Translate this page into:
Macrophage activation syndrome in a case of lupus: Identifying the trigger
*For correspondence: abledoc@gmail.com
-
Received: ,
This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
This article was originally published by Wolters Kluwer - Medknow and was migrated to Scientific Scholar after the change of Publisher.
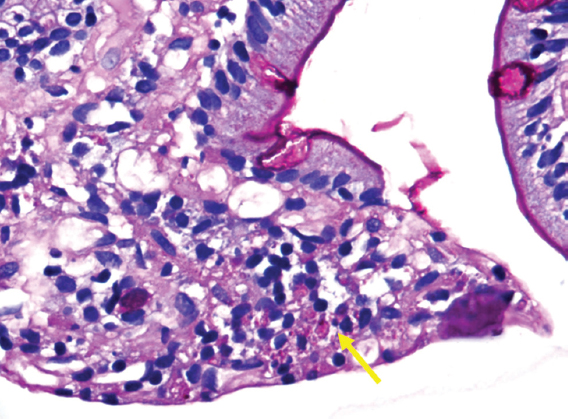
A 41 yr old male†, a case of lupus and secondary antiphospholipid antibody syndrome, presented to the department of Clinical Immunology at Sanjay Gandhi Postgraduate Institute of Medical Sciences, Lucknow, India, in April 2019, with fever, diarrhoea, melena, and hypotension. Investigations revealed pancytopenia, transaminitis, and deranged coagulation parameters with blood bacterial and fungal cultures being sterile. Ferritin was elevated, fibrinogen and erythrocyte sedimentation rate were low. Oesophagoduodenoscopy showed multiple duodenal ulcers and bone marrow (BM) examination showed occasional hemophagocytosis. He was treated for macrophage activation syndrome (MAS) and was discharged once blood counts improved. However, he returned in a week with fever and pancytopenia. Chest radiograph revealed bilateral heterogeneous infiltrates (Fig. 1A) and computed tomography chest confirmed the same (Fig. 1B). Repeat BM examination (Figs 2A, 2B and 3) revealed ill-defined granulomas formed by tiny foci of necrosis with karyorrhectic debris and epithelioid histiocytes and lymphocytes and several histiocytes showing Periodic acid–Schiff (PAS) positive intracellular yeasts. Giemsa stained peripheral blood smear also revealed small budding yeast cells (Fig. 4). Review of older duodenal biopsy showed histiocytic infiltration of the lamina propria with PAS-positive intracytoplasmic yeast forms (Fig. 5). The patient was treated for disseminated histoplasmosis and MAS with corticosteroids, liposomal amphotericin-B followed by itraconazole maintenance. He responded well with sterile cultures at five months follow-up.
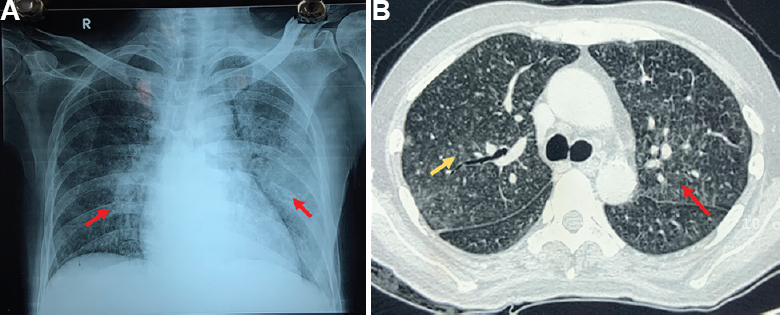
- (A) Chest Radiograph showing bilateral heterogeneous infiltrates (red arrows) affecting the left more than right lung and (B) Computed Tomography of the chest showing bilateral ground glass opacities (red arrow) and centrilobular nodules (yellow arrow) predominantly affecting the middle and lower lobes.
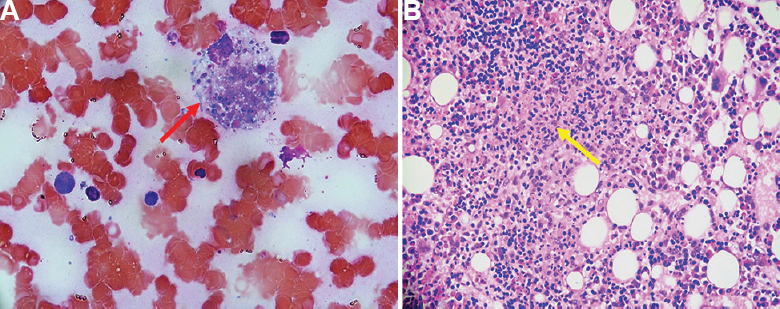
- (A) Bone marrow aspirate (PAS, ×40) showing evidence of hemophagocytosis with histiocytes (red arrow) showing intracellular small yeast forms (crescent-shaped nuclei with a pericellular halo) suggestive of histoplasmosis. (B) Bone marrow biopsy (H and E, ×10) showing ill-defined granulomas (yellow arrow) formed by tiny foci of necrosis with karyorrhectic debris and epithelioid histiocytes and lymphocytes.
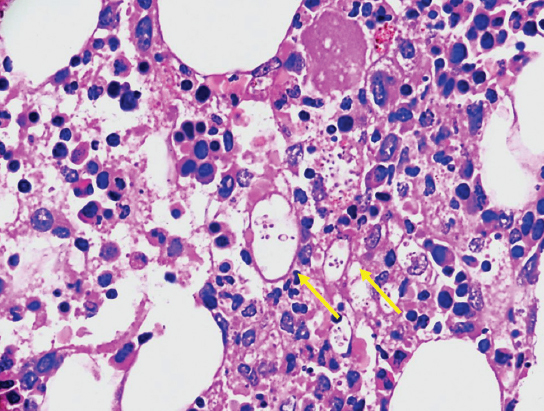
- Bone marrow biopsy (PAS, ×20) with several histiocytes showing PAS positive intracellular small yeast forms having round or crescent-shaped nuclei and pericellular halo (yellow arrows) suggestive of histoplasmosis.
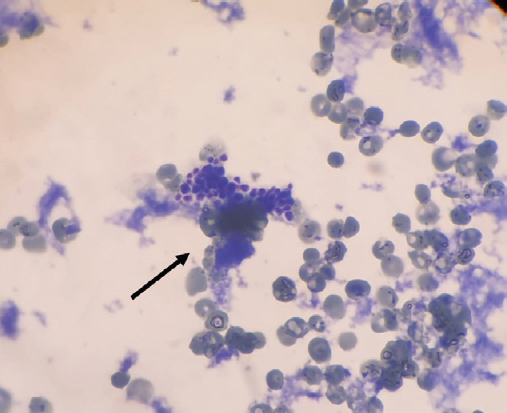
- Giemsa (×20) stained peripheral blood smear showing small budding yeast cells.
- Biopsy of duodenal ulcer (PAS, ×40) showing histiocytic infiltration of the lamina propria with PAS positive intracytoplasmic yeast forms.
Acknowledgments:
The authors acknowledge Drs Manjula Murari, Department of Pathology and Rungmei S.K. Marak, Department of Microbiology, SGPGIMS, Lucknow, for the photographs of pathology and microbiology specimens.
Conflicts of Interest: None.





