Translate this page into:
A preliminary study on contact tracing & transmission chain in a cluster of 17 cases of severe acute respiratory syndrome coronavirus 2 infection in Basti, Uttar Pradesh, India
For correspondence: Dr Rajni Kant, ICMR-Regional Medical Research Centre, Gorakhpur 273 013, Uttar Pradesh, India e-mail: rajnikant.srivastava@gmail.com
-
Received: ,
This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
This article was originally published by Wolters Kluwer - Medknow and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Background & objectives:
Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection has spread rapidly, causing unprecedented case fatalities across the world. The first laboratory-confirmed case of COVID-19 and also the first death associated with the disease in the eastern part of Uttar Pradesh (UP) was reported from Basti on March 31, 2020. The present study describes a cluster of 17 cases including one death of confirmed COVID-19 in Basti, UP, India.
Methods:
A 25 year old male from Basti, UP, India, who died of respiratory failure was diagnosed post-mortem as SARS-CoV-2 positive. Contact tracing carried out by the district administration found 16 cases positive among tested contacts. A detailed retrospective investigation in the form of one-to-one interview was carried out with 16 recovered individuals to understand the transmission dynamics and clinical characteristics.
Results:
The findings showed that the cluster transmission occurred at three levels: first was direct contact with the index case which resulted in two secondary cases. Second, at a household level where four of the seven susceptible contacts got infected, and the third was an event (funeral) where 50 individuals participated and this resulted in seven SARS-CoV-2-infected individuals in whom infection could be directly linked to a funeral gathering. The index case had associated comorbidities and succumbed to death. Most of the cases were asymptomatic except two individuals, who developed mild symptoms. The mean duration of quarantine facility was 21.6±7.3 days, and the average time taken for the first negative test after testing positive to COVID-19 was 12±4.1 days.
Interpretation & conclusions:
The funeral acted as a super-spreader event for the transmission of infection among family members, relatives and others. Active contact tracing and confirmation of infection among the contacts led to the isolation of 16 SARS-CoV-2 positive cases and hence the limited spread of the disease. Asymptomatic carriers and super-spreader events are among the major challenges in the control and prevention of SARS-CoV-2 transmission. Early testing, quarantine and social distancing may play key role in breaking the chain of transmission.
Keywords
Cluster
COVID-19
India
SARS-CoV-2
transmission
Uttar Pradesh
The ongoing COVID-19 pandemic which originated in December 2019 from the Wuhan city of Hubei Province of China, spread rapidly across the globe with >19 million laboratory-confirmed cases of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection, resulting in >0.7 million deaths worldwide in just eight months1.
In India, the first laboratory-confirmed case was reported from Kerala in a student who returned from Wuhan on January 30, 20202. Person-to-person transmission has also been shown3. As of August 1, 2020, the total number of laboratory-confirmed cases of infection in India was over >1.7 million cases, with >35000 deaths4. The first laboratory-confirmed COVID-19 case and also the first death associated with the disease in the eastern part of Uttar Pradesh (UP) was reported from Basti on March 31, 20204. We report herewith a cluster of 17 laboratory-confirmed cases from Basti to provide an insight into the transmission chain and clinico-epidemiological characteristics of SARS-CoV-2-infected individuals.
Material & Methods
The present study was conducted in the ICMR-Regional Medical Research Centre (ICMR-RMRC), Gorakhpur, UP, India, during May 12-31, 2020, as a part of the project (RMRCGKP/EC/2020/1.2) entitled “Clinico-epidemiological dimensions of COVID-19 during infection & post-discharge: A case series in and around Gorakhpur in Eastern Uttar Pradesh”, which was approved by the Institutional Human Ethics Committee (EC/NEW/INST/2019/191). All participants were informed about the objectives of the study. Written informed consent was obtained from each participant. In the case of participants <18 yr of age, assent of the child and consent of parents/guardians were taken.
A 25 yr old male from Basti, UP, was admitted to the Medical Emergency department in BRD Medical College, Gorakhpur, on March 29, 2020, having acute respiratory distress syndrome (ARDS) with multiorgan dysfunction syndrome (MODS) and respiratory failure and succumbed to death. Post-mortem sample tested positive for SARS-CoV-2. Later, the local authorities traced his close contacts according to guidelines issued by the WHO and the Ministry of Health and Family Welfare, Government of India56 at that time. People from the market where the index case had his shop, his treating physicians, people who attended his funeral, family members and friends were traced. Throat and deep nasal swabs were taken from all these contacts. A total of 16 individuals were found SARS-COV-2 positive. All these individuals were included in the study by conducting one-to-one interview. A semi-structured interview schedule was used for data collection, and interviews were conducted by trained medical personnel. Data regarding basic socio-demographic characteristics, clinical features, comorbidity, personal history, recent travel history, date of diagnosis, discharge etc., were collected from these individuals who were discharged from hospitals/isolation facilities after recovery from infection. Details about the presence of both typical and atypical symptoms such as cough, cold, sore throat, fever, chills, fatigue, loss of appetite, diarrhoea, new loss of taste or smell, shortness of breath, headache and muscular pain were also collected. Cases were given an alphanumeric code for identification where the alphabet denoted family (A, B…) and the number denoted family member (A1, E1…).
The results of the throat and deep nasal swab specimens tested for SARS-CoV-2 by real-time reverse transcription-polymerase chain reaction (RT-PCR) assay7 were collected, and their association with the viral clearance and incubation period was analyzed. The collected data were entered in MS Excel sheet; derived variables were generated where required and calculations of frequency, means, median etc., were done.
Results & Discussion
A total of 17 individuals were studied, among whom one had succumbed to death and was diagnosed having SARS-CoV-2 infection post-mortem. He (case A1) was a 25 yr old male and a shopkeeper in the local market. He had a history of recurrent episodes of pneumonia in the past and also a history of liver disease, according to his brother. He was taking treatment from a local private medical practitioner for about the last two years. On worsening of the health condition, he was admitted to the BRD Medical College where he died during treatment on March 30, 2020. He had no travel history outside the district/his place of stay was Basti for the last six months and also no one from his family had any history of travel outside Basti. No evidence for the source of infection could be traced. With the clinical suspicion for the sudden death, throat and nasal swabs were collected for SARS-CoV-2 testing post-death. His medical certification of death reported death due to sudden cardio-pulmonary arrest (ARDS, MODS and respiratory failure).
By the time confirmatory laboratory results were available on March 31,2020, the family and relatives practiced burial ceremony, which turned out to be a super-spreader event. As soon as contact tracing and quarantine of the suspected individuals was started, the infection was already transmitted to the family members and their close contacts56.
Funeral super-spreader event: About 50 individuals attended the funeral of case A1, as per the details obtained from the District Health and Administration and family members. The active contact tracing and quarantine exercise was initiated by the local health department and samples were collected from the contacts. Among the 39 individuals who attended the funeral and were quarantined and tested, seven tested positive for the infection. A total of three other family members of these seven infected individuals also tested positive. These were case C (a 32 yr old male), case D1 (a 45 yr old male), case D2 (a 21 yr old male), case D3 (a 18 yr old female), case E1 (a 28 yr old male), case E2 (a 15 yr old female), case F1 (a 50 yr old male), case F2 (a 45 yr old female), case F3 (a 17 yr old male) and case G (a 50 yr old male). Among them, only two (cases D1 and E2) developed symptoms that were mild and relieved by medication within 3-4 days. Case D1 had cough which got relieved in three days by taking azithromycin and multivitamin supplements. Case E2 developed fever with cough, and she was treated with paracetamol, azithromycin and multivitamin supplements.
Case B was a 26 yr old male who accompanied case A1 to the District Hospital, Basti, got himself tested out of suspicion and was tested positive for the infection on March 31, 2020. He was admitted to the isolation facility thereafter. He was asymptomatic during the period of isolation. Among his six-member family, all others were tested negative and on repeat testing after 14 days they did not complain about any symptom either. Case A5 was a 28 yr old male, brother-in-law of case A1, who accompanied him during a hospital visit in Gorakhpur and also accompanied the dead body back to Basti. He was tested positive after four days of funeral (April 4, 2020) along with his wife (case A6, a 26 yr old female) who travelled from Gorakhpur to Basti along with his husband. Both of them remained symptom free during the entire isolation period.
The index case A1 had a seven-member family and four were tested positive for the SARS-CoV-2 infection including himself [case A2 - his mother (a 45 yr old female), case A3 and case A4 - his two brothers aged 30 and 21 yr, respectively, were tested positive on April 2, 2020]. None of them reported any symptoms before or during isolation. The other three family members (his father and two sisters) were found free of the infection even on repeat testing after 14 days and did not have any symptom.
Clinical features: The majority of cases were male (12, 70.6%), and the median age was 28 yr (range: 15-50). The median family size was seven (range: 2-8). The majority (82%) of them were asymptomatic except for two cases who showed mild illness (cases D1 and E2). A history of comorbid illness was found in two individuals. None had a history of recent travel and recent respiratory illness. All the 16 cases had a history of contact with the deceased case during his course of illness and at the funeral (Table). The secondary attack rate of 45.5 per cent was found in the present cluster, which indicated the high infectivity of SARS-CoV-2.
| Characteristics | Frequency (%) |
|---|---|
| Age (yr) | |
| Median | 30 (range: 15-50) |
| 10-19 | 3 (17.6) |
| 20-40 | 9 (52.9) |
| 41-60 | 5 (29.4) |
| Gender | |
| Female | 5 (29.4) |
| Male | 12 (70.6) |
| Marital status | |
| Married | 10 (58.8) |
| Unmarried | 7 (41.2) |
| Symptoms | |
| Fever | 1 (5.8) |
| Cough | 3 (17.6) |
| Shortness of breath | 1 (5.8) |
| Atypical clinical feature | 0 |
| Asymptomatic | 14 (82.3) |
| Comorbid illnesses | |
| Liver disease | 1 (5.8) |
| Lung disease | 1 (5.8) |
| No comorbidity | 16 (94.1) |
| Outcome | |
| Recovered | 16 (94.1) |
| Death | 1 (5.8) |
| Duration of isolation (in days) (n=16) | |
| Median | 19 (range: 11-33) |
| 10-14 | 1 (6.3) |
| 15-19 | 7 (43.8) |
| 20-24 | 2 (12.5) |
| 25-29 | 2 (12.5) |
| 30-34 | 4 (25.5) |
| Median | 12 (range: 6-23) |
| <10 | 2 (12.5) |
| 10-14 | 11 (68.8) |
| >14 | 3 (18.8) |
All the 16 cases recovered clinically, with complete viral clearance proved by two consecutive negative samples tested 24 h apart. The average time taken for the first negative test after testing positive to COVID-19 was 12±4.11 days. The detailed sequential real-time RT-PCR cycle threshold (Ct) values for all the 17 patients on the day of positivity are shown in the Figure. The longer duration of viral clearance was noted in case B (23 days), case A5 (19 days) and case A6 (26 days), which was associated with their respective Ct values, indirectly depicting the high viral load. The mean duration of quarantine/isolation was 21.56±7.26 days.
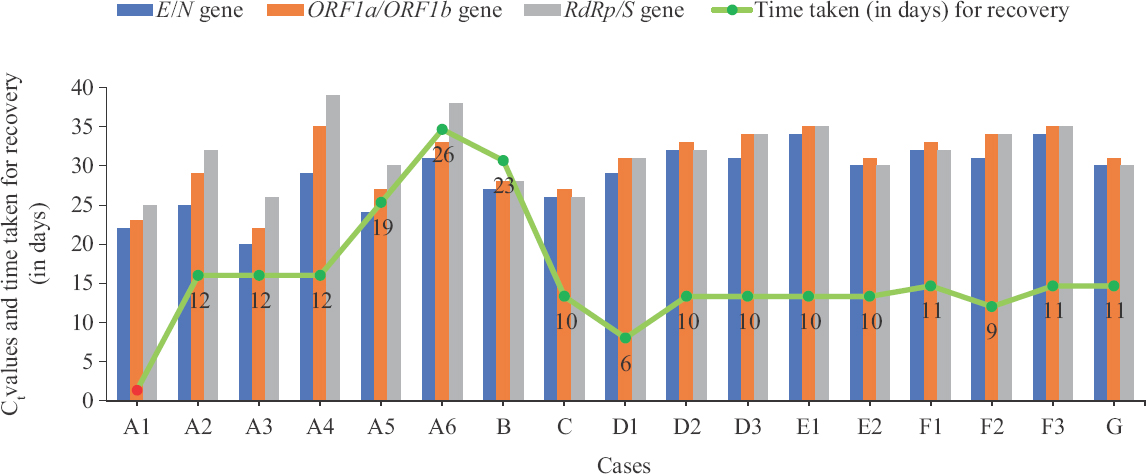
- Comparison of the cycle threshold (Ct) values of real-time RT-PCR on the day of positivity and time taken for recovery in terms of PCR-negative results of 17 laboratory-confirmed cases of SARS-CoV-2 infection. Index case A1 (red dot) deceased.
The majority (82.3%) of individuals (n=14) in this cluster recovered from infection without developing any symptom. Only two developed mild symptoms and the intra-cluster case fatality rate was 5.8 per cent (1/17) with one death. Similar findings have been reported from Bhilwara District, Rajasthan, India8. The less proportion of symptomatic individuals in this study may be due to early diagnosis and isolation, absence of comorbidity and relatively younger age, as compared to findings of other studies from different parts of the globe910111213.
In our study, transmission occurred at three levels: first was direct contact with the index case which resulted in two secondary cases. Second, at the household level where four of seven susceptible contacts got infected, and the third was an event (funeral) where 50 people participated and this resulted in seven positive individuals, in whom the infection was directly linked to a funeral gathering as there was no interaction after this. This event turned out to be a super-spreader event14. Later, these seven positives transmitted the infection to three of their household members. This indicates that asymptomatic cases can silently transmit infection as reported from other studies21516.
Our preliminary study had certain limitations. A clear infector-infectee relationship could not be defined because all the households were linked by either vicinity or relation, and also it was not clear that from whom or where the index case got infected. A phylogenetic analysis of the virus was not done, which could have helped in confirming the presumed epidemiological linkage for the infection transmission. The present study being conducted on a small group of individuals and localized to a small geographical area, the findings cannot be generalized. Findings of this study are interview based of the individuals recovered from the infection, which may not be the complete number.
This study shows the impact of an effective contact tracing and isolation towards prevention and control of an infectious disease where person-to-person transmission is known to occur3917 and proportion of asymptomatic cases is high. High proportion of asymptomatic cases poses a challenge in the prevention and control of an epidemic especially when the prevalence of the infection goes beyond the tracking and tracing capabilities of the system. In addition, younger age and absence of comorbidity seem to help in minimizing the severity of illness. Testing, contact tracing, containment and strict adherence to social distancing, following hygienic practices, avoiding crowded places and wearing mask may play a key role in breaking the chain of transmission.
Acknowledgment
Authors acknowledge the Basti District Health authorities and District Administration for their support and help in the study, and thank all the participants and their families involved in the study.
Financial support & sponsorship: This study was financially supported by the ICMR-RMRC Gorakhpur Intramural project fund.
Conflicts of Interest: None.
References
- Coronavirus Disease 2019 (COVID-19) Dashboard. Available from: https://covid19whoint/
- First confirmed case of COVID-19 infection in India: A case report. Indian J Med Res. 2020;151:490-2.
- [Google Scholar]
- A familial cluster of infection associated with the 2019 novel coronavirus indicating possible person-to-person transmission during the incubation period. J Infect Dis. 2020;221:1757-61.
- [Google Scholar]
- Available from: https://www.mohfw.gov.in/
- Considerations in the investigation of cases and clusters of COVID-19. Available from: https://wwwwhoint/publications/i/item/considerations-in-the-investigation-of-cases-and-clusters-of-covid-19
- Containment Plan: Novel Coronavirus Disease 2019 (COVID 19). Version 2 (updated 16.05.2020). Available from: https://www.mohfw.gov.in/pdf/Containmentplan16052020.pdf
- Laboratory preparedness for SARS-CoV-2 testing in India: Harnessing a network of virus research & diagnostic laboratories. Indian J Med Res. 2020;151:216-25.
- [Google Scholar]
- Insights from COVID-19 cluster containment in Bhilwara District, Rajasthan. Indian J Public Health. 2020;64:S177-82.
- [Google Scholar]
- Early transmission dynamics in Wuhan, China, of novel coronavirus-infected pneumonia. N Engl J Med. 2020;382:1199-207.
- [Google Scholar]
- Epidemiology and transmission of COVID-19 in 391 cases and 1286 of their close contacts in Shenzhen, China: A retrospective cohort study. Lancet Infect Dis. 2020;20:911-9.
- [Google Scholar]
- Epidemiologic and clinical characteristics of novel coronavirus infections involving 13 patients outside Wuhan, China. JAMA. 2020;323:1092-3.
- [Google Scholar]
- Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: A descriptive study. Lancet. 2020;395:507-13.
- [Google Scholar]
- Epidemiology, causes, clinical manifestation and diagnosis, prevention and control of coronavirus disease (COVID-19) during the early outbreak period: A scoping review. Infect Dis Poverty. 2020;9:29.
- [Google Scholar]
- Significance of super spreader events in COVID-19. Indian J Public Health. 2020;64:S139-41.
- [Google Scholar]
- Virology, epidemiology, pathogenesis, and control of COVID-19. Viruses. 2020;12:372.
- [Google Scholar]
- Impact of nonpharmacological interventions on COVID-19 transmission dynamics in India. Indian J Public Health. 2020;64:S142-6.
- [Google Scholar]
- A familial cluster of pneumonia associated with the 2019 novel coronavirus indicating person-to-person transmission: A study of a family cluster. Lancet. 2020;395:514-23.
- [Google Scholar]






