Translate this page into:
COVID-19 in India: Moving from containment to mitigation
*For correspondence: georgemvarghese@hotmail.com
This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
This article was originally published by Wolters Kluwer - Medknow and was migrated to Scientific Scholar after the change of Publisher.
In late December 2019, a cluster of cases with pneumonia of unidentified aetiology was reported in Wuhan city, Hubei province of People's Republic of China. This was soon identified to be caused by a novel strain of coronavirus which was named as severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) and the disease caused by it as the coronavirus disease (COVID-19)1. Since then, an epidemic of acute respiratory tract infection has been set in swing with the rapid transmission of infection primarily through droplets, respiratory secretions and direct contact2. By the end of February 2020, the infection had spread over 54 countries, infected more than 85,403 individuals across the world and resulted in an approximate 2,924 deaths3. The exponential rise in the number of cases being witnessed daily has compelled the World Health Organization (WHO) to title this outbreak a pandemic4.
In India, the first COVID-19 case was reported in Trissur, Kerala, on January 30, 20205. Current evidence suggests that the incubation period may last for 1-14 days, with a mean duration of 5-7 days2. The peak viraemia occurs at the end of the incubation period and before the onset of symptoms, suggesting that transmission begins 1-2 days before the onset of symptoms6. The rapid spread of infection is augmented by the potential for transmission by asymptomatic or minimally symptomatic patients7. Until now, our national strategy in tackling the COVID-19 has been predominantly one of containment, an approach typically utilized when a pathogen has slow transmission capacity or is brought in from external sources. This allows for the implementation of measures to limit its spread such as quarantine of individuals coming from a high transmission area, isolation of infected individuals, contact tracing as well as reducing the movement of people in areas that have a high case load. The containment strategies adopted by Kerala have helped in slowing the spread of infection into the community by the end of March8. However, once the infection starts to spread in the community with evidence of sustained local transmission, it becomes impossible to isolate all the infected individuals. In such situations, mitigation measures are needed with the aim to slow down the spread of infection. These procedures include closure of schools and a ban on public mass gatherings9. With the escalating number of COVID-19 cases being detected in our country over the last few weeks, it is time for India to shift its efforts to slow the spread of the SARS-CoV-2 virus from containment to community mitigation.
The community mitigation strategies are called 'flattening the curve' in epidemiological terms. The curve refers to the projected number of people who will contract COVID-19 over a given time frame. The shape of the curve varies according to the rapidity with which the infection spreads in the community. Infection curves with a steep rise also have a steep fall. This results in an overloading of the local healthcare systems beyond their capacity, leading to higher case fatality rates (Figure). The highest priority at this stage is to keep the mortality as low as possible. If individuals and communities take appropriate steps to slow the spread of the virus, the cases would be stretched out across a longer period of time, thereby flattening the curve and avoiding overburden of the existing healthcare systems. It also buys time to potentially develop newer drugs and vaccines targeted at the virus.
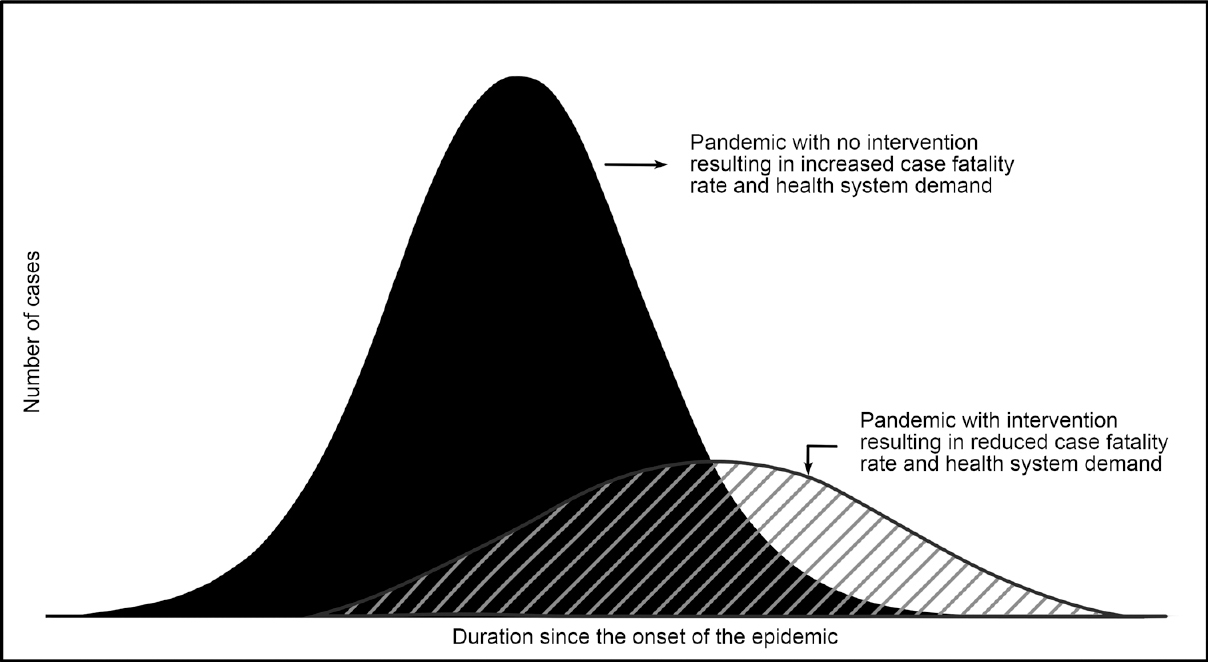
- Flattening the epidemic curve.
As the disease spreads in the community beyond the primary contacts, strategies to prevent further spread within communities is the need of the hour. We discuss below the possible interventions to help attain this.
Social distancing
Timely implementation of aggressive strategies that create social distance and reduce close contact of people has proven effective in delaying the rates of transmission and reducing severe illness and death in times of pandemic. The influenza outbreak of 1918 has proved that non-pharmaceutical measures such as social distancing are as important as drugs and vaccines in controlling a pandemic10. The lockdown in Wuhan to contain the COVID-19 outbreak in China showed a positive impact with significantly decreased growth rates and increased doubling time of cases11. Social distancing measures include isolation of infected people, quarantine of their contacts, options for people to work from home, the closure of schools and the cancellation of large gatherings. Such measures allow our healthcare system to handle the additional burden in a phased manner. The WHO recommends a minimum distance of at least 1 m (3 feet) to be maintained between individuals to prevent the spread of the infection through respiratory droplets12.
Personal protection measures
Individual protection measures, an integral part of infection control, reflect a level of personal commitment and action above and beyond governmental policies towards containment and mitigation of the disease. Evidence from earlier outbreaks advocate that face masks and hand hygiene reduce respiratory illnesses in shared living settings and in turn allay the impact of pandemics13. Frequent hand washing with soap and water may significantly reduce the chance of acquiring and transmitting the infection. Individuals are encouraged to practice respiratory hygiene. In case a person develops respiratory symptoms, using a medical mask is recommended. However, wearing rubber gloves out in public is discouraged and does not replace the need for appropriate hand hygiene. Disinfection and cleansing of frequently touched surfaces should also be carried out daily121415.
Home isolation when sick
Patients with suspected COVID-19, following triage at the point of first healthcare contact, can be managed at home if presenting with a mild illness, and there is no concern of rapid deterioration. Patients can be managed symptomatically with oral paracetamol. Such patients need to be placed in a well-ventilated single room, with their movements limited within the house and their shared space minimized. A single caregiver should optimally be chosen from among the household members, and visitors should not be permitted until the patient has a complete recovery. Respiratory masks are to be worn by both the patient and the caregiver, and dedicated linen and eating utensils should be assigned separately for the patient. All individuals in close contact with the patient with suspected or confirmed COVID-19 should be considered for quarantine and their health should be monitored for 14 days from the last day of interaction16.
Care of the vulnerable population
A critical facet of COVID-19 has been the disproportionately higher mortality seen among individuals more than 60 yr than the young adults or paediatric population17. Those above 80 yr were noted to have the highest case fatality rate at 14.8 per cent17. This was brought out in one of the largest data analyses conducted in China involving 72,314 patient records which comprised 44,672 (61.8%) confirmed cases, 16,186 (22.4%) suspected cases, 10,567 (14.6%) clinically diagnosed cases and 889 asymptomatic cases (1.2%). While patients with no prior co-morbid conditions had a case fatality rate of 0.9 per cent, the case fatality rate was higher among those with cardiovascular disease (10.5%), diabetes (7.3%), chronic respiratory disease (6.3%), hypertension (6.0%) and cancer (5.6%)17. These findings make it imperative to protect individuals belonging to these highly susceptible groups more strongly. As children may often be asymptomatic transmitters of the disease, their interaction with elderly should be limited18. Help in grocery shopping and delivery of food, medicines and essential services and supplies will go a long way in minimizing unnecessary exposure of our vulnerable population. Such rationally layered social-distancing interventions may be a more acceptable long-term solution to the current pandemic19.
Widening the testing and treatment capacity
Initially, testing facilities for COVID-19 by reverse transcription-polymerase chain reaction (RT-PCR) laid with government facilities alone, with the Indian Council of Medical Research (ICMR) recommending the testing of only those symptomatic patients with a history of international travel to affected countries or a history of close contact with a laboratory-confirmed positive case20. India has now scaled up the diagnostic and laboratory testing for SARS-CoV-2 virus considering the dire urgency for enhanced case detection to curb the dissemination of the disease. There is a need to secure adequate clinical infrastructure in the country with ample supply of personal protective equipment for the healthcare professionals. The ICMR-National Institute of Virology, Pune, has succeeded in retrieving the SARS-CoV-2 strain from infected patients, confirming a homology of 99.98 per cent with the strain from Wuhan21. This could imply that similar patterns of disease transmission can be expected if robust strategies to tackle the infection are not in place. It also gives hope to the possible development of newer diagnostics, therapeutics and vaccines to combat COVID-19. A comprehensive approach is needed to break the chains of transmission, and more aggressive testing, early diagnosis and isolation along with adequate treatment seem to be the way forward in tackling this infection in the future.
As India prepares for a worst case scenario, it is of utmost importance for all its citizens to follow strict hygiene practices to ensure self-protection and prevent the further spread of the infection within the community. The success of mitigation strategies will depend on public adherence to these. Clear, coordinated management guidelines need to be communicated consistently to healthcare professionals as well as to the public to avoid unnecessary fear and anxiety. With these measures, we can hope to tide over the pandemic as early as possible.
Conflicts of Interest: None.
References
- 2020. Novel coronavirus (2019-nCoV) situation report - 1. WHO; Available from: https://wwwwhoint/docs/default-source/coronaviruse/situation-reports/20200121-sitrep-1-2019-ncov
- The origin, transmission and clinical therapies on coronavirus disease 2019 (COVID-19) outbreak - an update on the status. Mil Med Res. 2020;7:11.
- [Google Scholar]
- 2020. Coronavirus disease 2019 (COVID-19) situation report - 40. WHO; Available from: https://wwwwhoint/docs/default-source/coronaviruse/situation-reports/20200229-sitrep-40-covid-19
- 2020. WHO Director-General's opening remarks at the media briefing on COVID-19. WHO; Available from: https://wwwwhoint/dg/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19---11-march-2020
- 2020. India confirms its first coronavirus case. CNBC; Available from: https://wwwcnbccom/2020/01/30/india-confirms- first-case-of-the-coronavirushtml
- How will country-based mitigation measures influence the course of the COVID-19 epidemic? Lancet. 2020;395:931-4.
- [Google Scholar]
- SARS-CoV-2 viral load in upper respiratory specimens of infected patients. N Engl J Med. 2020;382:1177-9.
- [Google Scholar]
- GoK Dashboard. Kerala: COVID 19 battle; Available from: https://dashboardkeralagovin/indexphp
- Social measures may control pandemic flu better than drugs and vaccines. BMJ. 2007;334:1341.
- [Google Scholar]
- The positive impact of lockdown in Wuhan on containing the COVID-19 outbreak in China. J Travel Med 2020 pii: Taaa037
- [Google Scholar]
- 2020. Coronavirus disease (COVID-19) advice for the public. WHO; Available from: https://wwwwhoint/emergencies/diseases/novel-coronavirus -2019/advice-for-public
- Mask use, hand hygiene, and seasonal influenza-like illness among young adults: A randomized intervention trial. J Infect Dis. 2010;201:491-8.
- [Google Scholar]
- 2020. Rational use of personal protective equipment for coronavirus disease 2019 (COVID-19): Interim guidance, 27 February 2020. WHO; Available from: https://appswhoint/iris/bitstream/handle/10665/331215/WHO-2019-nCov-IPCPPE_use-2020 1-engpdf
- Coronavirus disease 2019 (COVID-19): How to protect yourself. Available from: https://wwwcdcgov/coronavirus/2019-ncov/prepare/preventionhtml
- 2020. Home care for patients with COVID-19 presenting with mild symptoms and management of their contacts: Interim guidance, 17 March 2020. WHO; Available from: https://wwwwhoint/publications-detail/home-care-for-patients-with-suspected-novel-coronavirus-(ncov)-infection-presenting-with-mild-symptoms-and-management-of-contacts
- The epidemiological characteristics of an outbreak of 2019 novel coronavirus diseases (COVID-19) in China. Zhonghua Liu Xing Bing Xue Za Zhi. 2020;41:145-51.
- [Google Scholar]
- The different clinical characteristics of corona virus disease cases between children and their families in China - the character of children with COVID-19. Emerg Microbes Infect. 2020;9:707-13.
- [Google Scholar]
- 2020. Note on COVID-19 laboratory preparedness in India. New Delhi: ICMR; Available from: https://icmrnicin/sites/default/files/press_realease_files/ICMR_PressRelease_COVID_19
- Full-genome sequences of the first two SARS-CoV-2 viruses from India. Indian J Med Res 2020:151. doi: 104103/ijmrIJMR_663_20
- [Google Scholar]





