Translate this page into:
Determinants of post discharge mortality among hospitalized COVID-19 patients
For correspondence: Dr Aparna Mukherjee, Clinical Studies & Trials Unit, Indian Council of Medical Research, New Delhi 110 029, India e-mail: aparna.sinha.deb@gmail.com
-
Received: ,
This article was originally published by Wolters Kluwer - Medknow and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Background & objectives:
The post-acute effects of COVID-19 are continually being updated. This investigation was conducted to evaluate the determinants of post discharge mortality in hospitalized COVID-19 patients, especially 18-45 yr of age.
Methods:
A series of three nested case-control analyses was conducted on follow up data collected in the National Clinical Registry for COVID-19 between September 2020 and February 2023 from 31 hospitals. Matching (1:4) was done by the date of hospital admission ±14 days for the following comparisons: (i) case-patients reported as dead vs. controls alive at any contact within one year follow up; (ii) the same in the 18-45 yr age group and (iii) case-patients reported as dead between the first and one year of follow up vs. controls alive at one year post discharge.
Results:
The one year post discharge mortality was 6.5 per cent (n=942). Age [≤18 yr: adjusted odds ratio (aOR) (95% confidence interval [CI]): 1.7 (1.04, 2.9); 40-59 yr: aOR (95% CI): 2.6 (1.9, 3.6); ≥60 yr: aOR (95% CI): 4.2 (3.1, 5.7)], male gender [aOR (95% CI): 1.3 (1.1, 1.5)], moderate-to-severe COVID-19 [aOR (95% CI): 1.4 (1.2, 1.8)] and comorbidities [aOR (95%CI): 1.8 (1.4, 2.2)] were associated with higher odds of post-discharge one-year mortality, whereas 60 per cent protection was conferred by vaccination before the COVID-19 infection. The history of moderate-to-severe COVID-19 disease [aOR (95% CI): 2.3 (1.4, 3.8)] and any comorbidities [aOR (95% CI): 3 (1.9, 4.8)] were associated with post-discharge mortality in the 18-45-yr age bracket as well. Post COVID condition (PCC) was reported in 17.1 per cent of the participants. Death beyond the first follow up was associated with comorbidities [aOR (95%CI): 9.4 (3.4, 26.1)] and reported PCC [aOR (95% CI): 2.7 (1.2, 6)].
Interpretation & conclusions:
Prior vaccination protects against post discharge mortality till one year in hospitalized COVID-19 patients. PCC may have long term deleterious effects, including mortality, for which further research is warranted.
Keywords
India
observational study
one-year mortality
persistent symptoms
post-acute COVID symptoms
COVID-19 has been causing multiple waves worldwide for over three years now. With the pandemic continuing, the pool of COVID-19 survivors is constantly increasing. It has been well documented that the effects of COVID-19 infection last beyond the acute phase leading to a range of health problems from constitutional symptoms such as fatigue and joint pains to potentially fatal conditions such as coagulation abnormalities and cardiac events1-5. Research has shown that a proportion of people die within one year after experiencing COVID-19 disease6,7. Endothelial damage, viral toxicity, hypercoagulable state and dysregulation of the immune system are some of the mechanisms that have been hypothesized to cause fatal post COVID conditions (PCC)8,9. In addition, multiple news reports have been attributing COVID-19 disease and the COVID-19 vaccine to cause cardiac events and deaths amongst young adults.
Multiple nomenclatures and definitions have been used to describe this phenomenon. The common terms used to refer to this group of illnesses are post-acute sequelae of COVID-19, long COVID or PCC10-12. Understanding the risk factors associated with the development of PCC and the long term effect of PCC on the health of individuals is imperative for providing adequate care management to patients recovering from COVID-19.
This series of retrospective nested case-control analyses were conducted with the objective to evaluate the determinants of one year post discharge mortality in patients hospitalized for COVID-19, especially in the population of 18-45 yr. Another objective was to ascertain whether the presence of PCC had any effect on mortality beyond the first follow up in patients discharged after hospitalization for COVID-19.
Material & Methods
The National Clinical Registry for COVID-19 is an ongoing electronic platform developed and maintained by the Indian Council of Medical Research (ICMR) in collaboration with the Ministry of Health and Family Welfare (MoHFW), Government of India, (GoI), All India Institute of Medical Sciences, and ICMR-National Institute of Medical Statistics (NIMS), New Delhi. The structure and protocol of this registry are available in the public domain (https://www.icmr. gov.in/tab1ar1.html). More details about the functioning of the registry are published elsewhere13.
The study was approved by the Central Ethics Committee on Human Research, ICMR, New Delhi, as well as the Institutional Ethics Committee of all the participating institutes. Written informed consent or audiovisual consent was taken from all participants under follow up after discharge from the hospital.
Participants: The registry has been enroling consecutive SARS-CoV-2 positive hospitalized patients confirmed by reverse transcription polymerase chain reaction (RT-PCR), nucleic acid amplification test, rapid antigen test or any other molecular test across a network of 42 participating hospitals since September 2020. No exclusion criteria were applied. A subgroup of participants were followed up every month after being discharged from the hospital for the first three months post discharge and then once every three months until one year across 31 hospitals. The follow up was primarily telephonic; however, some patients were followed up physically based on the discretion of the treating physician and the policy of the treating hospital.
Data collection & analysis: Data were collected using a pre-structured case report form and entered into an electronic portal developed and maintained by the ICMR-NIMS, New Delhi.
In the present investigation, data from the participants who completed follow up post discharge until February 2023 was included. The study participants were grouped as case-patients and controls based on follow up as described in Table I. Nested case-control analyses were performed for three different scenarios: (i) case-patients reported as dead vs. controls alive at any contact within one year follow up; (ii) case-patients reported as dead vs. controls alive at any contact within one year follow up in the 18-45 yr age group and (iii) case-patients reported as dead between the first and one year of follow up vs. controls alive at one year post discharge. Matching (1:4) without replacement was done by the date of original hospital admission for COVID-19±14 days to balance the circulating variant of the virus and the eligibility for vaccination, which had been staggered. Conditional logistic regression was utilized to estimate the odds ratio with independent covariates such as gender, age, presence of any comorbidities, severity of COVID-19 disease and status of vaccination before COVID-19 infection added at the same time to the model; P<0.05 was considered significant. Data analysis was carried out using STATA v14 (STATA Corp., College Station, Texas, USA).
| Outcome | Case-patients | Controls |
|---|---|---|
| Post discharge death at any time within one year of follow up after discharge of patients hospitalized with COVID-19 | Participants who were reported as dead at any time in one year of follow up after discharge | Participants reported to be alive at any contact in one year of follow up after discharge |
| Post discharge death at any time within one year of follow up after discharge of patients, 18-45 yr, hospitalized with COVID-19 | Participants, 18-45 yr of age, who were reported as dead at any time in one year of follow up after discharge | Participants, 18-45 yr of age, reported to be alive at any contact in one year of follow up after discharge |
| Post discharge death at any time between the first follow up and one year of follow up after discharge (one-year status of these patients was known) | Participants who were reported as dead at any time between the first follow up and one year of follow up after discharge | Participants who were alive at one-year follow up after discharge |
Definitions used in the study:
Post COVID condition (PCC): The World Health Organization (WHO) describes PCC as follows - ‘Post-COVID-19 condition occurs in individuals with a history of probable or confirmed SARS-CoV-2 infection, usually three months from the onset of COVID-19 with symptoms that last for at least two months and cannot be explained by an alternative diagnosis. Common symptoms include fatigue, shortness of breath and cognitive dysfunction, but also others, and generally have an impact on everyday functioning. Symptoms may be new onset, following initial recovery from an acute COVID-19 episode, or persist from the initial illness. Symptoms may also fluctuate or relapse over time’. The WHO includes a wide range of symptoms in others, including constitutional, neurological, cardiovascular and gastrointestinal10. The Centres for Disease Control and Prevention (CDC) defines PCC as signs, symptoms or conditions that persist or develop at four weeks or more after the initial infection12. Since this study was planned before the publication of these definitions, applying them in toto was not feasible. The participants who reported persistent or new onset symptoms of fatigue, breathlessness or neurocognitive abnormalities (a participant was labelled to have cognitive abnormality if on questioning, they replied to be experiencing some difficulties in remembering or concentrating or having brain fog), at the 4-8 wk follow up (first follow up) post discharge, were considered having PCC. Participants who did not report symptoms at 4-8 wk post discharge were considered not having PCC, irrespective of whether they manifested any symptoms later.
For post discharge death, all-cause mortality in the participants who had been alive at the time of discharge from the primary COVID hospital was considered. Any patient who had required oxygen supplementation during the primary admission for COVID-19 was labelled as having a moderate-to-severe disease. The comorbidities considered for analysis included hypertension, diabetes, chronic cardiac disease, chronic kidney disease, asthma, malignancy, chronic pulmonary disease, chronic liver disease, stroke, tuberculosis, chronic neurological disease, rheumatological disease, autoimmune disease, haematological disorders, HIV and hepatitis B or C infection.
Results
Of the 14,419 participants who were followed up at least once between four weeks and one year post discharge, 942 (6.5%) had died and the remaining (93.5%) were reported alive at any contact during one year of follow up. The median duration of death was 28 days from hospital discharge (interquartile range: 10, 68.5 days).
Nested case-control 1: factors associated with post discharge death within one year of follow up: Matching was possible for 941 case-patients in the ratio of 1:4 for the date of admission±14 days with 3760 controls (Fig. 1). The odds of dying were higher among males [adjusted odds ratio (aOR) (95% confidence interval [CI]): 1.3 (1.1, 1.5)], age 60 yr and above [aOR (95% CI): 4.2 (3.1, 5.7)], followed by 40-59 yr [aOR (95% CI): 2.6 (1.9, 3.6)] and 0-18 yr [aOR (95% CI): 1.7 (1.04, 2.9)], among patients with comorbidities [aOR (95% CI): 1.8 (1.4, 2.2)] and among those who had a moderate-to-severe disease to begin with [aOR (95% CI): 1.4 (1.2, 1.8)]. Participants who had received at least one dose of the anti-SARS-CoV-2 vaccine before their COVID-19 infection had a lower risk of post-discharge mortality [aOR (95% CI): 0.4 (0.3, 0.5)] (Table II).
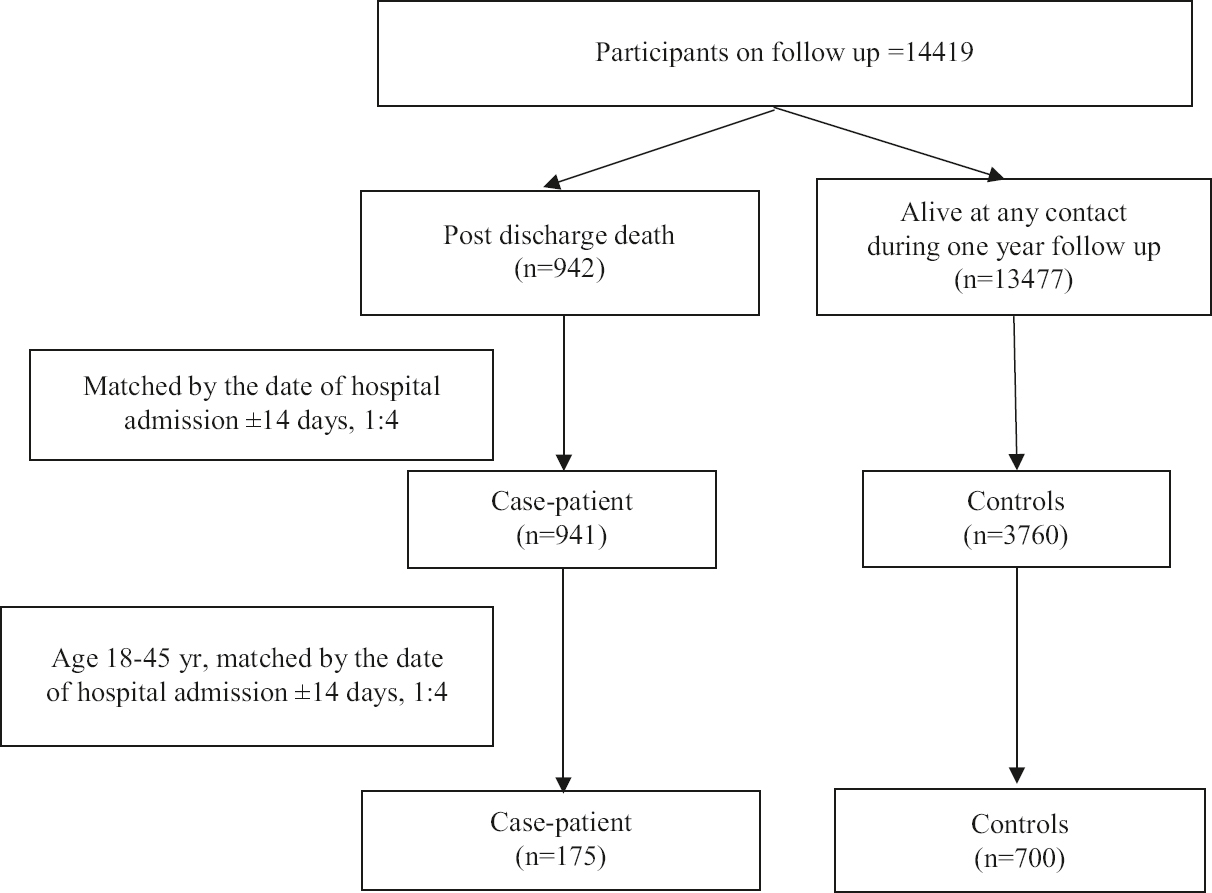
- Participant selection for nested case-control analyses to determine the risk factors of post discharge death within one year of follow up, at all ages and the 18-45 yr age group (matched by the date of hospital admission±14 days, 1:4).
| Characteristic | Participants who died (n=941), n (%) | Participants who survived (n=3760), n (%) | Unadjusted OR (95% CI) | aOR (95% CI) |
|---|---|---|---|---|
| Gender | ||||
| Female | 325 (34.5) | 1488 (39.6) | Reference | Reference |
| Male | 616 (65.5) | 2272 (60.4) | 1.2 (1.1-1.4) | 1.3 (1.1-1.5) |
| Age groups (completed yr) | ||||
| 0-18 | 43 (4.6) | 191 (5.1) | 2.7 (1.8-4.1) | 1.7 (1.04-2.9) |
| 19-39 | 94 (9.9) | 1129 (30) | Reference | Reference |
| 40-59 | 331 (35.2) | 1281 (34.1) | 3.1 (2.4-3.9) | 2.6 (1.9-3.6) |
| 60 and above | 473 (50.3) | 1159 (30.8) | 4.9 (3.9-6.2) | 4.2 (3.1-5.7) |
| Presence of at least one comorbidity | 690 (73.3) | 2033 (54.1) | 2.4 (2-2.8) | 1.8 (1.4-2.2) |
| Moderate-to-severe disease | 597 (63.4) | 1649 (43.9) | 2.3 (2-2.7) | 1.4 (1.2-1.8) |
| Patients vaccinated with at least one dose of the anti-SARS-CoV-2 vaccine | 197 (27.4) | 1080 (38.3) | 0.5 (0.4-0.6) | 0.4 (0.3-0.5) |
Case-patient: reported to have died any time after hospital discharge and within one year of follow up, n=942. Controls: alive at any point of contact after discharge, n=13477. Case-patients were attempted to be matched with controls by the date of admission±14 days in a 1:4 ratio. Successful matches obtained for each case-patient: 0 matched control: 1 (0.1%); 1 matched control: 1 (0.1%); 2 matched controls: 0 (0%) 3 matched controls: 1 (0.1%) and 4 matched controls: 939 (99.7%). To obtain aOR, the conditional logistic regression model was applied, with the independent variables being gender, age groups, severity of disease, presence of comorbidities and vaccination status. OR, odds ratio; aOR, adjusted OR; CI, confidence interval
Nested case–control 2: factors associated with post-discharge death within one year of follow up in the young population of 18-45 yr: Of the 942 deaths, 175 (18.6%) were in the age group of 18-45 yr. These case-patients were matched within±14 days of the date of admission with 700 controls who survived (Fig. 1). In this population of 18-45 yr, the odds of death were higher among those who had suffered from moderate-to-severe COVID-19 disease [aOR (95%CI): 2.3 (1.4, 3.8)] or had any comorbidities [aOR (95%CI): 3 (1.9, 4.8)]. Vaccinated participants had lower odds of dying, although it was not significant (Table III).
| Characteristic | Patients who died (n=175), n (%) | Patients who survived (n=700), n (%) | Unadjusted OR (95% CI) | aOR (95% CI) |
|---|---|---|---|---|
| Gender | ||||
| Female | 62 (35.4) | 270 (38.6) | Reference | Reference |
| Male | 113 (64.6) | 430 (61.4) | 1.1 (0.6-1.8) | 1.3 (0.8-2) |
| Age (yr), mean±SD | 36.3 (7.1) | 31.8 (7.8) | 1.1 (1-1.1) | 1.04 (1.01-1.1) |
| Presence of at least one comorbidity | 111 (63.4) | 208 (29.7) | 4.4 (2.4-8.1) | 3 (1.9,4.8) |
| Moderate-to-severe disease | 102 (58.3) | 192 (27.4) | 3.8 (2.1-7.1) | 2.3 (1.4-3.8) |
| Patients vaccinated with at least one dose of the anti-SARS-CoV-2 vaccine | 25 (20.5) | 156 (33.8) | 0.3 (0.1-0.8) | 0.6 (0.3-1.1) |
Case-patient: 18-45 yr age, reported to have died any time after hospital discharge and within one year of follow up, n=175. Controls: 18-45 yr of age, reported to be alive at any contact after discharge from the hospital, n=1510. Case-patients were attempted to be matched with controls by the date of admission±14 days in a 1:4 ratio. Successful matches obtained for each case-patient: 0 matched control: 0 (0%); 1 matched control: 0 (0%); 2 matched control: 0 (0%) 3 matched control: 0 (0%) and 4 matched control: 175 (100%). To obtain aOR, the conditional logistic regression model was applied, with the independent variables being gender, age, severity of disease, presence of comorbidities and vaccination status
Nested case–control 3: assessing whether post COVID condition (PCC) had any effect on post discharge mortality: Persistent or new onset symptoms or PCC were reported by 1341 (17.1%) of the 7864 patients alive at the first follow up. One hundred and thirteen (1.4%) partcipants had died at any time between the first and one-year follow up post discharge; 112 of such case-patients were matched with 445 controls who were known to be alive at both time points (Fig. 2). The odds of dying after the first follow up at 4-8 wk were higher among those with comorbidity [aOR (95% CI): 9.4 (3.4, 26.1)] and those who reported PCC [aOR (95% CI): 2.7 (1.2, 6)]. The odds of death after the first follow up were lower among those who had a moderate-to-severe disease during initial hospitalization and had received anti-SARS-CoV-2 vaccination, although the association was not significant (Table IV).
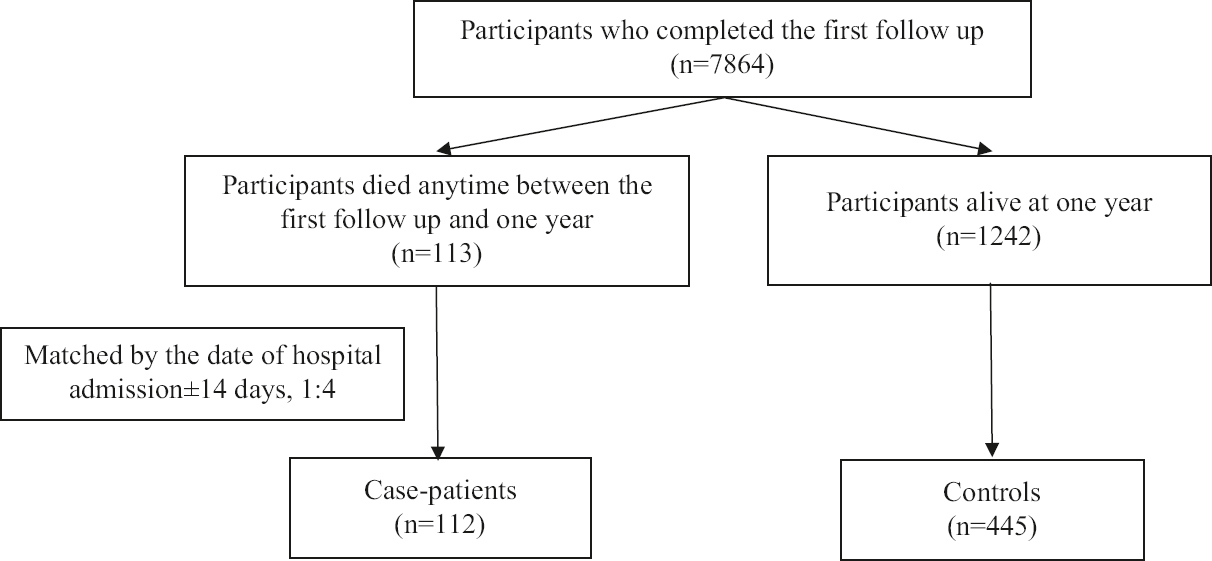
- Participant selection for nested case-control analysis to determine the risk factors of late post discharge death, (beyond the first follow up till one year), in the participants for whom status is known both at the first follow up and one year (matched by the date of hospital admission±14 days, 1:4).
| Characteristic | Patients who died (n=112), n (%) | Patients who survived (n=445), n (%) | Unadjusted OR (95% CI) | aOR (95% CI) |
|---|---|---|---|---|
| Gender | ||||
| Female | 41 (36.6) | 178 (40) | Reference | Reference |
| Male | 71 (63.4) | 267 (60) | 1.1 (0.7-1.8) | 1.3 (0.7-2.5) |
| Age groups (completed yr) | ||||
| 0-18 | 4 (3.6) | 12 (2.7) | 2.9 (0.8-10.2) | 5.6 (0.4-76.1) |
| 19-39 | 15 (13.4) | 132 (29.7) | Reference | Reference |
| 40-59 | 43 (38.4) | 169 (37.9) | 2.2 (1.2-4) | 1.8 (0.7-4.7) |
| 60 and above | 50 (44.6) | 132 (29.7) | 3.3 (1.8-6) | 2.6 (0.9-7.1) |
| Presence of at least one comorbidity | 98 (87.5) | 255 (57.3) | 5.4 (2.9-9.8) | 9.4 (3.4-26.1) |
| Moderate-to-severe disease | 54 (48.2) | 227 (51.0) | 0.9 (0.6-1.4) | 0.3 (0.1-0.6) |
| Persistent symptoms after 4-8 wk of discharge | 32 (28.6) | 92 (20.7) | 1.6 (1-2.5) | 2.7 (1.2-6) |
| Patients vaccinated with at least one dose of the anti-SARS-CoV-2 vaccine | 20 (27) | 107 (38.9) | 0.6 (0.3-1.1) | 0.6 (0.3-1.2) |
For this analysis, both cases and controls were obtained from only those participants who had recorded a follow up at 4-8 wk post-discharge (first follow up), and the outcome at one year was known. Case-patient: reported to have died any time after the first follow up and one year of follow up, n=113. Controls: alive till at least one year after discharge from the hospital, n=1242. Case-patients were attempted to be matched with controls by the date of admission ±14 days in a 1:4 ratio. Successful matches obtained for each case-patient: 0 matched control: 1 (0.9%); 1 matched control: 0 (0%); 2 matched control: 1 (0.9%); 3 matched control: 1 (0.9%) and 4 matched control: 110 (97.3%). To obtain aOR, the conditional logistic regression model was applied, with the independent variables being gender, age groups, severity of disease, presence of comorbidities and vaccination status before COVID-19 infection
Discussion
The current nested case-control analyses highlighted the factors associated with post discharge deaths among patients previously hospitalized for COVID-19 disease.
In our analyses, 6.5 per cent post discharge mortality was reported in one year. This is comparable to data being generated worldwide. A systematic review of 43 studies reported all-cause mortality during one-year post-discharge as 7.5 per cent6. We observed that the male gender, age above 40 yr, history of moderate-to-severe COVID-19 disease and presence of comorbidities increased the odds of death within one year of discharge from the hospital. Multiple studies have identified increasing age as a risk factor for post discharge death14-16. The current analysis additionally showed that the participants younger than 18 yr had 1.7 times higher odds of dying after discharge from the hospital. Our earlier reports have shown that comorbidities among admitted children are more severe, such as malignancies, kidney disorders, haematological disorders and others13,17. This could be hypothesized as one of the reasons for the higher odds of death among these children. Novelli et al18 described previously existing comorbidities, including cancer, diabetes, cardiac diseases, immunosuppression and vasculopathies, as associated with post discharge mortality. Moderate-to-severe disease, being linked to post discharge all-cause mortality, indicates lingering damage due to COVID-19. Although some reports have claimed that the severity of pneumonia had no bearing on post discharge mortality, many have documented the association of intensive care unit stay or mechanical ventilation with post discharge mortality18,19.
Fortunately, vaccination against COVID-19 before contracting the infection provided around 60 per cent protection against post discharge death. In a recent living systematic review and meta-analysis, vaccine effectiveness against mortality after the primary schedule of anti-COVID-19 vaccination was observed to have reduced after 168-195 days but was still around 86 per cent20. Protection against all-cause mortality at the one-year post-acute phase of COVID-19 has not been documented for anti-SARS-CoV-2 vaccines.
Emphasis was put on the 18-45 yr of age to understand the factors associated with post discharge death in young adults. Factors associated with death in them after discharge were similar to the ones observed in other age brackets. Prior anti-COVID-19 vaccination did lend some protection against all-cause post discharge death in this age group, although this cannot be claimed conclusively as the association was not statistically significant.
Post COVID condition was reported by 17.1 per cent of the participants at 4-8 wk follow up. According to the WHO, the current rate of PCC is 10-20 per cent21. There is variability in the prevalence of PCC reported across different studies, ranging from 50 per cent at six month follow up in a cohort from Moscow to 6.2 per cent in a modelled estimate based on a meta-analysis of 54 studies22,23. Such wide variability has stemmed from the differences in definitions used and assessment time points. The exact mechanistic pathway of developing PCC is unclear. Various hypotheses have been postulated, including prolonged inflammation, organ damage due to the virus, endothelial dysfunction and hypercoagulable state leading to thrombo-embolic phenomenon24.
In the present investigation, the history of PCC was associated with 2.7 times higher odds of post discharge mortality. The National Centre for Health Statistics, USA, released a report on death certificate analysis. The age-adjusted death rate for long COVID was estimated to be 6.3/1 million population in a 12 month period25. The presence of any comorbidities was another important predictor of late post discharge death. It is difficult to ascertain whether the comorbid condition causing death was unrelated to the COVID-19 infection or the viral infection and its long-term effects exacerbated the comorbid condition culminating in death. Interestingly, those with moderate-to-severe disease had lower odds of dying after an initial period of 60 days. It could be hypothesized that these patients would have been under a more stringent follow up and would have had better health seeking behaviour as a response to the initial critical event. Encouragingly, although not statistically significant, vaccination before COVID-19 infection conferred around 40 per cent protection to late deaths between 60 days and one-year post discharge.
The limitations of the current investigation include reliance on telephonic follow up, which could have led to under reporting of the symptoms. The present analyses only included patients who were hospitalized due to COVID-19, and consequently, the findings cannot be generalized to all patients who had COVID-19. Furthermore, the operational definition of PCC used in this study is not an exact match to either the WHO or CDC definition mentioned earlier. This variation of the definition for PCC may be a source of bias. In the first two nested case-control analyses, it is possible that the participants could have died sometime after being contacted and were misclassified as controls rather than cases. However, we do not expect any major bias to arise, as this misclassification would have made the analyses more conservative.
Overall, the study findings suggest that a post discharge mortality rate of 6.5 per cent in patients hospitalized for COVID-19 warrants a vigilant follow up. Younger as well as older age, male gender, moderate-to-severe disease and presence of comorbidities are associated with higher odds of post-discharge one-year mortality. Encouragingly, vaccination before the COVID-19 infection confers protection to post discharge mortality. PCC and the presence of comorbidities may have some association with late post discharge deaths; further research is warranted in this field.
Financial support and sponsorship
None.
Conflicts of interest
None.
References
- More than 50 long-term effects of COVID-19: A systematic review and meta-analysis. medRxiv 2021 Doi: 2021.01.27.21250617
- [Google Scholar]
- Neurocognitive and psychiatric symptoms following infection with COVID-19: Evidence from laboratory and population studies. Brain Behav Immun Health. 2023;28:100595.
- [Google Scholar]
- Frequent neurocognitive deficits after recovery from mild COVID-19. Brain Commun. 2020;2:fcaa205.
- [Google Scholar]
- Hospital readmissions and post-discharge all-cause mortality in COVID-19 recovered patients;a systematic review and meta-analysis. Am J Emerg Med. 2022;51:267-79.
- [Google Scholar]
- Readmissions, postdischarge mortality, and sustained recovery among patients admitted to hospital with coronavirus disease 2019 (COVID-19) Clin Infect Dis. 2023;76:e82-82.
- [Google Scholar]
- The COVID heart-one year after SARS-CoV-2 infection, patients have an array of increased cardiovascular risks. JAMA. 2022;327:1113-4.
- [Google Scholar]
- Risk of acute myocardial infarction and ischaemic stroke following COVID-19 in Sweden: A self-controlled case series and matched cohort study. Lancet. 2021;398:599-607.
- [Google Scholar]
- A clinical case definition of post COVID-19 condition by a Delphi consensus. Available from: https://apps.who.int/iris/bitstream/handle/10665/345824/WHO-2019-nCoV-Post-COVID-19-condition-Clinical-case-definition-2021.1-eng.pdf?sequence=1&isAllowed=y
- National comprehensive guidelines for management of post-covid sequelae. Available from: https://www.mohfw.gov.in/pdf/NationalComprehensiveGuidelinesforManagementof PostCovidSequelae.pdf
- Long COVID or post-COVID conditions. Available from: https://www.cdc.gov/coronavirus/2019-ncov/long-term-effects/index.html
- Vaccination saves lives: A real-time study of patients with chronic diseases and severe COVID-19 infection. QJM. 2023;116:47-56.
- [Google Scholar]
- Readmission and death after initial hospital discharge among patients with COVID-19 in a large multihospital system. JAMA. 2021;325:304-6.
- [Google Scholar]
- 6-month mortality and readmissions of hospitalized COVID-19 patients: A nationwide cohort study of 8,679 patients in Germany. PLoS One. 2021;16:e0255427.
- [Google Scholar]
- Thirty-day post-discharge outcomes following COVID-19 infection. J Gen Intern Med. 2021;36:2378-85.
- [Google Scholar]
- Evaluation of a hospitalized pediatric COVID-19 cohort from Indian national clinical registry of COVID-19. Indian J Pediatr 2023 Doi:10.1007/s12098-022-04449-w
- [Google Scholar]
- One-year mortality in COVID-19 is associated with patients'comorbidities rather than pneumonia severity. Respir Med Res. 2023;83:100976.
- [Google Scholar]
- Survival after hospital discharge in patients hospitalized for acute coronavirus disease 2019: Data on 2586 patients from a tertiary center registry. Croat Med J. 2022;63:335-42.
- [Google Scholar]
- Long-term effectiveness of COVID-19 vaccines against infections, hospitalisations, and mortality in adults: Findings from a rapid living systematic evidence synthesis and meta-analysis up to December,. Lancet Respir Med. 20222023;11:439-52.
- [Google Scholar]
- Coronavirus disease (COVID-19): Post COVID-19 condition. Available from: https://www.who.int/news-room/questions-and-answers/item/coronavirus-disease-(covid-19)-post-covid-19-condition
- Prevalence and risk factors of post-COVID-19 condition in adults and children at 6 and 12 months after hospital discharge: A prospective, cohort study in Moscow (StopCOVID) BMC Med. 2022;20:244.
- [Google Scholar]
- Estimated global proportions of individuals with persistent fatigue, cognitive, and respiratory symptom clusters following symptomatic COVID-19 in 2020 and 2021. JAMA. 2022;328:1604-15.
- [Google Scholar]
- Identification of deaths with post-acute sequelae of COVID-19 from death certificate literal text: United States, January 1, 2020-June 30, 2022. Available from: https://stacks.cdc.gov/view/cdc/121968
- [Google Scholar]






