Translate this page into:
Epidemiological scenario of leprosy in marginalized communities of India: Focus on scheduled tribes
For correspondence: Dr Pushpendra Singh, Microbial Pathogenesis & Genomics Laboratory, ICMR-National Institute of Research in Tribal Health, Jabalpur 482 003, Madhya Pradesh, India e-mail: pushpendra.S@icmr.gov.in
-
Received: ,
This article was originally published by Wolters Kluwer - Medknow and was migrated to Scientific Scholar after the change of Publisher.
Abstract
The Scheduled Tribes (STs) are designated among the most disadvantaged social groups in India. Until the year 2005 (pre-elimination era of leprosy in India), several leprosy-specific control field programmes were implemented, which have been discontinued subsequently. Since then, leprosy diagnosis and treatment have been integrated with General Health Services. Thereafter, specialized expertise for the early diagnosis of leprosy has been gradually diminishing, especially at the peripheral clinics in remote areas. Hence, leprosy cases usually remain undetected for a long time and persist as endemic reservoirs. The tribal population of India accounts for just 8.6 per cent of the overall population. However, 18.5 per cent of the new leprosy cases were detected within the tribal community in the year 2020, indicating a disproportionately high burden of leprosy among the tribal population. Recent data suggest that these health disparities can be mainly related to the increased marginalization of STs as compared to other communities. This shows the need to further explore the current situation of leprosy in STs so that suitable interventions can address the contributing factors, leading to health inequalities in disadvantaged socio-economic groups. Therefore, this review aims to present the current distribution of leprosy in marginalized communities with a special emphasis on STs. Further, this review discusses how resources might be mobilized for such communities to find and treat undetected leprosy patients in STs to enable effective control of leprosy through early detection and timely treatment.
Keywords
Burden
elimination
evaluation
leprosy
tribal
Leprosy or Hansen’s disease is one of the world’s oldest diseases. It is caused by uncultivated mycobacterial pathogens, Mycobacterium leprae and M. lepromatosis. Leprosy usually presents as patches/lesions on the skin. Leprosy bacilli affect peripheral nerves, eyes and the mucosa of the upper respiratory tract1,2. The physical symptoms include having patches on pale and reddish skin (usually flat, that may be numb and look faded), numbness in limbs (hands and feet), loss of sensation in the affected patch of skin, accompanied by loss of eyebrows and eyelashes in some cases3,4. The routes of M. leprae transmission are still not entirely known5,6. Although there is compelling evidence of increased risk of infection due to close and prolonged contact with an index case through aerosols generated during coughing and sneezing, there is also a possibility of direct and indirect exposure from the environment, or via direct contact. However, it is generally emphasized that leprosy cannot simply be acquired by casual contact with an uninfected person7. The incubation period of M. leprae might last anywhere from a few weeks to more than two decades8. Only a small fraction of infected people contract leprosy, the majority (>80%) of the population can resist leprosy owing to genetic factors9,10. Leprosy occurs in many regions of the world, but over three quarters of all the cases are reported from Brazil, India and Indonesia9,11. The likelihood of leprosy infection is also correlated with socio-economic conditions and poverty12,13. A mix of variables such as crowded settings and poor hygiene may also result in increased chances of transmission. Malnutrition, as well as other comorbidities, may be the factors associated with leprosy to consider it as a disease of poverty14,15. While leprosy treatment is free in India as also around the world, the cost of travel and the associated loss of wages, failure of surveillance mechanisms in endemic areas and a lack of information about the availability of treatment are significant barriers to treatment16,17. Discontinuation of specialized leprosy hospitals and stopping the treatment follow up and surveillance activities can contribute to poor adherence to treatment.
Many individuals having leprosy or leprosy-like symptoms might avoid or postpone looking for care, conceal the condition of the disease or stop the ongoing treatments18,19. The social stigma associated with leprosy is also a major deterrent for people while seeking treatment18,20. Even nowadays, a sizeable number of cases have been identified within Schedule Caste (SC) and Scheduled Tribe (ST) communities with a prevalence rate of leprosy as high as 4.5/10,000 in contrast to the national level figures of 0.6/10,000 population, which demonstrates a high burden of leprosy in certain pockets of India21,22.
Despite this, little is known about the current situation of leprosy in the ST population as the information about social group or caste (whether SC/ST/OBC, etc.) is not recorded during the documentation of cases.
Search strategy: Leprosy prevalence rate provides insight into disease transmission patterns as well as serves as an indicator of the efficacy of public health schemes in different geographical regions and communities. After attaining the leprosy elimination goal in 2005, there is still no comprehensive data regarding the prevalence of leprosy among SCs and STs. Most of the epidemiological studies demonstrate that NLEP contributed by sustaining the control efforts in all sections of the society, including tribal populations; however, there is a need to improve the surveillance efforts in hyperendemic areas and populations with higher prevalence of disease, such as in tribal populations in difficult terrain. To provide a comprehensive guide for future studies and policies, research articles from MEDLINE were identified using the following keywords: “Leprosy”, “Tribal”, “Leprosy” India Tribal, “Adivasi leprosy” and “Indian tribal leprosy”. Papers were selected if they included epidemiological aspects of leprosy in the tribal regions of India. However, most studies were related to traditional knowledge about the usage of medicinal plants for treating leprosy and leprosy-like presentations. The extended Google search was done again using the same keywords to get the reports from NGOs and news articles that shed light on leprosy in tribals. Many studies/reports have focussed on determining the societal perceptions of leprosy, however, only a few publications are available on the epidemiological situation of leprosy among tribals23-25. Compiling these studies will be useful to obtain a broad overview of the situation. Hence, this literature review aimed to consolidate this knowledge on the present situation of leprosy in tribal areas based on various sources of information.
Current scenario
With over 1.14 lakh new leprosy cases detected in 2020, India accounts for >55 per cent of the total cases reported globally, indicating an active transmission, especially in certain pockets of hyperendemicity11. By bringing down the prevalence rate <1/10,000 at the national level, India had officially reached the leprosy elimination goal, as a public health issue (Prevalence rate <1 per 10,000 population as defined by the WHO) in 200526. However, leprosy remains endemic in several States and Union Territories of India, where prevalence was > 1/10,000, such as Jharkhand, Chhattisgarh, the UT of Chandigarh, Dadra and Nagar Haveli, Maharashtra, Odisha and Bihar. In the post-elimination era of leprosy, major structural changes were made by the National Leprosy Eradication Programme (NLEP) and the Global Leprosy Plan27. These changes were aimed at reducing disability and improving the detection of new cases, especially among children below 15 yr of age. However, the pace did not go as planned and deficiencies in attaining these targets continue to persist to this day. As per the latest available data for 2019-2020, the Grade 2 Disability (G2D) is identified in 2.41 per cent of leprosy cases, with a G2D rate of 1.96 per million population. A recent five-year retrospective analysis reported the G2D in children as high as 14 per cent, suggesting a diagnostic delay28. Moreover, around 77 per cent of the total districts in the country have ANCDR <10 per 100,000 population (NLEP report)29. However, in the remaining 23 per cent districts, it is important to investigate the underlying epidemiological/demographic factors so that a revised optimal strategy can be implemented there.
Scheduled castes (SCs) and scheduled tribes (STs)
Caste system is commonly practised in India. Scheduled Castes (SCs) and STs are economically deprived communities with a greater chance of living in unfavourable circumstances30-32. SCs and STs are the most neglected communities of India that have often experienced a higher level of poverty and discrimination33,34. STs face more marginalization in Indian society as compared to SCs35. Several independent studies also revealed the disproportionate burden of leprosy cases in these communities17, 23-25,36-38. The ST is the collective word for Indian subcontinent tribes that are considered indigenous to places in India where they live. As per the census report 201139, they account for 8.6 per cent of the total population of India and comprise 705 tribes. Similarly, the population of the SC or Dalits represents 16.6 per cent of the Indian population. Together, SCs and STs comprise roughly 25 per cent of the total population, but these account for 37.6 per cent of all new leprosy cases detected in the country, and therefore, leprosy is starting to become a disease mostly in the marginalized and neglected communities39,40. A further breakdown of these figures revealed that while the proportion of new leprosy cases among the SC population has remained almost constant over the years, there has been a continuous increase in the proportion of new cases belonging to the ST population. The proportion of SC cases of leprosy remains between 18 and 19 per cent in the past decade. However, the proportion of new cases of leprosy among STs grew from 13.3 per cent in 2009 to 18.8 per cent in 2017 (Fig. 1). This is a matter of concern that may highlight a possibility of inadequate efficacy and/or access to leprosy control programmes among the ST population40.
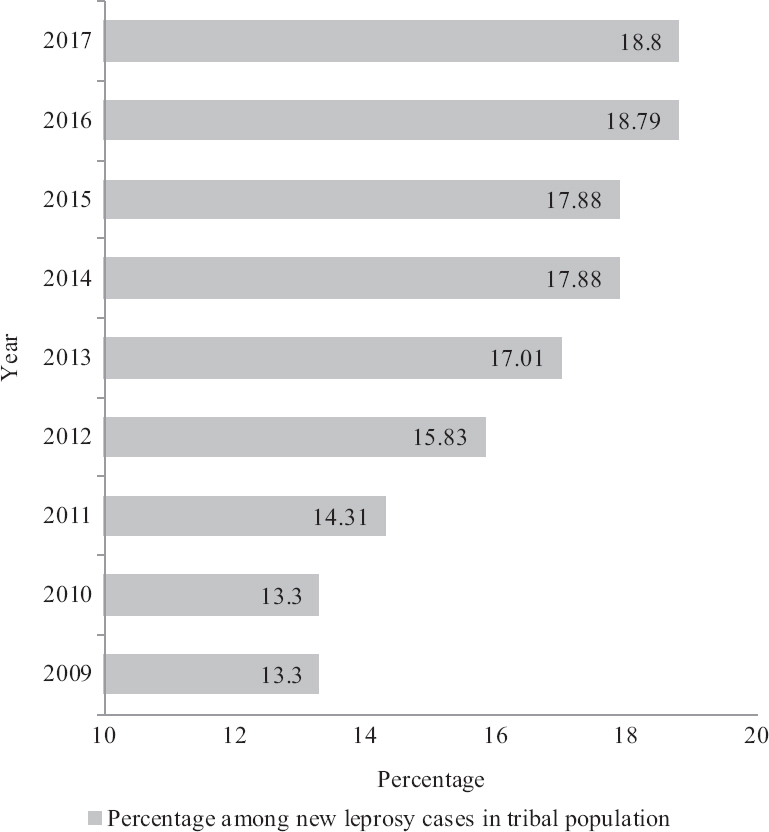
- Proportion of STs among new leprosy cases in India until 2017. An increasing trend has been shown. Data beyond 2017 are not yet available (Source: ORF report 201940). ST, scheduled tribe
State-level data present an even more dismal picture. For example, in 2017, ‘three out of every four new leprosy patients belonged to either SC or ST community in Tripura while their combined share in the population is around 50 per cent. In Gujarat, two out of every three new leprosy patients belonged to either Adivasi or Dalit communities, and in States such as Odisha, Madhya Pradesh, Maharashtra, West Bengal and Jharkhand, every second new case of leprosy belonged to these communities’40. These figures are disproportionately higher than the percentage share of the SC as well as ST population put together in these States (Fig. 2). Given that the proportion of multibacillary (MB) leprosy cases is high in some of these States, in addition to the tough terrain and remote locations in some areas of these States may further contribute to the ongoing transmission22.
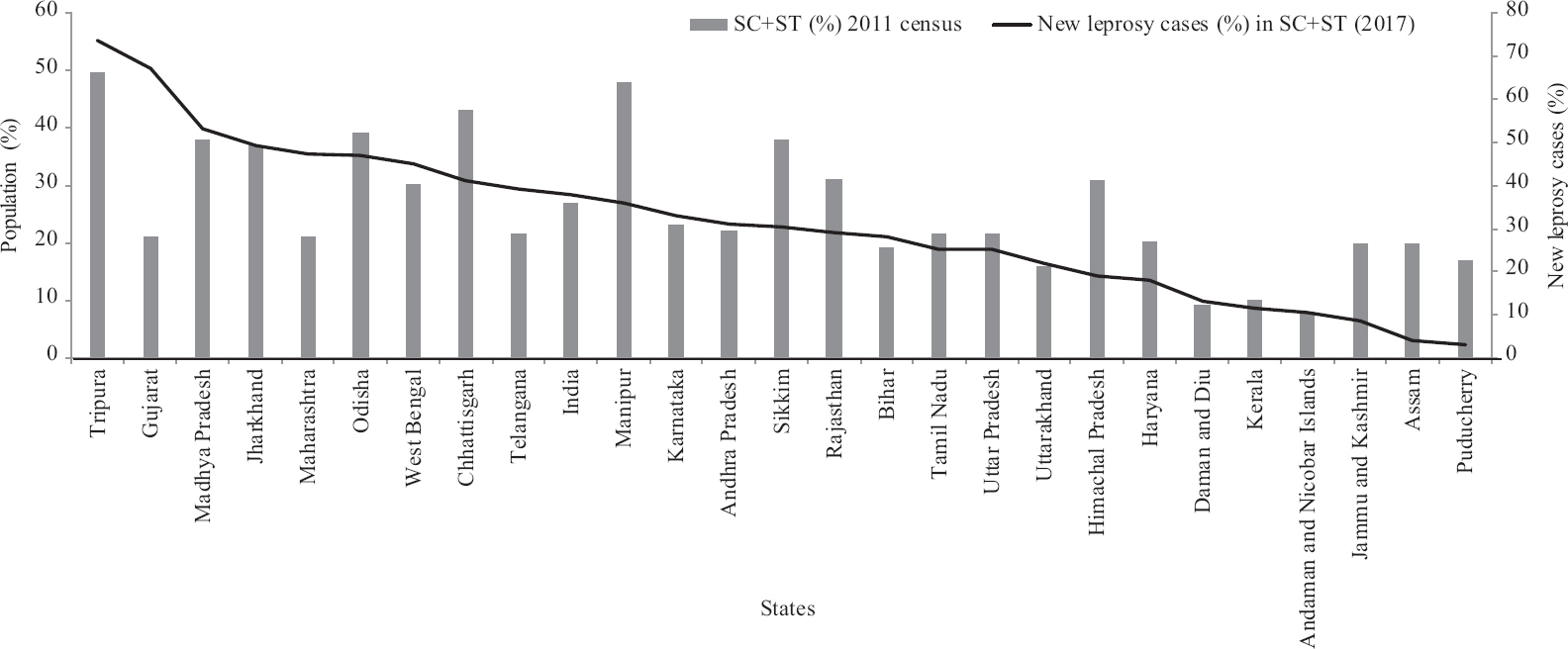
- State-wise proportion of SCs and STs and burden of new leprosy cases among SCs and STs in 2017 (Source: ORF report 201940). ST, scheduled tribe; SC, schedule caste
STs make up just 14.8 per cent of the total population of Gujarat, whereas around 64.8 per cent of all new leprosy cases were identified among them in the year 2016-201740,41. Likewise, with a 21 per cent share of the total population of Madhya Pradesh, the STs account for 39.4 per cent of the new leprosy cases detected in the State. STs in Maharashtra exhibit 33.7 per cent of all new leprosy cases despite having a <10 per cent share in the total population of the State. West Bengal reported 20.3 per cent of all new leprosy cases among STs whereas these make up only 5.8 per cent of the State population. Tripura State and Dadra and Nagar Haveli UT (with 31.8 and 52% share of STs in the total population of the State/UT), report 64.7 and 98.2 per cent of the new leprosy cases among STs, respectively (NLEP)40. The disproportionately high burden of leprosy in STs is evident from the above data for at least certain States42. The State-wise leprosy data from Figure 3 highlight those States where ANCDR is >10/100,000 (shown by red dots)43. These five States (Bihar, Chhattisgarh, Madhya Pradesh, Odisha and Telangana) and two UTs (Dadra and Nagar Haveli, Daman and Diu) have a relatively high percentage of ST and SC population. Around 31 per cent of the total population of India lives in the above-mentioned States. Strikingly, the percentage of the ST population living in these States/UTs is around 42 per cent of the total population of the tribals in India (Census 2011)39.
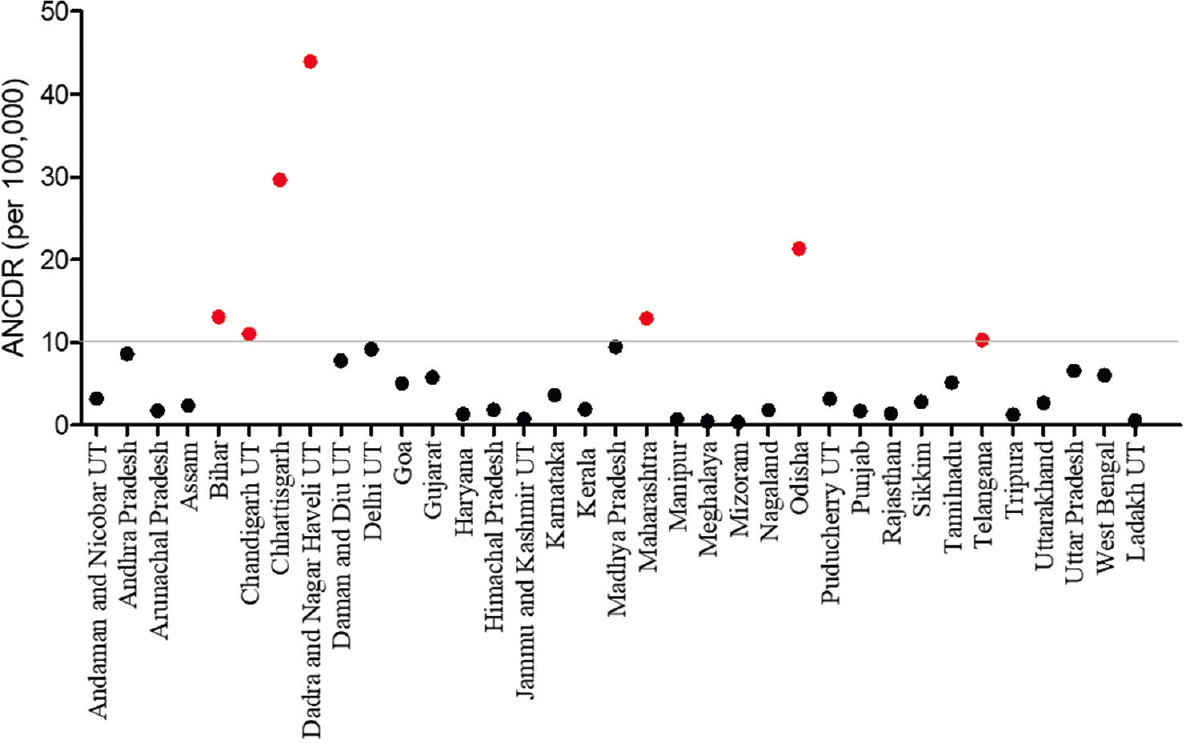
- Annual New Case Detection Rate (ANCDR) in 2019-2020, states and union territories of India (ANCDR >10 are shown in Red) (Source: NLEP, 202043). ANCDR, annual new case detection rate
Meanwhile, as leprosy treatment is integrated with the General Health Services, mere identification of the leprosy cases is not easy in the settings where they remain as endemic reservoirs unless greater efforts are made to reach them. For example, the Government of India (GoI) figures from the Tapi district in Gujarat (with a tribal population of more than 80 per cent) suggest that the incidence of leprosy has risen from 9.37 per 10,000 populations in 2010 to 17.16 per 10,000 in 201440,44. However, Tapi has now achieved the elimination goal as of March 2020 (https://nhm.gujarat.gov.in/nlep1.html). On the contrary, the incidence has gone up in several tribal belts between 2010 and 2017. The reason for the high prevalence of the disease in such areas could be their remote location where access to healthcare facilities and awareness is limited, leading to long diagnostic delays from the time of onset of symptoms which leads to continued transmission.
Indeed, a recent report from Raipur district (where 27% population is represented by STs) in Chhattisgarh State has shown that nearly 40 per cent of individuals did not take any action after noticing the symptoms, and nearly all the individuals (98% of the leprosy patients diagnosed between April 2017 and March 2019), attributed ‘ignorance about the symptoms of leprosy as the cause of their delay in seeking proper diagnosis and treatment45. Prevalence rates of childhood leprosy are also high, with a range from four to 34 per cent in certain pockets of the country, and are considered a surrogate marker of the recent transmission of leprosy46,47. Children rely on their parents to take them to hospitals for diagnosis and treatment, but several characteristics lead to the delayed start of the treatment. Many parents believed that the disease would go by itself, which is a serious concern as such delays often lead to excessive bacterial load and deformities in patients48. In some cases, access to a medical centre with proper diagnosis and treatment is also limited, which results in a prolonged delay49. These data also highlight the poor access to the healthcare system by STs, which could be the main reason that the expected level of leprosy control has remained elusive despite much-recognized achievements in other communities of the society.
Drug resistance
Recently rising trends in drug resistance have become evident in leprosy cases50. A survey by the World Health Organization showed that eight per cent of the samples examined in India exhibited DNA mutations associated with resistance to the anti-leprosy drug rifampicin51. Researchers have employed various molecular epidemiology tools to understand the nature of primary and secondary drug resistance in various populations worldwide52,53. Even though tribal communities have a high prevalence of leprosy, such surveillance initiatives have not been recorded. Tribal people often migrate for short durations to neighbouring districts and States to work in fields, for example, at the time of crop harvest. This compromises their treatment compliance, thereby leading to the emergence of drug resistance and can also contribute to the transmission of mycobacterial pathogens to other health members in the household or other communities. Therefore, certain innovative efforts must be made to control leprosy among tribal populations since controlling infectious diseases in these populations has broader health advantages for non-tribal societies as well. For example, with a rising proportion of MB leprosy cases in the population, there is an urgent need to evaluate the ongoing ‘fixed duration treatment’ guidelines for MB leprosy22. The management of such MB cases in tribal population/those living in remote areas should involve additional measures such as field-applicable point-of-care tests for screening of biomarkers of leprosy bacilli in the lesions. A microscopic examination to determine the bacillary index and provision of patient follow up at six-month intervals can also be useful.
Surveillance: Inadequate compliance to treatment is a major issue with tribal populations as they undertake short-term migration making them prone to leave their treatment incomplete, thereby increasing the chances of emergence of drug resistance. Regular monitoring of the cases released from treatment and relapse cases is also needed to further reduce leprosy burden12, 21,45,54,55.
Although, a national sample survey of leprosy was conducted by the Indian Council of Medical Research (ICMR), and other partners in 2017, only big cities in the urban clusters were covered56. The evaluation and the comparison of the leprosy cases in the tribal population vis-a-vis general population could not be assessed and this was a major limitation of the study. Only one study carried out in 2017 has so for identified the regions of actual hotspots of leprosy within Maharashtra State by dividing the new cases into several categories such as child, female and MB and G2D cases found within the high prevalence areas such as Vidarbha region. By comparing the prevalence to non-tribal hotspot data, the study concluded that ‘even a single new case with G2D/new child/female cases should be treated as evidence of hidden endemicity in the tribal belt’21. MDT has proven to be an effective tool for treating leprosy, particularly when patients are detected timely and treatment compliance is good57. When it is not, the leprosy-affected patients can develop disability.
To visualize the distribution of leprosy situations across the country of past 10 years, a district-level report was prepared by NLEP comprising annual new cases detected, ANCDR, G2D rate and prevalence rate. The geometric mean for the 10 yr duration (2008-2009 and 2018-2019) has been considered to reflect the leprosy situation in India. Weightage was applied to each parameter according to the endemicity, such as 40 per cent weightage to the number of new leprosy cases, 20 per cent to registered prevalence, 20 per cent to the number of child cases and G2D, respectively. After the weightage, the districts were categorized into high endemic, moderately endemic, low endemic and sporadic cases. These data were compared with the population data of India, which revealed that where the tribal population is more than 10 per cent of the total population (Fig. 4). In addition, the prevalence of leprosy in 12 States (Chandigarh, Delhi, Uttar Pradesh, Chhattisgarh, Dadra and Nagar Haveli, Maharashtra, Madhya Pradesh, Jharkhand, West Bengal, Odisha, Andhra Pradesh and Telangana) is also high. Specifically, there were 324 districts in India classified as high and moderate endemic districts, of which 241 are in the above mentioned 12 States and UTs. The data clearly suggest that numerous government and non-governmental groups should emphasize towards the challenges to deal with the issues of tribal health.
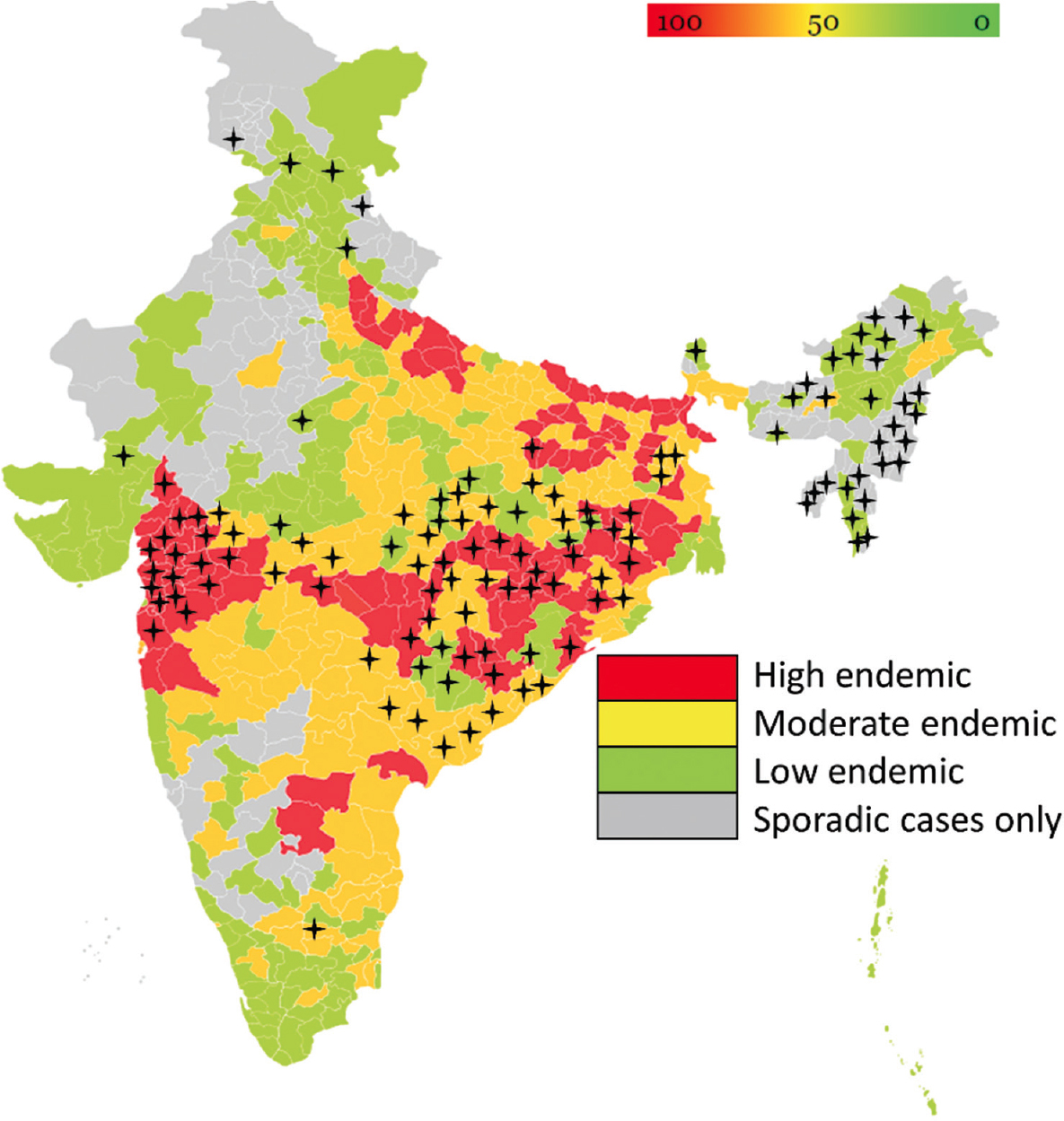
- Comparison of leprosy endemicity between tribal districts vs. non-tribal districts in India from 2008-2018 (NLEP 2019). ‘+’ denotes the tribal district. The map was constructed using gramener (https://gramener.com/indiamap/). NLEP, National Leprosy Eradication Programme
Strategy for leprosy elimination in tribal areas
The integration of NLEP with other health programmes was aimed at improving case detection and treatment access; however, special efforts are required to eliminate leprosy in many tribal areas. There is often a time gap in the project preparation, execution and reporting stages. The planned timeframe for completing all these tasks is often not achieved.
Some of the underlying reasons for this situation are stated below:
Involvement of local people in the implementation of Government schemes: Tribal people are often shy. Their first preference is to go to a traditional tribal healer (Gunia). Therefore, training the tribal healers about leprosy symptoms can be an effective approach. These trained tribal healers can be given referral incentives like those given to Accredited Social Health Activist (ASHA) workers for assisting in the identification of new cases, their registration and treatment compliance58. The Special Activity Plan and Leprosy Case Detection Campaign generated by Gujarat (https://nhm.gujarat.gov.in/nlep1.htm) can serve as a model for other States as well to achieve goals set by NLEP. The NLEP aims to eradicate leprosy in each district by 203059. For these programmes, such as ‘Active Case Detection and Regular Surveillance’ in both rural and urban regions, should be implemented to ensure regular and early detection of leprosy cases. In addition, these health assistants should be trained about the occurrence of leprosy reactions and where to refer the patients so that such presentations can be managed effectively, and the treatment compliance is not compromised.
Guaranteeing service delivery: The fact that households are often scattered and inaccessible means that service delivery is often difficult, even with improvements in the supply chain system60. However, storage of drugs and distributing MDT can also be structured where drugs are given to patients for a longer period and are assisted by a trustworthy local individual, such as a village volunteer or representative. The health centres of the government, private sector, and NGOs should develop or extend the existing drug distribution points along with telephone service in case of any emergency. In addition, a trustworthy volunteer/local person who previously treated cases taught of symptoms of leprosy, such as signs of reaction and deterioration. For these volunteers also, there should be incentivization for successful referrals and case detection.
Spreading awareness among the communities: The main reason for hidden endemicity is a lack of voluntary reporting by the community because of continuing stigma and prejudice towards people affected by leprosy. Through communicating the need for early identification and treatment of leprosy, the SPARSH leprosy awareness campaign61 launched by the GoI made an impact that helps to eliminate this stigma and prejudice by increasing the awareness level about leprosy and detecting a greater number of new cases to provide early treatment. Various camps are organized to identify and treat people with skin diseases, including leprosy and those at a risk of developing disability. These camps have served as valuable places for raising awareness by engaging the community. In addition, the inclusion of the previously cured cases of leprosy as ‘the agents of change’ or as ‘Leprosy Champions’ (similar to the concept of ‘TB champions’) can address the concerns around social stigma against leprosy. Regional language(s) can be used for general communication with a community. The best way to cross language barriers is to get the full participation of local patrons.
Availability of trained staff at primary health care (PHC) centre
With over 150,000 health and wellness centres being created in India as part of the Ayushman Bharat plan, it is an opportunity to locate, detect and provide treatment to individuals who were previously not covered by the NLEP62. Slit-skin smear microscopy remains the only laboratory test mandated by the Ministry of Health and offered by the Public Health network63. It is a rapid and low-cost test that has high accuracy in categorizing the clinical form of the disease and hence aids in establishing the treatment plan. It seems like slit skin smear examination is a forgotten technique and probably not paid enough attention at the PHC levels. Hence, such cases which could be diagnosed even by simple microscopy can remain undetected for a long time. Most of the programmes work on the first two cardinal features of leprosy: (i) skin lesions, (ii) nerve thickening with the sensory deficit with or without motor function impairment, and the third one, i.e. (iii) the detection of AFB in slit skin smear, has not been paid due attention. The construction of an active and well-designed care network in tribal areas with well-defined local and regional reference services, with the experience of basic and simple laboratory tests for a more accurate diagnosis and effective case follow up, would help to consolidate the efforts to further control leprosy in these regions.
The current tribal area leprosy elimination strategy was built based on the experiences of NLEP and NGOs, as well as some pilot projects undertaken in a few Indian tribal regions. It would be necessary to further refine this strategy to suit the special needs of tribal populations in other parts of the country for those living in remote areas. Door-step delivery of diagnosis and treatment should be implemented in remote areas and marginalized populations. In addition, the experiences of the person involved in supply chain related to health services at the village level (such as ASHA workers, etc.) should be availed. Other data, such as sociodemographic details and information about various population groups (ST/SCs, etc.) should be documented and made available for policymakers so as to enable targeted and more effective implementation of leprosy control activities. While documentation may be a useful tool in the longer term, an ongoing, sustainable mechanism for monitoring the local leprosy situation must also be established that integrates all the documents in a single system or website, based on which local stakeholders can decide on renewed leprosy elimination activities.
Overall, the rate of decline in leprosy is much slower among tribal communities compared to non-tribal communities. Leprosy eradication attempts by 2030 would be a difficult task without paying special attention to the high-risk pockets of tribal areas. The tribal belt should be the focus of the NLEP for the effective management and efficient control of the disease through health education and communication campaign; early detection and management of cases; ensuring treatment adherence using ASHA workers and traditional healers, and possibly through direct observation of treatment; and through the provision of uninterrupted supply of treatment and MDT delivery at patient doorstep. Many of these could even potentially become the subjects for implementation research by NLEP, ICMR and partners. To reach the zero-leprosy goal, it is essential to address the leprosy situation among tribal people promptly and adequately by expanding the scope of tribal health through scientific research and development methodologies tailored to match the needs of tribal people.
Financial support & sponsorship: None.
Conflicts of Interest: None.
References
- Mycobacterium lepromatosis as a second agent of Hansen's disease. Front Microbiol. 2021;12:698588.
- [Google Scholar]
- Disabilities in leprosy:An open, retrospective analyses of institutional records. An Bras Dermatol. 2020;95:52-6.
- [Google Scholar]
- Leprosy. StatPearls, Treasure Island (FL): StatPearls Publishing Copyright©2021, StatPearls Publishing LLC; 2021.
- Current knowledge on Mycobacterium leprae transmission: A systematic literature review. Lepr Rev. 2015;86:142-55.
- [Google Scholar]
- Unsolved matters in leprosy: A descriptive review and call for further research. Ann Clin Microbiol Antimicrob. 2016;15:33.
- [Google Scholar]
- Reservoirs and transmission routes of leprosy;A systematic review. PLoS Negl Trop Dis. 2020;14:e0008276.
- [Google Scholar]
- Leprosy: An overview of pathophysiology. Interdiscip Perspect Infect Dis. 2012;2012:181089.
- [Google Scholar]
- Global elimination of leprosy by 2020:Are we on track? Parasit Vectors. 2015;8:548.
- [Google Scholar]
- Weekly epidemiological record. 2021;96:421-44.
- Socioeconomic risk markers of leprosy in high-burden countries:A systematic review and meta-analysis. PLoS Negl Trop Dis. 2018;12:e0006622.
- [Google Scholar]
- Comorbidities in patients with Hansen's disease. In: Scollard DM, Gillis TP, eds. The International Textbook of Leprosy. USA: American Leprosy Missions; 2016.
- [Google Scholar]
- Dietary diversity and poverty as risk factors for leprosy in Indonesia:A case-control study. PLoS Negl Trop Dis. 2018;12:e0006317.
- [Google Scholar]
- Socio-cultural features and help-seeking preferences for leprosy and turbeculosis:A cultural epidemiological study in a tribal district of Maharashtra, India. Infect Dis Poverty. 2015;4:33.
- [Google Scholar]
- Prevalence and determinants of undernutrition and its trends among pre-school tribal children of Maharashtra State, India. J Trop Pediatr. 2012;58:125-32.
- [Google Scholar]
- The stigmatization of leprosy in India and its impact on future approaches to elimination and control. PLoS Negl Trop Dis. 2008;2:e113.
- [Google Scholar]
- Leprosy perceptions and knowledge in endemic districts in India and Indonesia:Differences and commonalities. PLoS Negl Trop Dis. 2021;15:e0009031.
- [Google Scholar]
- Towards elimination of stigma &untouchability:A case for leprosy. Indian J Med Res. 2019;149:S81-7.
- [Google Scholar]
- Epidemiological perspective of National Leprosy Eradication Programme in Maharashtra:Focusing on “Tribal Hot-spot”of Tribal District. Indian J Community Med. 2017;42:174-6.
- [Google Scholar]
- Current situation of leprosy in India and its future implications. Indian Dermatol Online J. 2018;9:83-9.
- [Google Scholar]
- Molecular characterization of environmental mycobacterial species from leprosy endemic tribal regions of North Purulia District, West Bengal. Int J Mycobacteriol. 2019;8:381-9.
- [Google Scholar]
- Hidden leprosy cases in tribal population groups and how to reach them through a collaborative effort. Lepr Rev. 2015;86:328-34.
- [Google Scholar]
- Epidemiological survey of neurological diseases in a tribal population Cluster in Gujarat. Ann Indian Acad Neurol. 2018;21:294-9.
- [Google Scholar]
- Leprosy in post-elimination era in India:difficult journey ahead. Indian J Dermatol. 2013;58:443-6.
- [Google Scholar]
- World Leprosy Day, 2015:Renewing commitment for a leprosy free world. Indian J Med Res. 2015;141:1-4.
- [Google Scholar]
- Prevalence and risk factors for grade 2 disability among newly diagnosed leprosy in children and adolescents:A record-based analysis from India. Lepr Rev. 2022;93:79-88.
- [Google Scholar]
- Leprosy on the rise in India:Need to adopt enhanced strategy for its control. Primary Health Care. 2014;4:e109.
- [Google Scholar]
- Literacy and health status of scheduled castes in India. Contemp Voice Dalit. 2020;12:97-110.
- [Google Scholar]
- Distribution of Schedule Tribes health configuration in India:A case study. Sci Technol Dev J (IT Publ). 2020;9:181-203.
- [Google Scholar]
- Tribal population in India:A public health challenge and road to future. J Family Med Prim Care. 2020;9:508-12.
- [Google Scholar]
- Leprosy among tribal population of Chhattisgarh state, India. Indian J Lepr. 2011;83:23-9.
- [Google Scholar]
- Genomic epidemiology reveals multiple introductions and spread of SARS-CoV-2 in the Indian state of Karnataka. PLoS One. 2020;15:e0243412.
- [Google Scholar]
- Ministry of Health and Family Welfare and Ministry of Tribal Affairs, Government of India. Tribal Health in India: Bridging the gap and a roadmap for the future: Executive summary and recommendations. Available from: https://nhm.gov.in/nhm_components/tribal_report/Executive_Summary.pdf
- Census Digital Library. Office of the Registrar General & Census Commissioner India. Ministry of Home Affairs, Government of India. Provisional population totals. New Delhi: MoHA, GoI; 2011. p. :409-13.
- Observer Research Foundation. Leprosy and inequities in India's healthcare: Beyond the persistent rhetoric of ‘Elimination‘. New Delhi: ORF; 2019.
- The Indian Express. Scheduled Tribes most affected by leprosy in Gujarat. Avaialble from: https://indianexpress.com/article/lifestyle/health/scheduled-tribes-most-affected-by-leprosy-in-gujarat-5598457/
- Current situation of leprosy in tribal areas of India in the post-elimination era. Indian J Dermatol Venereol Leprol. 2022;88:450-1.
- [Google Scholar]
- Central Leprosy Division. Directorate General of Health Services, Ministry of Health & Family Welfare, Government of India. NLEP annual report: 2019-2020. New Delhi: MoHFW, GoI; 2020.
- 2019. India Hosts 66% of Leprosy Patients, Shows WHO Data: Mint. Available from: https://www.livemint.com/science/health/was-india-ever-free-from-leprosy -1566443030568.html
- Clinico-epidemiological pattern of determinants of visible disabilities among patients affected with leprosy in Raipur district, Chhattisgarh. Int J Community Med Public Health. 2020;7:1565-70.
- [Google Scholar]
- Leprosy in elderly and children among new cases - A 3-year retrospective study. Indian Dermatol Online J. 2021;12:294-7.
- [Google Scholar]
- Leprosy among children under 15 years of age:Literature review. An Bras Dermatol. 2016;91:196-203.
- [Google Scholar]
- Risk of disability among adult leprosy cases and determinants of delay in diagnosis in five states of India:A case-control study. PLoS Negl Trop Dis. 2019;13:e0007495.
- [Google Scholar]
- Characteristics of children with leprosy:Factors associated with delay in disease diagnosis. Indian J Dermatol Venereol Leprol. 2022;88:337-41.
- [Google Scholar]
- Equal rates of drug resistance in leprosy cases with relapse and recurrent/chronic Type 2 reaction:Time to revise the guidelines for drug-resistance testing in leprosy? Clin Exp Dermatol. 2022;47:297-302.
- [Google Scholar]
- Antimicrobial resistance in leprosy:Results of the first prospective open survey conducted by a WHO surveillance network for the period 2009-15. Clin Microbiol Infect. 2018;24:1305-10.
- [Google Scholar]
- Simultaneous determination of Mycobacterium leprae drug resistance and single-nucleotide polymorphism genotype by use of nested multiplex PCR with amplicon sequencing. J Clin Microbiol. 2021;59:e0081421.
- [Google Scholar]
- Molecular epidemiology and transmission dynamics of leprosy among multicase families and case-contact pairs. Int J Infect Dis. 2020;96:172-9.
- [Google Scholar]
- The role of an active surveillance strategy of targeting household and neighborhood contacts related to leprosy cases released from treatment in a low-endemic area of China. PLoS Negl Trop Dis. 2020;14:e0008563.
- [Google Scholar]
- National sample survey to assess the new case disease burden of leprosy in India. Indian J Med Res. 2017;146:585-605.
- [Google Scholar]
- Multidrug therapy for leprosy:a game changer on the path to elimination. Lancet Infect Dis. 2017;17:e293-7.
- [Google Scholar]
- Connecting the unconnected:the way forward for public health to reach the unreached tribal communities in India. Current Science. 2021;120:24.
- [Google Scholar]
- Ministry of Health and Family Welfare, Government of India. Progress achieved in National Leprosy Eradication Programme. Delhi: MoHFW, GoI; 2021.
- A qualitative study of the barriers to utilizing healthcare services among the tribal population in Assam. PloS One. 2020;15:e0240096.
- [Google Scholar]
- Accelerating towards a Leprosy Free India through innovative approaches in the National Leprosy Eradication Programme (NLEP), India. Lepr Rev. 2020;91:145-54.
- [Google Scholar]
- Health system readiness for roll out of the Ayushman Bharat Health and Wellnes Centres –Early experiences from Punjab State. J Family Med Primary Care. 2022;11:1354-60.
- [Google Scholar]






