Translate this page into:
Cost of providing family planning services & management of pregnancy outcomes at public health facilities in India
For correspondence: Dr Beena Joshi, ICMR-National Institute for Research in Reproductive and Child Health, Jahangir Merwanji Street, Parel, Mumbai 400 012, Maharashtra, India e-mail: joshib@nirrch.res.in
-
Received: ,
This article was originally published by Wolters Kluwer - Medknow and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Background & objectives:
Lack of costing data is a critical gap that exists in the field of family planning (FP) in India. The aim of this study was to estimate health system costs of FP in India for existing modern methods, and potential newer methods (etonorgestrel implant and levonorgestrel intrauterine device) and pregnancy-related services in India.
Methods:
A bottom-up micro-costing study was conducted in five public health facilities of an Indian State. Data of last one year were collected from existing hospital records and hospital staff was interviewed. Collected data were analyzed using standard costing methods.
Results:
Package costs of delivering FP services ranged from ₹ 807 (95% CI 685, 931) for condoms and ₹ 10,539 (8796, 12269) for tubal ligation. Estimates of etonorgestrel implant and levonorgestrel intrauterine system were ₹ 3,200 (2800, 3625) and 3,426 (3232, 3623). Cost of antenatal care along with vaginal delivery, caesarean and abortion were ₹ 10,916 (8744, 13078), 22,136 (17570, 26910) and 8,574 (6791, 10379), respectively. One way sensitivity analysis showed that the three most influential factors on the costs of FP services were prices of drugs and consumables, number of beneficiaries and health personnel cost.
Interpretation & conclusions:
The present study has generated package costs for FP and pregnancy-related services in India which could be used by publicly-funded insurance schemes, for budgeting, economic evaluations and improve resource allocation of services. The cost estimates from this study add to the limited literature in India on costs of FP.
Keywords
Contraception
family planning
India
micro-costing
pregnancy
public health services
Family planning (FP) allows individuals and couples to plan and attain the desired number of children using various contraceptives1. India has witnessed a progressive change in its approach to FP. Through its flagship programme, National Health Mission (NHM), India, now provides various spacing and permanent methods of contraception2. These services are not charged to the user; nevertheless, the government incurs costs on providing them to eligible and willing couples.
FP services are provided across all levels of public health care in India. The National Family Health Survey-4 (2015-2016) shows that 69 per cent of the country’s modern contraceptive services are availed from the public health sector3. The NHM budgetary allocation to FP in the year 2016-2017 was 2.7 per cent4. In the financial year 2016-2017, only 60.7 per cent of the total budget available for FP activities was spent5. A critical gap that exists in FP policy, planning and programme expansion is a lack of costing data that could be accessible to policy analysts, country officials and implementing organizations. Such a database is available online for a few developing countries (excluding India), but is more than two decades old6. A few studies done in India reported the unit costs of insertion of intrauterine contraceptive device and conducting a vaginal delivery. There are some studies on out-of-pocket expenditure from the patients’ perspective, but very few studies from the health system perspectivexy78. Apart from these, costs of FP service data in India are limitedxy910.
According to a report by a World Health Organization Health financing committee, costs of health services could be used for budgeting, economic evaluation studies, or to compare the efficiency of different settings. Determining cost estimates are vital for health facilities, systems and countries, to inform health finance management and health policy decisions11. There are a few studies done in the past decade, in developing countries that report unit cost of providing hospital services121314. There is limited cost data specifically on FP services.
This paper is part of a larger study on Health Technology Assessment (HTA) conducted to facilitate making a policy decision on introducing newer long-acting reversible methods into the national health programme in India. If any contraceptive method fails, it results in unintended pregnancy which in turn can result in either abortion, ectopic pregnancy, vaginal or caesarean section. Thus, costing exercise was undertaken for contraceptive service delivery as well as management of side effects and its failure.
Material & Methods
A cross-sectional study with a bottom-up micro-costing approach was used to estimate the current costs of providing FP methods such as copper intrauterine device (IUD), oral contraceptive pills (OCP), depot medroxyprogesterone acetate (DMPA) injectables and female sterilization; potential newer contraceptives such as levonorgestrel intrauterine system, etonorgestrel implants and pregnancy-related services at the public health facilities in Maharashtra State. The health system’s perspective was used for the costing study. The study was conducted during April-October 2018 by the HTA Resource Hub, ICMR-National Institute for Research in Reproductive and Child Health (NIRRCH), after approval by the Institutional Ethics Committee of Clinical Studies. Written permissions were obtained from all relevant officials prior to conducting the study. The operational definitions used in this study are mentioned in the Box.
| Health facility: A public health facility as defined by the Indian Public Health Standards (IPHS) |
| Health facility cost: Cost to the government to provide a service at a public health facility |
| Programme cost: Cost to the government to run a public health programme including the activities pertaining to Information-Education-Communication (IEC), training and incentives given to providers and beneficiaries |
| Health system costs: A sum of health facility and programme costs |
| Unit cost of a service: Cost of providing a specified service for one woman for one event |
| Package costs: Overall costs of providing either a contraceptive method or a pregnancy-related service to one woman for one year (including outpatient visits, inpatient days, operation procedure costs, etc.). |
| The above terminologies have been adapted from HTA reference manual15. |
Study setting: The study was undertaken in five public health facilities, based on purposive sampling, representing the three levels of healthcare in India. A 2844-bedded tertiary care hospital in Mumbai, a 336-bedded district hospital (DH) in Thane, a 100-bedded sub-DH (SDH), a 30-bedded primary health centre (PHC) and a one-bedded sub-centre (SC) from a district in the State of Maharashtra, India, were selected for the study. The SDH was located about 120 Km from Mumbai, the capital city of the State of Maharashtra.
In accordance with the IPHS, the SDH, DH and tertiary care hospital had specialists in obstetrics and gynaecology. In PHC, there were MBBS/BAMS doctors. At the primary care level, the service providers were the auxiliary nurse midwives, lady health visitors, staff nurses and doctors. Spacing methods like intrauterine copper devices were provided from the SC level and above. Condoms, OCP and emergency contraceptive pills were provided at the village level through SC and accredited social health activists (ASHA) who provide doorstep delivery of these contraceptives. Limiting/permanent methods like tubectomy and non-scalpel vasectomy were provided from PHC level and above. Caesarean sections were done at SDH level and above2.
Data collection: Costs for resources utilized at these centres, for FP and pregnancy-related services, such as human resources (HR), infrastructure, capital and overheads, medical and non-medical equipment, drugs and consumables and utilities such as electricity, water, transport, diet and laundry were collected. Costs from floor area, spaces within the public health facilities such as outpatient department (OPD), inpatient ward (IPD), labour room, laboratory, radiology, operation theatre (OT), pharmacy and administration were collected. Tools of a larger ongoing costing study funded by the Department of Health Research, Government of India, were adapted and used for data collection.
Data sources: Data for the study were collected for the financial year 2017-2018 and sources of data included written hospital registers and electronic hospital records, health management information system; building plans of the health facility, statements from accounts departments (for salary slips, bills, etc.), excel sheets of indent and supply from pharmacy and store departments, staff interviews, observations and measurements. Each health centre maintains a record of its activities in one or more of the primary registers online as per government health management and information system16. This system was used to get information on the number of patients who received various services such as OPD consultations, IPD, vaginal and caesarean deliveries, abortions, sterilizations, contraceptive provision and related statistics in the financial year 2017-2018. Staff interviews were used to assess the time spent by the staff doing different activities. Activities were classified as routine/fixed and their frequency was noted. Time spent on each patient in OPD, IPD, time taken to do a surgery was asked, by the senior-most specialist/doctor during their work hours. Nurses, laboratory technicians and radiology staff were interviewed for their time distribution at the workplace. In the laboratory, the time taken to do a separate group of tests such as haematological, biochemical, serological and immunological tests were collected. The health facility area was measured, medical and non-medical equipment along with details of year of purchase, cost at the time of purchase, and time it was used was obtained. Expenditure on IEC material and activities, training, incentives to ASHA, beneficiaries and providers for the whole State, pertaining to FP and pregnancy-related services was obtained from the Maharashtra State Government for the financial year of 2017-2018.
Data analysis: Data analysis was done to derive the health facility cost and programme cost separately. This was then combined to report health system costs. The following steps were undertaken:
Step 1: Calculating unit costs for services in each of the health facilities: For each health facility a unit cost per day was derived for the following categories in Obstetrics and Gynaecology department (OBGYN): OPD consultation, IPD per bed-day, OT per procedure and institutional delivery. This was done by summing up the components of HR salaries, equipment costs, costs of drugs in that category, overheads and utilities that were required for the OBGYN department. This sum was divided by the number of beneficiaries for OPD, IPD and OT, respectively.
It was ensured that the contraceptive, ANC and delivery services were separated from the other services provided by the health facilities by using appropriate apportioning factors. Data were collected from all the points inside the health facilities where contraceptive, ANC and delivery care were provisioned. Any resource that was used to provide more than one service was apportioned. For example, personnel, space or equipment that was being used for more than one activity was apportioned and the costs relevant to our objectives were obtained at each health facility.
For each of the facilities, annualization of equipment costs was done. Annualization factor was calculated using a discount factor of three per cent and the average life of the item as per the HTA India reference case15. A depreciation rate of 10 per cent was applied for medical equipment. Standardized methods were used to calculate unit costs10.
Step 2: Calculation of weighted average of unit costs to derive overall health facility costs: The unit costs of the OBGYN services (OPD, IPD, OT and labour room costs per service per day) at different levels of healthcare were combined by a weighted average method to arrive at a single unit cost for the overall OBGYN services in the public health facilities. The weights used were percentages of women seeking care for FP and pregnancy-related services at primary, secondary and tertiary public health facilities that were 21.7, 30.97 and 47.26 per cent, respectively17. For example, one OBGYN outpatient consultation at the PHC, SDH, DH and tertiary care hospital was combined using the aforementioned weights to derive the cost of one OBGYN OPD cost overall for the public health facilities.
Step 3: Calculation of package costs for family planning (FP) and pregnancy-related services: To calculate a package cost for each contraceptive method and pregnancy-related events (such as vaginal delivery, caesarean or, abortion and ectopic pregnancy), packages were designed and the health system unit costs were used as components of the package. These packages were designed by consulting specialists working in public health facilities and reviewing literature. Total OPD visits, IPD days and/or OT services for each of the different FP methods and pregnancy services were decided based on consensus with service providers and experts. Hence, the package costs included the cost of follow up care and treatment of side effects and complications of the methods.
Step 4: Calculation of health system costs: Programme costs such as unit cost of IEC, training and providing incentives (method-specific) to provider and beneficiary were added to the package costs to derive health system unit cost of services.
Step 5: Sensitivity analysis: One-way sensitivity analysis (OWSA) was done to assess which components of costs affected the unit cost of providing FP services. In OWSA, individual parameters were varied to account for uncertainty. The costs of drugs and consumables were varied by 100 per cent on the upper limit and 50 per cent on the lower side due to the large variations across the country. The salaries and other parameters were varied by 25 per cent9. Our sensitivity analysis varied in the number of beneficiaries, costs for drugs and consumables, laboratory investigations and infrastructure costs. The tornado diagram was generated to see which parameter affected the unit cost the most. Probabilistic sensitivity analysis was done, in which 1000 simulations were run, for each package cost to derive 1000 costs. A mean and SD cost was derived from these 1000 package costs which was then used to calculate 95 per cent confidence interval (CI) for each of the FP and pregnancy-related services.
Results
Characteristics of health facilities: The characteristics of the health facilities are presented in Table I. The facilities represented the three levels of healthcare that provide FP services. The beds in the facility were in line with IPHS. Staff providing FP services included OBGYN department staff at higher facilities like DH and tertiary care hospital.
| Characteristics | Sub-centre | Primary health centre | Sub-district hospital | District hospital | Tertiary care hospital |
|---|---|---|---|---|---|
| Number of beds | 1 | 30 | 100 | 336 | 2844 |
| Number of employees in the health facility | 3 | 22 | 65 | 446 | 3000 |
| Staff providing FP services | 2 | 10 | 35 | 61 | 105 |
| Annual facility outpatient consultations | 380 | 31,938 | 64,618 | 209,962 | 994,238 |
| Annual facility OBGYN outpatient | 68 | 11,624 | 5020 | 12,506 | 36,860 |
| Total annual inpatient admissions | 0 | 1258 | 5500 | 12,269 | 57,646 |
| Total OBGYN admissions | 0 | 494 | 1785 | 4784 | 11,897 |
| Total number of vaginal deliveries | 0 | 494 | 1526 | 2986 | 2202 |
| Total number of caesarean deliveries | 0 | 0 | 330 | 1045 | 1141 |
OBGYN, obstetrics and gynaecology; FP, family planning
Table I shows that about 35 per cent of the OPD in the PHC constitutes OBGYN consultations. This proportion ranged from about 3-10 per cent in SDH and higher level facilities. IPD admissions in OBGYN department were between 30 and 40 per cent of total admissions in PHC, SDH and DH. In the tertiary care hospital, this proportion was about 20 per cent. There were higher numbers of OBGYN OPD consultations in PHC (11,624) as compared to the SDH (5020).
The unit costs of services pertaining to FP and pregnancy in the health facilities are presented in Table II. Cost is presented in ₹ (Indian Rupee) and also converted to US $ (currency of the United States of America) at the conversion rate of one US $ = ₹ 7218.
| Health facilities at different levels | ₹ (US$) | |||
|---|---|---|---|---|
| Out-patient per-consultation | In-patient per-bed-day | Operation theatre per-procedure | Labour room per-delivery | |
| Primary health care centre | 72 (1) | 302 (4.2) | 2825 (39.2) | 1495 (20.7) |
| Sub-district hospital | 110 (1.5) | 720 (10) | 2464 (34.2) | 1738 (24.1) |
| District hospital | 244 (3.4) | 724 (10.1) | 2398 (33.3) | 2713 (37.7) |
| Tertiary care hospital | 446 (6.2) | 947 (13.2) | 4450 (61.8) | 4322 (60) |
Unit costs of services provided in the public health facilities showed a trend of being least in the PHC and highest in the tertiary care hospital. OT procedure costs are highest, as compared to OPD, IPD and labour room costs. OPD cost per consultation is ₹ 72, 110, 244 and 446, respectively at PHC, SDH, DH and tertiary care hospital, respectively.
The package cost of providing various contraceptive methods and pregnancy-related services; across the various levels of public health care facilities are presented in Tables III and IV, respectively. Here, using the methodology discussed above, the package costs were calculated for each of the items.
| Contraceptive method | Package health system cost | |
|---|---|---|
| ₹ (95% CI) | US$ (95% CI) | |
| OCP | 1,561 (1227-1890) | 21.7 (17,26.3) |
| Condoms | 839 (712-964) | 11.7 (9.9,13.4) |
| Copper IUD | 1259 (1051-1470) | 17.5 (14.6,20.4) |
| DMPA Injectables | 1164 (954-1367) | 16.2 (13.3-19) |
| LNG-IUS | 3474 (3270-3678) | 48.3 (45.4,51.1) |
| Etonorgestrel implant | 3366 (2897-3862) | 46.8 (40.2-53.6) |
| Tubal ligation | 8885 (7456-10274) | 123.4 (103.6,142.7) |
IUD, intrauterine device; DMPA, depot medroxyprogesterone acetate; LNG-IUS, levonorgestrel intra uterine system; CI, confidence interval; OCP, oral contraceptive pills
| Pregnancy outcomes | Package cost in | |
|---|---|---|
| ₹ (95% CI) | US$ (95% CI) | |
| Abortion | 6921 (5467-8345) | 96.1 (75.9-115.9) |
| Ectopic pregnancy | 7796 (6230-9323) | 108.3 (86.5-129.5) |
| Antenatal care + vaginal delivery | 8047 (6666-9486) | 111.8 (92.6-131.8) |
| Antenatal care + caesarean delivery | 12,899 (10575-15283) | 179.2 (146.9-212.3) |
The highest unit cost was for tubal ligation at ₹ 8885. OCPs, condoms, copper IUD, DMPA cost estimates were ₹ 1561, 839, 1259 and 1164, respectively. LNG-IUD and etonorgestrel implant, which are not in the programme currently, would cost approximately ₹ 3474 and 3366 per woman if introduced.
It was observed that the cost of pregnancy and related events was the highest for those who underwent caesarean delivery at ₹ 12899 and lowest for abortion at ₹ 6921.
Table V shows the package costs at different health facilities. The cost of providing FP and pregnancy-related services across the three levels of healthcare showed that costs increased with increased in the level of healthcare at which the service was provided.
| Procedure | Primary health centre ₹ (US$) | Sub-district hospital ₹ (US$) | District hospital ₹ (US$) | Tertiary care hospital ₹ (US$) |
|---|---|---|---|---|
| OCP | 607 (8.4) | 635 (8.8) | 1456 (20.2) | 1854 (25.8) |
| Copper IUD | 687 (9.5) | 704 (9.8) | 1196 (16.6) | 1435 (19.9) |
| DMPA | 592 (8.2) | 608 (8.4) | 1101 (15.3) | 1339 (18.6) |
| Condoms | 458 (6.4) | 469 (6.5) | 797 (11.1) | 956 (13.3) |
| Tubal ligation | 6008 (83.4) | 6397 (88.8) | 6757 (93.8) | 9049 (125.7) |
| LNG IUS | 2902 (40.3) | 2919 (40.5) | 3411 (47.4) | 3650 (50.7) |
| Etonorgestrel implant | 2351 (32.7) | 2237 (31.1) | 2718 (37.8) | 3600 (50) |
| Vaginal delivery | 3554 (49.4) | 4570 (63.5) | 6627 (92) | 8794 (122.1) |
| Caesarean delivery | NA | 8672 (120.4) | 9858 (136.9) | 12,794 (177.7) |
| Abortion | NA | 4433 (61.6) | 4793 (66.6) | 7084 (98.4) |
| Ectopic | NA | 5108 (70.9) | 5502 (76.4) | 7895 (109.7) |
DMPA, depot medroxyprogesterone acetate; IUD, intrauterine device; LNG-IUS, levonorgestrel intrauterine system; PHC, primary health centre; OCP, oral contraceptive pills; NA, not applicable
Sensitivity analysis: The tornado diagram derived from the OWSA is shown in Figure. In the present study, the components of cost that affected the unit cost of FP services the most were drugs and consumables, total beneficiaries and HR costs. If the prices of drugs and consumables increased, then the unit cost of services increased and if the number of beneficiaries increased, the unit cost of services decreased. This is demonstrated in Figure.
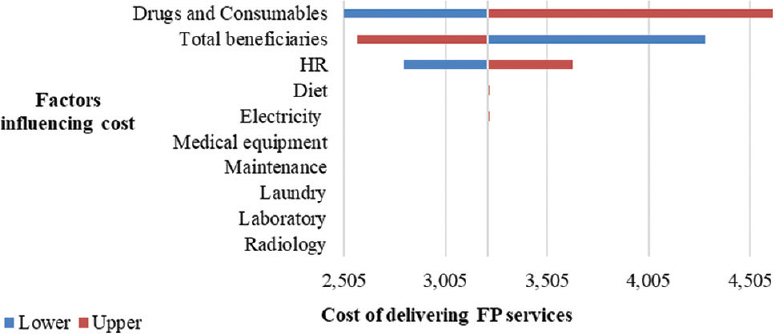
- The tornado diagram shows the factors that influence the costs in the public health system in India.
Discussion
This study evaluated specifically the costs of providing FP services, ANC and delivery care at selected public health facilities in Maharashtra State in India. It was part of a HTA of a newer contraceptive, etonorgestrel implant (containing 68 mg etonorgestrel, radiopaque; brand name: nexplanon/implanon-NXT); to provide evidence to policymakers in deciding whether the introduction of this method into the public health system would be cost-effective.
In developing nations, the cost of providing a modern contraceptive method to one woman per year was estimated to be US $ 1.01 in the year 201719. In the present study, this cost ranged from US $ 12 for condoms to US $ 48 for a contraceptive implant. In a study from Paraguay, done in 2002, the mean costs to the government for vaginal and caesarean delivery were US $ 39 and 5420, respectively. The inflation-adjusted rates: (Paraguay rates US $ 55 and 77) were lower than our study (US $ 112 and 180) because it included the rates of the antenatal care package as well. A study from 1997 showed a wide variation in contraception costs per couple years of protection (CYP) depending on the region and how the contraception was delivered among 14 developing countries. Cost per CYP was similar across Asia, Latin America and the Middle East, ranging from US $ 4 to 5, and were higher in Africa, where the average cost per CYP was US $ 14. These costs per CYP cannot, however, be compared with the present study results. A study done in Africa in 2017 showed an annual cost of facility-based IM injection of DMPA to be US$12. Our study estimates were comparable and stand at US$16.2 (13.3, 19)21.
The cost of one out-patient consultation in the OBGYN department of a DH in our study was ₹ 244. In a study by Prinja et al10, done in North India, in 2015, the speciality-wise unit cost of an outpatient consultation in OBGYN department is reported as a median of ₹165 and a 95 per cent CI of ₹ 68 to 274. The unit cost of the present study also lies within this range. The same study reported inpatient cost of OBGYN department per bed day as ₹ 997 (592, 1412). Our study estimated inpatient unit cost to be ₹ 724 at the secondary level, in the DH. The cost per case operated in DH in our study was ₹ 2398, which also falls within these range. In a study, done in three States in northern India, the mean cost of an OPD consultation was ₹ 139, (95 per cent CI :109,171)10. Our study reports a lower OPD consultation cost at the PHC level to be ₹ 72. Institutional delivery, at the PHC level in their study was reported to cost ₹ 2039 (1547, 2702); our study estimated it to be slightly lower, at ₹ 1495. At the SDH level, OPD and institutional delivery were reported as ₹ 162 and 2225. In our study, the corresponding costs were ₹ 110 and 1738, respectively.
It is to be noted that our package cost of delivering contraceptive methods was higher than other studies. This may be because this study provides a package cost that includes follow up care for one year, the management of side-effects and complications and is based only on OBGYN-related costs. For example, providing IUCD procedure at PHC and CHC level in the study by Prinja et al10 is ₹ 180.7 and 77.9, respectively. This was derived by taking a ratio of total annual cost and the beneficiaries in the facility. In the present study, the cost of providing copper intrauterine device is ₹ 1259. This is because, a package of costs, covering OPD consultation for insertion, removal, side-effects, programme costs, like incentives and training were calculated. The cost of providing antenatal care and vaginal delivery was calculated to be ₹ 8047 and caesarean delivery at ₹ 12,899. A study reported in 2005, reports ₹ 3800 and 8600, respectively22.
Our study package rates for vaginal delivery, caesarean delivery; abortion and ectopic pregnancy were comparable to the publicly funded insurance scheme in India, Ayushman Bharat Pradhan Mantri Jan Arogya Yojana (Table VI). The delivery rates were comparable to the Central Government Health Scheme, however, the Employees’ State Insurance Corporation scheme has low package rates for the same (Table VI) and our study results can be used to revise these rates. The insurance schemes do not, however, provide a breakdown of their final reimbursement amount; hence determining the reason for the difference between our study’s costs and that of the schemes will be difficult.
| Procedure | Cost from the present study (₹) | PMJAY23 (₹) | CGHS scheme24 (Non-NABH hospitals) (₹) | CGHS scheme24 (NABH hospitals) (₹) | ESIC scheme25 (ESI hospitals) (₹) |
|---|---|---|---|---|---|
| Normal delivery | 8047 | 9000 | 8000 | 9200 | 2500 |
| Caesarean section | 12,899 | 9000 | 14,050 | 16,158 | 4500 |
| Medical termination of pregnancy (>12 wk) | 6921 | 6500 | - | - | - |
| Ectopic pregnancy management | 7796 | 10,000 | - | - | - |
| OPD consultation | 218 | - | 150 | 150 | - |
| IPD consultation | 673 | - | 300 | 300 | - |
CGHS, Central Government Health Scheme; ESI, Employees’ State Insurance; ESIC, ESI corporation; IPD, inpatient department; OPD, outpatient department; PMJAY, Pradhan Mantri Jan Arogya Yojana; NABH, National Accreditation Board for Hospitals & Healthcare Providers
Table VI shows the cost difference in providing contraceptive methods at the different health facilities. These differences are likely to be due to the difference in the infrastructure and the type of services offered at the different levels; for instance, OT facilities are better and more advanced in the DH and tertiary care hospital as compared to the SDH. There is also a difference in the number of beneficiaries at the different health facilities.
Study limitations: The present study was not without its limitations. Firstly, it was not a stand-alone economic costing study (costing was done as a part of the economic evaluation for HTA); the sample facilities chosen were limited to one each from every level of healthcare in the Indian public health system (PHC, SDH, DH and tertiary care hospital). Secondly, the PHC and the DH had adequate total staffing and beds, however, the SDH was short of total staff. The SDH was hundred bedded but has only 65 total staff as compared to the IPHS recommended 95 to 146 staff. Thirdly, the data on the prices of equipment received from the facilities were not complete and we had to refer to market price for a few equipments. The average life of the equipment was also not available with the facilities. The date of purchase was also available only for a few, hence an average of 10-15 yr was used for all equipments in annualization calculations. Lastly, the sensitivity analysis varied the number of beneficiaries, drugs and consumables, laboratory investigations and infrastructure costs; however, the capacity utilization and staff numbers could not been varied.
Overall the present study provides unit and package costs of delivering FP and pregnancy-related services. Costs derived from this study can be used by programme managers and policymakers. These can also be used by publicly-funded insurance schemes to revise their package rates, government departments and agencies for budget-impact analyses and also for conducting economic evaluations. The study provides unit cost estimates for newer contraceptive methods under consideration for programme introduction in India. Government budgets also could consider the extent to which out-of-pocket expenditure could be reduced in spite of providing these services at negligible costs232425.
The way forward for improving cost evidence in India; would be to encourage health facilities to maintain better records of costs and details of the year of purchase of commodities, and for researchers to include a more diverse sample of facilities.
Acknowledgment:
Authors acknowledge, DHR HTAIn Secretariat, the Director-General ICMR and the Director NIRRCH, Mumbai, for their support in carrying out this study. Authors also acknowledge all the authorities and staff from all health facilities where this data collection was undertaken. We thank Dr Shankar Prinja and his team at PGIMER, Chandigarh, for guiding us in this analysis.
Financial support & sponsorship: This study was funded by the Department of Health Research, MoHFW, India (grant no. T.11011/02/2017-HR/3100291).
Conflicts of Interest: None.
References
- World Health Organization. The ABC's of family planning. Available from: https://pmnch.who.int/
- National Health Mission. Ministry of Health and Family Welfare, Government of India. Indian public health standards. Available from: https://nhm.gov.in/index1.php?lang=1&level=2&sublinkid=971&lid=154
- International Institute for Population Sciences. National family health survey, India. Available from: http://rchiips.org/nfhs/factsheet_nfhs-4.shtml
- Population Foundation of India. Cost of inaction in family planning in India: An analysis of health and economic implications. New Delhi: PFHI; 2018.
- Indian Council of Medical Research. National Health System Cost Database for India. Family planning unit cost database. Available from: https://www.healtheconomics.pgisph.in/costing_web/index.php?action=gen_output
- A cost analysis of deliveries conducted in various health care settings in a city of India. Healthline. 2011;2:61-4.
- [Google Scholar]
- Cost of hospitalization for childbirth in India:How equitable it is in the post-NRHM era? BMC Res Notes. 2017;10:409.
- [Google Scholar]
- Cost of delivering secondary-level health care services through public sector district hospitals in India. Indian J Med Res. 2017;146:354-61.
- [Google Scholar]
- Cost of delivering health care services in public sector primary and community health centres in North India. PLoS One. 2016;11:e0160986.
- [Google Scholar]
- World Health Organization. Estimation of unit costs for general health services: Updated WHO-CHOICE estimates: Technical background report 2011
- Unit cost of medical services at different hospitals in India. PLoS One. 2013;8:e69728.
- [Google Scholar]
- Unit cost of healthcare services at 200-bed public hospitals in Myanmar:What plays an important role of hospital budgeting? BMC Health Serv Res. 2017;17:669.
- [Google Scholar]
- The determinants of hospital cost:A cost-volume-profit analysis of health services in the occupied territories:Palestine. Int J Pharm Pract. 2010;18:167-73.
- [Google Scholar]
- Health technology assessment in India: A manual. Available from: http://htain.icmr.org.in/modules/mod_flipbook_8/tmpl/book.html
- Health management information system. Available from: https://hmis.nhp.gov.in/#!/
- XE: Convert USD/INR. United States dollar to India rupee. Available from: https://www.xe.com/currencyconverter/convert/?Amount=1&From=USD&To=INR
- Guttmacher Institute. Adding it up: Investing in contraception and maternal and newborn health, 2017-Estimation methodology. Available from: https://www.guttmacher.org/report/adding-it-up-investing-in-contraception-maternal-newborn-health-2017-methodology
- Cost and efficiency of reproductive health service provision and the facility level in Paraguay. Available from: https://www.measureevaluation.org/resources/publications/wp-02-45.html
- Costs of administering injectable contraceptives through health workers and self-injection:Evidence from Burkina Faso, Uganda, and Senegal. Contraception. 2018;98:389-95.
- [Google Scholar]
- Cost factors related with normal vaginal delivery and caesarean section in government and non-government settings. Indian J Community Med. 2005;30:2.
- [Google Scholar]
- National Health Authority. Health Benefit Packages | Ayushman Bharat. Available from: https://pmjay.gov.in/hbc
- Central Government Health Scheme, Ministry of Health & Family Welfare, Government of India. Home – CGHS. Available from: https://cghs.gov.in/
- Employees' State Insurance Corporation. Ministry of Labour & Employment, Government of India. Homepage. Available from: https://www.esic.nic.in/
- Pattern and correlates of out-of-pocket payment (OOP) on female sterilization in India, 1990–2014. BMC Womens Health. 2020;20:13.
- [Google Scholar]






