient was disease-free.

- Pre-treatment image showing right-sided face and parotid region painless and progressively increasing swelling (arrow).
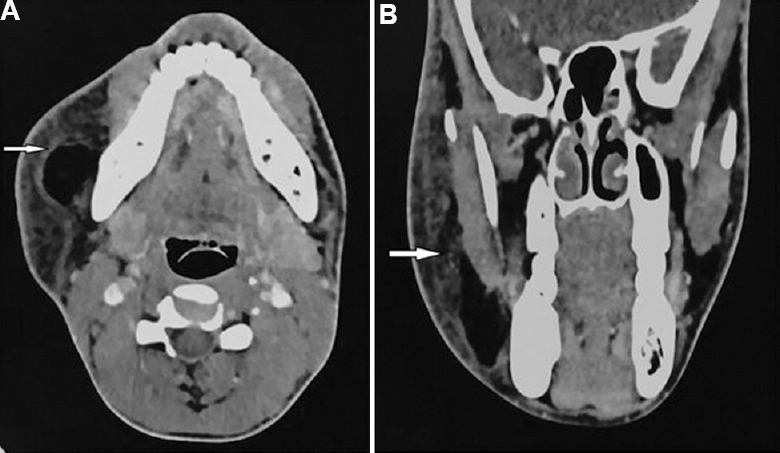
- Axial (A) and coronal (B) contrast-enhanced computed tomographic scan images showing subcutaneous oedema and fat reticulations (white arrows) in the right parotid region with an irregular outline of the right parotid gland.
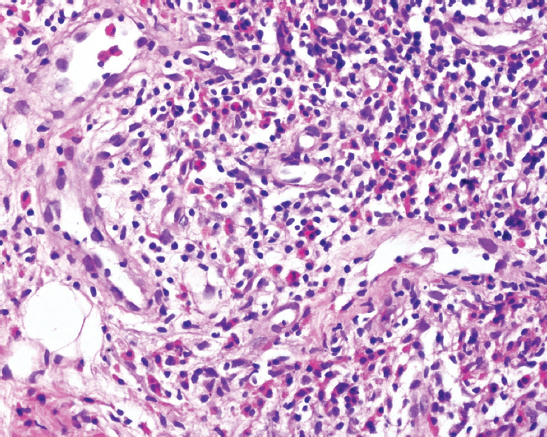
- Core biopsy showing fibroadipose tissue with lobules of inflammatory cells, i.e. lymphocytes, eosinophils and interspersed small vascular channels lined by plump endothelial cells, suggestive of angiolymphoid hyperplasia with eosinophilia (H and E, ×40).
Acknowledgment:
Authors thank Dr Aanchal Kakkar, department of Pathology, AIIMS, New Delhi, for providing pathological microphotograph and its details, Dr Ritesh Kumar, department of Radiotherapy, AIIMS, New Delhi, for providing radiation services to the patient and referral of the patient to surgical oncology services.
Conflicts of Interest: None.





