Translate this page into:
Post-thyroidectomy hypoparathyroidism: A rare cause of extensive brain parenchymal calcification
*For correspondence: bhadadask@rediffmail.com
-
Received: ,
This article was originally published by Wolters Kluwer - Medknow and was migrated to Scientific Scholar after the change of Publisher.
A 24 yr old female† presented in Endocrinology outpatient department, Postgraduate Institute of Medical Education & Research, Chandigarh, India, in April 2019, with anasarca and sluggishness. At nine years of age, she underwent total thyroidectomy with radical neck dissection for papillary thyroid carcinoma. Her serum albumin was 2.4 g/dl, corrected calcium was 4.4 mg/dl [reference range (RR) 8.2-10.4 mg/dl], serum phosphate was 9.8 mg/dl (RR 2.5-4.5 mg/dl), intact parathyroid hormone was 1.5 pg/ml (RR 15-68 pg/ml), 25(OH)D was 2.5 ng/ml and thyroid-stimulating hormone was 27 uIU/ml (RR 0.5-4.2), T4 was 2.6 mcg/dl (RR 4.22-12.8) and T3 was 0.57 ng/ml (RR 0.8-2.0). Contrast-enhanced computed tomography scan of the brain showed bilaterally symmetrical calcification of brain parenchyma involving basal ganglia, thalamus, subcortical white matter of bilateral frontoparietal lobe and bilateral cerebellar hemisphere calcification (Figs 1 and 2). Electroencephalography showed generalized increase in theta wave activity, suggestive of diffuse encephalopathy. DiGeorge syndrome was ruled out using the MLPA (Multiplex Ligation-Dependent Probe Amplification) method. She was discharged with oral calcium carbonate 2500 mg/day and 1,25 hydroxyvitamin D1 µg/day. She improved clinically and biochemically and was regularly followed up from 18 months as outpatients through teleconsultation requiring 500 mg of calcium carbonate and 0.25 µg/day.
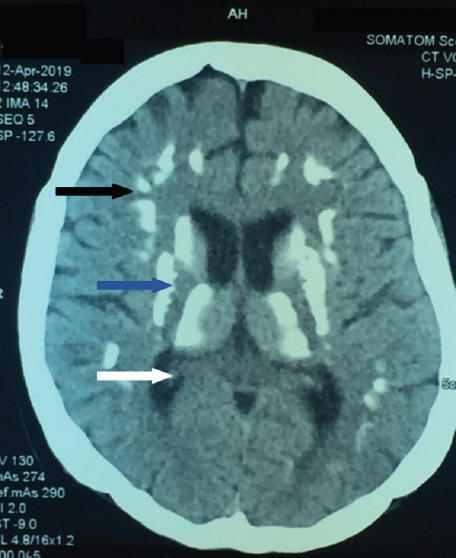
- Non-contrast CT of brain with diffuse brain parenchymal (black arrow), basal ganglia (blue arrow) and thalamic calcification (white arrow).
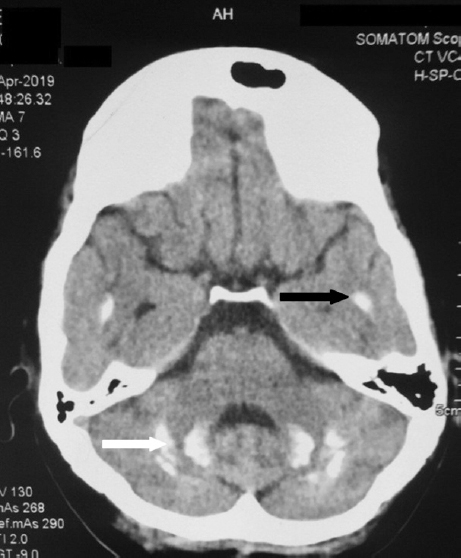
- Non-contrast CT of brain with diffuse cerebellar (white arrow), temporal lobe calcifications (black arrow).
The generalized calcification of the brain parenchyma is rare in post-surgical hypoparathyroidism patients as it depends on the duration of poorly corrected serum calcium levels. Patients of post-surgical chronic hypoparathyroidism should be evaluated for brain parenchymal calcification, if they present with abnormal body movement as it may be caused by increased calcium phosphate product, altered calcium phosphate ratio and duration of hypocalcaemia.





