Translate this page into:
Meandering through arteriovenous malformation maze: A multidisciplinary approach
*For correspondence: abhiruge@yahoo.com
-
Received: ,
This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
This article was originally published by Wolters Kluwer - Medknow and was migrated to Scientific Scholar after the change of Publisher.
A 28 yr old female† presented to the Vascular and Interventional Radiology division at St John's Medical College and Hospital, Bengaluru, India, in October 2019, with painful progressively enlarging swellings over the right forearm for the past 15 years, which eventually led to deformity of the hand, ulceration and bleeding. On examination, there was clawing of the medial two fingers, ulceration and gangrenous changes of the fifth digit and audible bruit over the swellings (Fig. 1). Ultrasound Doppler study, showed a high-flow arteriovenous malformation (AVM), and digital subtraction angiography confirmed that feeders were from both ulnar and radial arteries (Figs 2, 3A and B and Video A).
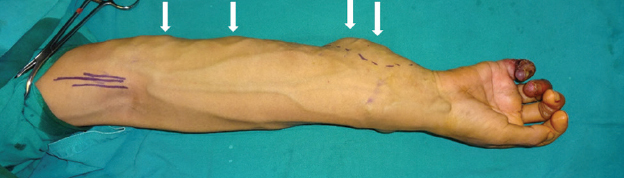
- Multiple painful swellings of the right forearm, ulnar clawing, ulceration and gangrene of the little finger. Multiple dilated and tortuous veins, pulsatile lesions and warm mass (white arrows) with a thrill on examination were also seen.
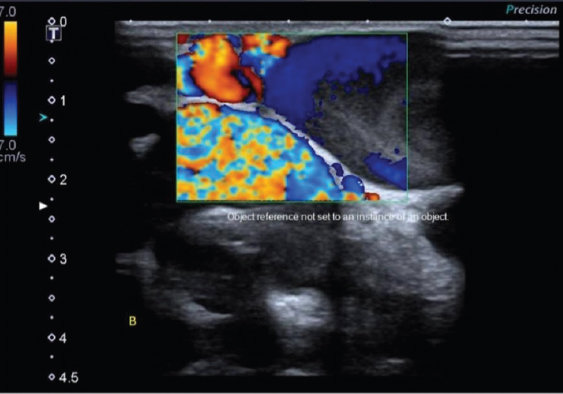
- Ultrasound image showing multiple tortuous dilated vascular channels with aliasing effect – high-flow vascular malformation.
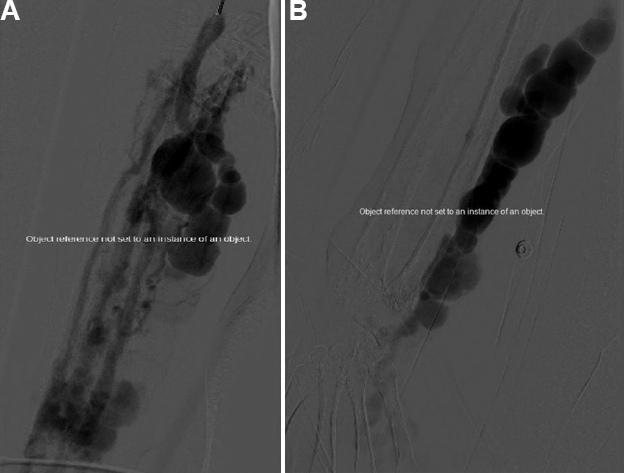
- Digital subtraction angiogram (DSA). (A) Pre-embolization selective digital subtraction angiography of the right brachial artery showing a high-flow arteriovenous malformation (AVM) with feeders arising both from radial and ulnar arteries was noted, with early opacification of multiple dilated tortuous AVM. (B) Pre-embolization selective DSA of the right ulnar artery showing feeders arising from ulnar artery, opacification of the nidus of abnormal vessels and with extension into the hand.
The adjunctive endovascular procedure was performed under local anaesthesia after cannulating the brachial artery via femoral access. The feeders from ulnar artery were embolized with a lipiodol-glue (2-N-butyl cyanoacrylate) combination, along with percutaneous sclerotherapy of the remnant veins (Fig. 4A and Video B).
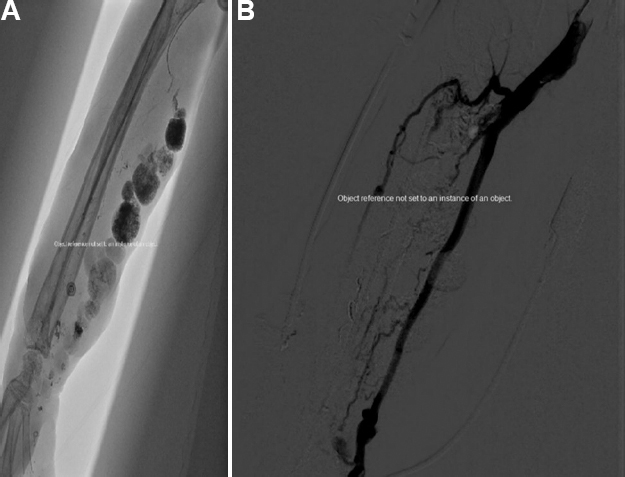
- (A) Image showing endovascular embolization of the nidus performed using lipiodol-glue combination. (B) Post-embolization selective digital subtraction angiogram of the right brachial artery showing exclusion of the nidus and glue-cast filling all the feeding branches from ulnar artery and the nidus; normal opacification of the radial artery is seen with residual AVMs which was not embolized to preserve the circulation to the hand.
Post-embolization selective angiogram of the right brachial artery showed obliteration of the nidus and glue-cast filling all the feeding branches from the ulnar artery and nidus. Normal opacification of the radial artery was seen with residual AVM (Fig. 4B and Video C), which was not embolized to preserve circulation to the hand. Subsequently, debulking surgery and amputation of the little finger due to gangrene were performed. Cosmetic results of the forearm post-surgery were appreciable along with symptomatic relief (Fig. 5).

- Post-debulking and amputation of little finger image of the right forearm showing significant reduction in the size of the AVMs.
 Video available at ijmr.org.in.
Video available at ijmr.org.in.
Acknowledgment:
Authors acknowledge Dr Naren, Department of Plastic Surgery, St Johns' Medical College & Hospital, Bengaluru.
Conflicts of Interest: None.





