Translate this page into:
Charting a roadmap for heart failure research in India: Insights from a qualitative survey
For correspondence: Dr Sivadasanpillai Harikrishnan, Department of Cardiology, Sree Chitra Tirunal Institute for Medical Sciences & Technology, Thiruvananthapuram 695 011, Kerala, India e-mail: drharikrishnan@outlook.com
-
Received: ,
This article was originally published by Wolters Kluwer - Medknow and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Background & objectives:
Heart failure (HF) is emerging as a major health problem in India. The profile of HF in India is divergent from elsewhere in the world. While cardiologists must equip themselves with the requisite clinical management tools, scientists and health policymakers would need epidemiological data on HF and information on the resources required to meet the challenges ahead. The aim of this study was to identify the lacunae and to suggest recommendations to improve HF research.
Methods:
We surveyed a multidisciplinary group of HF experts using a two stage process. An email-based survey was conducted using a structured questionnaire, followed by an online discussion. The experts prioritized the major challenges in convergence research in India and inter-rater agreement values were calculated. In addition, they enlisted potential research gaps and barriers in the domains of epidemiology, diagnostics, management and technology and suggested recommendations to overcome those barriers.
Results:
The experts identified a paucity of data on HF burden, lack of state-of-the-art diagnostic facilities and trained personnel, overt dependence on imported devices/equipment/reagents, lack of interaction/awareness/information among stakeholders and lack of biobanks, as major barriers in HF research. Three fourths of the experts agreed that lack of interaction among stakeholders was the major challenge with the highest inter-rater agreement in both stages (19 out of 25 and 11 out of 17, respectively). The experts recommended the creation of multidisciplinary taskforces dedicated to population sciences, data sciences, technology development and patient management with short-, intermediate- and long-term strategies.
Interpretation & conclusions:
The study generated a wish list for advances in HF research and management, and proposed recommendations for facilitating convergence research as a way forward to reduce the burden of HF in India.
Keywords
Diagnostic
genomics
health policy
heart failure
India
multidisciplinary
Heart failure (HF) is emerging as a global pandemic1. With advancing epidemiological transition, India is expected to experience ‘double burden’ posed by the persistence of old age diseases such as rheumatic heart disease, and the emergence of new-age diseases such as coronary artery disease increases the propensity for HF2. Although clinical and epidemiological data on HF in India are limited, the recently established regional and national registries such as the Trivandrum Heart Failure Registry and the National Heart Failure Registry have aided in compiling clinical and epidemiological information3,4. Basic research related to HF, however, is still at its infancy and there is a perceived lack of coordination and collaboration between clinicians and basic researchers5.
Given the need for successful integration of clinical and basic research, the Indian Council of Medical Research (ICMR) – National Centre for Advanced Research and Excellence in HF (CARE-HF) at Sree Chitra Tirunal Institute for Medical Sciences and Technology (SCTIMST) at Trivandrum, with the International Academy of Cardiovascular Sciences and the Heart Failure Association of India (HFAI) initiated a dialogue between clinical investigators and basic scientists to integrate ideas on how to channelize available resources for convergence research. The aim of this study was to identify the lacunae in broad areas such as epidemiology, diagnostics, technology and management and to suggest recommendations to improve HF research in India.
Material & Methods
Identification of experts: Experts involved in the field of HF or cardiology were identified based on their publications in PubMed Indexed journals. The NCBI Entrez Programming Utilities (E-Utilities) were used to retrieve their email IDs6. Initially, the Web of Science database was searched to identify articles using ‘heart failure’ and ‘India’ as keywords. The DOIs of the 3743 retrieved articles were imported into the ESearch programme of the E-utilities to find their corresponding PMIDs. The 3510 articles that were returned with PMIDs were imported into the EFetch programme to fetch author affiliations and email IDs. After the removal of duplicates and exclusion based on the screening of titles and abstracts, we could identify 125 experts in HF research in India (Figure).
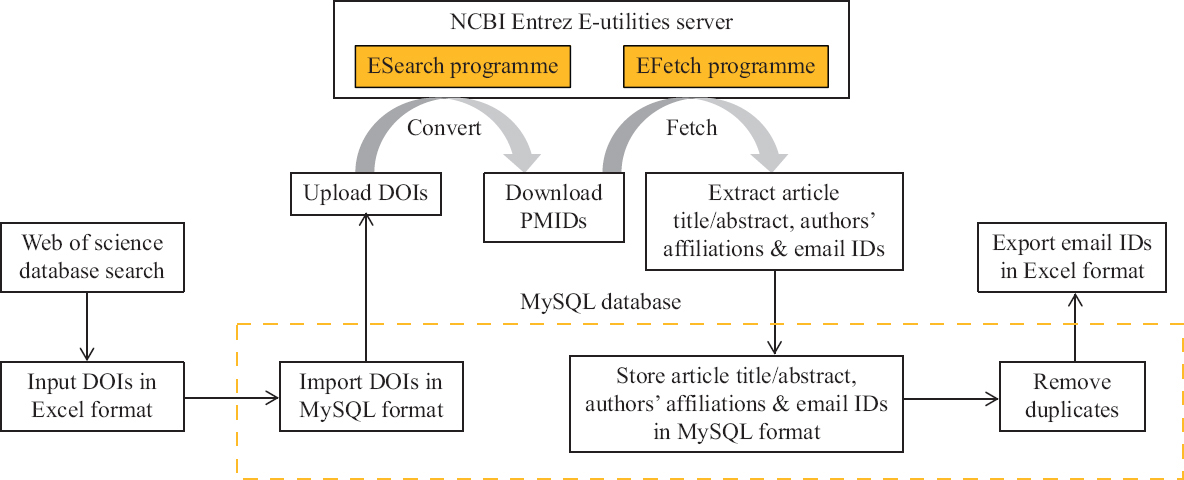
- Process flow adopted for identifying email IDs of experts. NCBI, National Center for Biotechnology Information; DOIs, dgital object identifier
Development of the questionnaire and two stage survey: A panel of three cardiologists, three scientists and two public health experts identified the research questions to be included in the questionnaire, following an in-depth literature survey7-9. From the literature, the following areas of epidemiology, diagnostics, technology and management were identified as domains that require research focus for HF. The questionnaire was divided into two sections, as shown in Table I, which was directed to either clinicians or scientists. The questionnaire sought the expert’s views on the burden of HF in India, the diagnostic and therapeutic challenges in the management of HF, the relationship between multi morbidity and clinical outcome, the impact of HF on the patient, health system and society and the perspectives from clinicians and scientists on the challenges of convergence research.
| Questions for clinicians |
| • What is the HF burden in India? Is multimorbidity as a clinical syndrome in Indian HF patients associated with poor health outcomes? Do we have enough evidence to indicate this? Which are the major clusters of conditions in HF patients in India associated with an extended length of hospital stay, days in and out of the hospital, elevated cost and increased risk of mortality? |
| • What are the diagnostic and therapeutic challenges which you face while managing these clusters of patients? |
| • Identify the problems which you would like to be addressed or solutions to be discovered in collaborative studies with scientists? |
| • What do you think are the major challenges in convergence research in India and what are your recommendations to overcome them? |
| Questions for basic scientists |
| • What are the expertise and tools available in India for (a) identifying diagnostic and prognostic biomarkers (b) developing diagnostic and treatment devices (c) drugs and cardiac regenerative strategies for HF? |
| • What are the diagnostic challenges in using known markers for managing a co-morbidity in HF patients? Which new biomarkers can help in better management of HF patients with multimorbidity? |
| • Would you be interested in being part of a multicentric multidisciplinary research team? In what areas would you like to collaborate in HF research? |
| • Give a list of research projects in HF which if nurtured through collaboration between basic scientists and cardiologists and or cardiovascular surgeons can be used in clinical practice in the next three years (low hanging fruit) or five years (long term)? |
| • What do you think are the major challenges in convergence research in India and what are your recommendations to overcome them? |
HF, heart failure
For the first stage, an e-mail survey was conducted, wherein an invitation email explaining the aim of the study along with the semi-structured open ended questionnaire was sent to all selected experts. The selected experts included cardiologists, basic scientists, public health professionals and biomedical engineers, from national institutes and representatives from funding agencies. Few experts were also contacted telephonically. For the second stage, an online brainstorming session was conducted in conjunction with an online international conference, ‘Heart Failure Conflux’, jointly organized by the department of Cardiology, SCTIMST and HFAI in February 2021. The expert panel discussed the questionnaire in detail, and the responses received from the first stage of the email survey. Responses to questions that elicited descriptive responses were compiled and summarized broadly into challenges, barriers and research gaps, and recommendations in areas such as epidemiology, diagnostics, technology and management for HF.
Results & Discussion
A total of 42 experts were surveyed. In the first stage of the email survey, we received feedback from 25 experts (5 females) among the 125 individuals (102 males and 23 females) to whom the questionnaires were sent (20% response rate). In the second stage, 17 experts participated in the online brainstorming session. The major challenge identified in convergence research in India was the lack of awareness/information/interaction that was identified as the item with the highest agreement in both stages, 19 out of 25 and 11 out of 17 in stage 1 and 2, respectively. The lack of funding/research facility/trained personnel was the item with the second highest agreement identified in stage 1, whereas in stage 2, the lack of data/registries/specimens/biobanks was identified as the item with the second highest agreement. The lack of biomedical industry involvement was the item with the third highest agreement identified in stage 2, followed by administrative delays/regulatory approvals.
The barriers and research gaps in areas of epidemiology, diagnostics, technology and management for HF in India, and a listing of recommendations for overcoming these barriers, are listed in Tables II and III. The strategies to be taken up in the road map as the way forward in areas are (i) identification and prioritization of specific research questions for studies related to HF, (ii) defining an approach to achieve the objectives, (iii) delineating foreseeable stumbling blocks, and (iv) drafting an action plan for initiating interdisciplinary and collaborative research. The complex nature of HF which is an outcome of a number of clinical conditions, suggests that a diverse array of projects would be required to address the research gaps in epidemiology, diagnostics, technology and management. However, a few research activities that can be pursued as short-, intermediate- and long-term goals are illustrated below.
| Broad areas | Research gaps and barriers | Salient recommendations |
|---|---|---|
| Epidemiology | Lack of prevalence and incidence data on HF in India | Initiate hospital-based registries |
| Lack of data on heterogeneity amongst HF patients in terms of age at onset, risk factors, comorbidities and prognosis | Sub-phenotype HF to address patient heterogeneity | |
| Lack of data on multimorbidity associated with poor health outcomes in HF | Collect data on co-morbidities such as cardio-renal syndrome, chronic obstructive pulmonary disease and sleep apnoea | |
| Lack of data on COVID-19 and long-COVID related cardiac and vascular complications in HF | Collect data on COVID-19 infections for HF prognosis | |
| Lack of data on the association between air pollution and HF in the Indian context | Collect data on the effect of air pollution in HF | |
| Lack of data on the influence of the Indian diet in HF | Investigate the role of the gut microbiome in HF pathogenesis | |
| Lack of data on population-specific genetic/pharmacogenetic and conventional risk factors for HF and its subtypes | Apply genetic screening methods to discover novel population-specific genetic markers of cardiomyopathies and channelopathies. Implement pre-emptive pharmacogenetic testing | |
| Diagnostics | Biomarkers such as NPs are costly and not available in all peripheral centres | Develop a multi-biomarker panel for capturing the complexity of HF |
| Fluctuations and variations in biomarker levels in different patient groups pose a challenge to the treating physician | Identify markers for early detection of HF as well as ‘stage-specific’ using an integrated omics approach. Identify markers of decompensation and readmission in patients with HF, cardiac structural remodelling and the differences in patients with HFrEF and HFpEF with emphasis on non-invasive circulating biomarkers | |
| Limited infrastructure, expertise and training facilities for conducting omics studies using next-generation sequencing, LC–MS, MALDI-TOF MS and microarray platforms, for identifying diagnostic and prognostic markers | Create advanced diagnostics facilities attached to hospitals with adequately trained supporting personnel. Initiate multi-centric hospital-based trials to gather data for validating novel markers | |
| Lack of biobanks with high-quality biospecimens and related clinical data for biomarker discovery | Establish biobanks (serum, plasma, saliva, DNA and tissue samples) and clinical autopsy centres with carefully-phenotyped data for HF biomarker discovery |
NPs, natriuretic peptides; LC-MS, liquid chromatography-mass spectrometry; MALDI-TOF MS, matrix-assisted laser desorption ionization time-of-flight mass spectrometry; HF, heart failure; HFrEF, HF with reduced ejection fraction; HFpEF, HF with a preserved ejection fraction
| Broad areas | Research gaps and barriers | Salient recommendations |
|---|---|---|
| Technology | Lack of indigenous technology for production of diagnostic and surgical tools | Initiate industrial incubation centres to develop or scale-up production of indigenous low-cost POC devices, testing platforms and diagnostic reagent/consumables for HF diagnostics |
| Overt dependence on imported reagents and consumables with vendor or technology ‘lock-in’, has led to a steady hike in prices | Develop self-monitoring gadgets and mobile applications for patients to ensure drug compliance, monitoring of body weight and periodic follow up, with online support from cardiologists or specialist nurses, and ASHA workers. Develop sensors that can be integrated to a mobile app to diagnose volume overload state-‘wet and cold acute decompensated HF’ | |
| Increasing annual maintenance costs of imported diagnostic equipment and non-availability of local service engineers | Fabricate low-cost indigenous cardiac resynchronization therapy (CRT), pacemaker and his bundle pacing for use in patients with severe left ventricular dysfunction and left bundle branch block | |
| Paucity of large-scale funding as available in developed countries, with a lack of public-private sector interaction | Identify strategies to encourage funding from non-governmental agencies as seen in the Horizon Europe funding programmes. Ensure that high-risk goals (blue sky research) with no immediate returns are considered for research funding | |
| Management | Lack of leadership and governance model to facilitate research alongside patient care | Create a transdisciplinary platform for networking of institutions dedicated to HF research, comprising cardiologists, cardiac surgeons, public health experts, geneticists, molecular biologists, pathologists and bio-medical technologists |
| Lack of forum/platforms for fruitful interactions between clinicians and scientists | Develop a national database with a national EMR system for long-term follow-up of patients with HF, accessible to clinicians and scientists | |
| Lack of EMR, and poor inter-operability of EMR data amongst hospitals due to the absence of unique patient identification number | Design a national HF research portal where expertise and experience can be exchanged | |
| Lack of patient hand over and tracking, where the concept of clinical handover or referral linkages is either rudimentary and non-existent | Build community-level surveillance systems to collect data for application of artificial intelligence for big data analysis | |
| Inadequacies in public awareness that lead to delayed presentation to the healthcare facility, and delay in early revascularization in patients with coronary artery disease | Reorganize the health system by improving awareness and quality of clinical care and decision support systems to aid HF nurses and ASHA workers | |
| Lack of regular periodic follow up resulting in difficulty to achieve up-titration of disease-modifying agents to target levels | Explore traditional medicines and biologicals in HF treatment | |
| Patients in HF require polypharmacy, some of the drugs may not produce desired effects in all those administered | Promote prescription of polypills in treatment of comorbidity | |
| Expertise and facilities for advanced HF management and cardiac rehabilitation are only available in the cities. Lack of dedicated HF clinics and beds that are otherwise available only in a few tertiary care centres and private hospitals | Identification of markers of relapse of HFimpEF, and investigate potential of myocardial regeneration therapy | |
| Delays in obtaining regulatory approvals; difficulties in obtaining informed consent from study participants | Create a benefit-sharing model for of patents/publications. Draft standard operating protocols for preparing MoUs and MTA | |
| Predicaments in credit sharing amongst clinicians and scientists while filing of patents and publications | Adopt standardized contribution disclosure form such as CRediT, to describe each author’s specific scholarly input to a publication. Consult a legal cell while filing patents to safeguard intellectual property rights and to improve patent contribution disclosure |
CRT, cardiac resynchronization therapy; EMR, electronic medical records; ASHA, accredited social health activist; HF, heart failure; HFimpEF, HF in patients with improved ejection fraction; POC, point-of-care; MoUs, memorandum of understanding; MTA, material transfer agreement; CRediT, contributor roles taxonomy
Epidemiology: Initiate registries, surveys, trials and taskforces for HF and subtypes.
Limited data on HF are available from India. The data available from hospital-based registries suggest that the burden is likely to be high, which can be expected to increase the HF burden in the coming years due to the ageing of the population and comorbidities. Indian patients are younger by 10-15 yr10 and they have a higher prevalence of comorbidities such as diabetes mellitus and smoking3. The most common causes of HF in India were identified as coronary artery disease, cardiomyopathies and valvular heart disease3,11,12. However, population-representative data on HF incidence, prevalence and mortality are not available from India. Further, conditions related to the Indian context that are associated with HF such as peripartum cardiomyopathy12, HF associated with infectious diseases such as dengue fever13 and leptospirosis and the restrictive cardiomyopathy-endomyocardial fibrosis have not been studied in detail14. Multimorbidity as a clinical syndrome in Indian HF patients was associated with poor health outcomes. The discovery of primary prevention strategies aimed at reduction of risk for HF can be a possible as a strategy to bring down the incidence of HF. Moreover, the low prevalence of HF with preserved ejection fraction amongst Indian patients has not been well characterized in the Indian setting. The burden and management of HF in paediatric cases were noted to be distinct from that of adults. A common cause for HF in children was attributed to a structural defect such as a congenital heart anomaly, which could be eminently treated and cured unlike in adults where treatment of HF is palliative in a sizeable population, the significance of this difference from adult patients does not seem to be seriously recognized. Computation-based prediction tools for HF can be developed using long-term data from registries15. This model can be structured on the available demographic data, and the information on classical HF biomarkers that are routinely measured in patients, as well as the use of medications for comorbidities. Of note, computational cardiology is a new multidisciplinary frontier that integrates patient-specific heart or ventricular imaging and health informatics data from large patient populations16. These computational cardiology models based on physiology and physics rather than on population statistics, enable computational simulations for instance, to predict the risk of sudden cardiac death or to predict treatment outcomes for individual patients.
A significant percentage of COVID-19 patients develop cardiovascular complications and HF which was not uncommon in those who developed severe disease. The COVID-19 pandemic led to two problems, first, it added to the disease burden itself and second, prevented patients with HF from getting regular follow ups and maintenance of guideline-directed therapy. Nevertheless, the COVID-19 pandemic gave a unique opportunity to the scientific community to respond proactively by designing and developing diagnostic tools indigenously.
Joint forums for scientific discussions and exchange between leading institutions in India may facilitate convergence in HF research. The majority of the scientists agreed (17 out of 19) to be a part of multicentric multi-disciplinary research. A multidisciplinary task force on HF comprising cardiologists, scientists, public health experts, technologists, industry representatives, information technology experts and health economists may be constituted under the combined administrative umbrella of the ICMR, DST (Department of Science & Technology), DBT (Department of Biotechnology) and CSIR (Council of Scientific & Industrial Research) to draft a mission document for translational HF research. A model incorporating patient advocacy groups may also be integrated into the task force since they are important stakeholders in treatment selection17. Since HF is a broad and multidimensional topic, the task force may have subgroups dedicated to (i) population sciences, which may consider the creation of regional and or national cohorts of HF patients, and a national HF registry with biorepositories and biobank facilities, (ii) data sciences focussed on compiling clinical, imaging, molecular and genetic data from diverse patient populations across the country using the National HF Registry of ICMR as a launchpad and using artificial intelligence to study the linkages between phenotypes and genotypes, or interactions between environment and phenotypes, (iii) technology development and identifying low-cost solutions in technology, and (iv) identifying ways of improving quality of clinical care and decision support systems to aid HF nurses and accredited social health activist (ASHA) workers.
Diagnostics: (i) Facilitate the discovery of genetic, protein and transcriptome-based biomarkers, (ii)Establish biobanks.
Three fourths of the experts agreed (19 out of 25) that there were either diagnostic or therapeutic challenges while managing HF patients. The genetic screening of patients with cardiac channelopathies or cardiomyopathies provides the opportunity for disease prevention through genetic counselling. The ICMR is currently supporting projects that aim to characterize genetic mutations among hypertrophic cardiomyopathy patients using next-generation sequencing, and for the development of point-of-care (POC) device for NT-pro BNP detection. The study of the ‘Expressed Genome’ in HF is also an exciting and significant long-term project to pursue. Expressed genome profiling of blood and myocardial tissue could aid the discovery of novel biological processes, leading to novel diagnostic tests18. Similarly, small RNAs such as miRNA, circular RNA and long non-coding RNAs would be promising transcriptome-based biomarkers for explaining the phenotypic variance of HF and complex comorbidities19. For instance, circular RNA Foxo3 was found to modulate stress response that induced cardiac senescence involved in HF20. Pharmacogenomics in HF is an area where research goals can be achieved in the short-term. Biobanks which hold collected patient samples and associated phenotypic data are an invaluable resource to enhance biomarker development. The ICMR-funded National Heart Failure Biobank, constituted as part of the CARE-HF at the SCTIMST, is collecting biospecimens and clinical data from HF patients (https://heartfailure.org.in/). Such initiatives can be extended to collecting representative samples from different regions across India.
Technology: Facilitate indigenous development and patenting of POC devices, implants and diagnostic assays.
Areas such as medical device development, artificial intelligence and deep learning, activities related to the development of POCs for the detection of biomarkers, microfluidics and lateral flow assays were still in infancy in our country. Prioritization both for research objectives as well as for technology development is required in tandem since this would be advantageous for the optimal utilization of resources in the public/private sector and for the funding agencies to rank new projects before sanction of funds. The indigenous development of POC devices and implants can be pursued as an intermediate-term strategy, whereas the development of the left ventricular assist devices (VADs) and pacemakers can be envisaged as long-term strategies.
Management: Development of standard operating protocols (SOPs) for the management of HF subtypes and comorbidities.
Among patients stabilized after the initial presentation with acute decompensated HF, only <5 per cent of the patients need focussed high-intensity therapy, while the majority can be managed with relatively simple measures. The identification of these two different groups of patients could be advantageous for streamlining management protocols. In the Indian setting, the management of HF treatment is undeniably resource intensive, where resources must be channelized cost-effectively. Clinicians need to weigh between spending on high-cost short-term circulatory support devices like VADs vs. providing free proven disease-modifying HF medications to a larger population. Studies on quality improvement programmes, the development of decision support systems and their impact, and the effectiveness of the use of semi-skilled workers in follow up care can be taken up as short-term programmes.
Brief roadmap for HF research in India: With the goal to improve the quantity and quality of HF research in India, this study has identified the research gaps and barriers in broad areas such as epidemiology, diagnostics, technology and management of HF. We have proposed recommendations in each of these areas that can be pursued as research actions in the next three years (short term) or five years (long term). Joint scientific forums involving basic scientists, technology developers, omics experts, cardiologists, primary care physicians, patients and policy makers can take responsibility to facilitate multi- and transdisciplinary research in HF. Funding earmarked specifically for HF can be provided for collaborative research, to be completed in short and long timeframes. The funding agencies can monitor and evaluate the research output in terms of patents or publications, and evidence of success measured in terms of number of technology transfers or number of policies implemented. In conclusion, this would support social and community led innovations to foster a sustainable development of local communities alongside powerful actors such as policy and industry.
Financial support and sponsorship
This study received funding support from the Centre for Advanced Research and Excellence (CARE) in Heart Failure (File No. 55/4/5/CARE-HF/2018-NCD-II), funded by the Indian Council of Medical Research (ICMR), New Delhi. The support for the online meeting was provided by the Heart Failure Association of India (HFAI).
Conflicts of interest
None.
Acknowledgment:
Authors acknowledge the following experts who participated in our study and provided their valuable opinions and suggestions.
The participants were (in alphabetic order of the place): Assam: Drs Sanjay Banerjee (NIPER); Bengaluru: S.R. Kalpana (SJICSR); Canada: Naranjan S. Dhalla (Manitoba University); Chandigarh: Ajay Bahl, Anupam Mittal (PGIMER); Chennai: Nitish Mahapatra (IITM); Guwahati: Vibin Ramakrishnan (IIT); Hyderabad: Renu John (IIT); Kochi: Indulekha Pillai, R. Krishna Kumar (AIMSRC); Kottayam: Johny Joseph (Caritas Hospital); Lucknow: Barthwal Manoj, Shashi Kumar Gupta (CDRI); Mumbai: Soumyo Mukherji (IIT Bombay); Mysuru: Veena Nanjappa (SJICSR, Mysore Branch), New Delhi: Dorairaj Prabhakaran (CCDC and PFHI), Meenakshi Sharma (ICMR), Sandeep Seth (AIIMS), Shantanu Sengupta, Vinod Scaria (CSIR-IGIB); Shimla: Prakash Negi (IGMC); Thiruvananthapuram: Abdul Jaleel, S. Ananthalakshmi, R. Radhakrishnan, Surya Ramachandran (RGCB), C.C. Kartha (KIMS), C.V. Muraleedharan, D.S. Nagesh, G. Srinivas, Kavita Raja, K. Shivakumar, P.R. Harikrishna Varma (SCTIMST); P.R. Sudhakaran (Kerala University); Sankar V. H. (SAT).
References
- The upcoming epidemic of heart failure in south Asia. Circ Heart Fail. 2020;13:e007218.
- [Google Scholar]
- Clinical presentation, management, in-hospital and 90-day outcomes of heart failure patients in Trivandrum, Kerala, India:the Trivandrum Heart Failure Registry. Eur J Heart Fail. 2015;17:794-800.
- [Google Scholar]
- National Heart Failure Registry, India: Design and methods. Indian Heart J. 2019;71:488-91.
- [Google Scholar]
- CSI position statement on management of heart failure in India. Indian Heart J. 2018;70:S1-72.
- [Google Scholar]
- National Center for Biotechnology Information. A general introduction to the E-utilities. Available from: https://www.ncbi.nlm.nih.gov/books/NBK25497/
- Omics phenotyping in heart failure:the next frontier. Eur Heart J. 2020;41:3477-84.
- [Google Scholar]
- Heart failure in the era of precision medicine: A scientific statement from the American Heart Association. Circ Genomic Precis Med. 2019;12:458-85.
- [Google Scholar]
- Biomarkers in heart failure:the past, current and future. Heart Fail Rev. 2019;24:867-903.
- [Google Scholar]
- Heart failure in Africa, Asia, the Middle East and South America: The INTER-CHF study. Int J Cardiol. 2016;204:133-41.
- [Google Scholar]
- In-hospital and three-year outcomes of heart failure patients in South India: The Trivandrum Heart Failure Registry. J Card Fail. 2018;24:842-8.
- [Google Scholar]
- Peripartum cardiomyopathy: An analysis of clinical profiles and outcomes from a tertiary care centre in southern India. Obstet Med. 2020;13:179-84.
- [Google Scholar]
- Spectrum of cardiac involvement in patients with dengue fever. Int J Cardiol. 2021;324:180-5.
- [Google Scholar]
- Geographical distribution of endomyocardial fibrosis in South Kerala. Int J Epidemiol. 1996;25:1202-7.
- [Google Scholar]
- Big Data Approaches in heart failure research. Curr Heart Fail Rep. 2020;17:213-24.
- [Google Scholar]
- A model for incorporating patient and stakeholder voices in a learning health care network: Washington State's Comparative Effectiveness Research Translation Network. J Clin Epidemiol. 2013;66:S122-9.
- [Google Scholar]
- The expressed genome in cardiovascular diseases and stroke: Refinement, diagnosis, and prediction: A scientific statement from the American Heart Association. Circ Cardiovasc Genet. 2017;10:e000037.
- [Google Scholar]
- Circular RNAs in hypertension:challenges and clinical promise. Hypertens Res. 2019;42:1653-63.
- [Google Scholar]
- Foxo3 circular RNA promotes cardiac senescence by modulating multiple factors associated with stress and senescence responses. Eur Heart J. 2016;38:1402-12.
- [Google Scholar]






