Translate this page into:
Coronin-1 levels in patients with tuberculosis
For correspondence: Dr Sanjeev Sinha, Department of Medicine, All India Institute of Medical Sciences, Ansari Nagar, New Delhi 110 029, India e-mail: drsanjeevsinha@gmail.com
-
Received: ,
This article was originally published by Wolters Kluwer - Medknow and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Background & objectives:
Despite advances in diagnostics and therapeutics, tuberculosis (TB) is widely prevalent and contributes to a significant burden of illness in both developing and developed nations. The present study was aimed to assess the role of coronin in TB patients and healthy controls. Coronin is a leucocyte-specific protein that is actively recruited in mycobacterial phagolysosomes, where it inhibits lysosomal delivery of Mycobacterium by activating a calcium-dependent phosphatase-calcineurin.
Methods:
In the study, 100 newly diagnosed cases of TB (pulmonary and extra-pulmonary) and healthy controls were prospectively enrolled over one year and the levels of coronin-1a in these patients and controls were measured by quantitative PCR (qPCR).
Results:
A total of 100 TB patients and 100 healthy individuals as controls were assessed. There were 59 patients with extra-pulmonary TB (EPTB) and 41 of pulmonary TB (PTB). In 47 per cent of patients, corroborative histopathological evidence of TB was also available. Significantly higher values of coronin-1a were observed in TB patients (19.94±2.61) than in healthy controls (16.09±1.91) (P<0.001).
Interpretation & conclusions:
Coronin 1a appears to play an important role in the TB disease pathophysiology and agents developed against coronin may have a role in the treatment of TB. Further studies are required to assess if coronin-1a levels are elevated in non-tubercular infective a etiologies and whether these can be a potential drug target in patients with TB.
Keywords
Coronin
drug therapy
EPTB
phagolysosome
PTB
tuberculosis
Tuberculosis (TB) is a serious bacterial infection caused by Mycobacterium tuberculosis (MTB). Historically known as consumption due to its ability to cause severe weight loss in patients, the disease is still widely prevalent worldwide with the major disease burden localized in the developing nations1. The World Health Organization estimates that 62 per cent of new cases of TB are found in the South-East Asia and Western Pacific region. As per the WHO global report on TB (2021), 1.4 million people die of TB worldwide2. Half a million patients had drug-resistant TB, of whom only 186,772 were diagnosed and only 57 per cent of these patients responded appropriately to treatment2. Despite this, the incidence of TB is falling by about two per cent per year, but to meet the milestones of the End TB strategy, this must accelerate to a 4-5 per cent annual decline3.
For the effective implementation of the End TB strategy, understanding the pathophysiology of MTB, particularly the mechanisms of evasion of the immune surveillance of the body, becomes a pertinent issue. The formation of the phagolysosome in macrophages is considered to be the keystone of the immune response to TB. This leads to autophagy and the destruction of the bacterium. The induction of autophagy is a prospective target of drug therapy and new vaccine development3. Over the time, MTB has developed methods subverting phagolysosome formation and therefore, survive inside macrophages. In absence of autophagy, the intracellular burden of the organism continues to increase and leads to the persistence of the disease. Subversion of phagolysosome formation is achieved by modulating the trafficking of Ras-associated binding (Rab) GTPases which leads to maturation arrest of phagosomes4. Coronin-1a is a key player in the above-mentioned mechanism. It is a leucocyte-specific protein which is upregulated in infections and is actively recruited in mycobacterial phagolysosomes, where it inhibits lysosomal delivery of Mycobacterium by activating a calcium dependant phosphatase-calcineurin5.
Knock-out studies in mice reveal that in other infections, coronin-1a is not an essential component in the processes of phagocytosis, membrane ruffling or motility- components of the immune system in removing infectious agents6. Thus, inhibition of coronin-1 would lead to decreased calcineurin levels and interfere with the mechanism of evasion employed by MTB to avoid phagolysosomes. In the current study, the objective was to evaluate levels of coronin-1a in TB patients and healthy individuals using quantitative polymerase chain reaction (qPCR).
Material & Methods
This was a prospective observational study conducted over one year (2016-2017) at the DOTS Centre for Diagnosis and Treatment of TB at the All India Institute of Medical Sciences, New Delhi, India.
One hundred consecutive patients with pulmonary TB (PTB) and an equal number of healthy individuals as controls were included in the study group. Pulmonary TB was defined as a patient with relevant clinical manifestations (such as cough >2-3 wk duration, lymphadenopathy, fever, night sweats, weight loss) and epidemiologic factors (such as the history of prior TB infection or disease, known or possible TB exposure, and/or past or present residence in or travel to a TB endemic area) which is supported by imaging features and definitive diagnosis achieved by isolation of MTB from a body secretion or fluid (e.g. culture of sputum, bronchoalveolar lavage or pleural fluid) or tissue (e.g. pleural biopsy or lung biopsy). Additional diagnostic tools include sputum acid-fast bacilli (AFB) smear and nucleic acid amplification testing (NAAT); a positive NAAT (with or without AFB smear positivity) in a person at risk for TB78. Extrapulmonary TB (EPTB) was defined as a patient with relevant clinical manifestations (such as lymphadenopathy, fever, night sweats, weight loss) and epidemiologic factors (such as history of prior TB infection or disease, known or possible TB exposure, and/or past or present residence in or travel to a TB endemic area). TB involving organs other than pulmonary involvement (e.g. pleura, lymph nodes, abdomen, genitourinary tract, skin, joints and bones, or meninges) which is confirmed by identification by AFB staining and/or NAAT of tissue sampled from affected area9. Any patient who had both area was considered to be a case of PTB.
All consecutive patients who consented to be a part of the study and met the inclusion criteria were included in the study. Patients already on therapy for TB or receiving any form of immunosuppressant drugs or steroids, patients with chronic liver or kidney disease, chronic alcoholics [consuming more than 4 units (40 g/day) for males or more than 2 units (20 g/day) of alcohol per day for at least one year]10 and those having concomitant administration of other hepatotoxic drugs for other illnesses (e.g. methotrexate, phenytoin, valproate) were excluded from the study. Controls were healthy individuals who did not have TB and had normal baseline liver and kidney function tests, and who were willing to participate in the study.
Blood collection, RNA isolation, RT-PCR: Blood (8 ml) was drawn from each patient and control in an ethylenediaminetetraacetic acid (EDTA) vial on their visit to the DOTS centre. The blood was be divided into two aliquots- for RNA and DNA isolation, respectively. RNA isolation was done by peripheral blood mononuclear cells (PBMC) isolation using 6 ml of blood. The blood samples were diluted in 1:1 ratio with phosphate-buffered saline (PBS). This was layered over Ficoll-Hypaque in 1:2 ratio, centrifuged at 700 g for 20 min. The white buffy coat was separated and collected in a fresh falcon. These PBMC were washed with PBS twice and pelleted by centrifuging at 1008 g for 10 min followed by RNA isolation by Trizol (Thermo Fisher Scientific, USA). The buffy coat was diluted in 1 ml of Trizol and mixed well. To this, 200 µl of chloroform was added, centrifuged at 18928 g for 15 min. The transparent layer was pipetted out and collected in a fresh Eppendorf tube. This was processed through an RNA binding column by Qiagen (Qiagen, Hilden, Germany). RNA samples were checked on non-denaturing one per cent agarose gel with 1x TAE (trisbase, acetic acid and EDTA) and RNA integrity number (RIN) was checked by Agilent 2100 Bioanalyser G2938C systems (Agilent Technologies, CA, USA).
DNA was isolated from 400 µl of whole blood using Qiagen DNA isolation kit (Qiagen, Hilden, Germany). The DNA bands were checked on agarose gel for visualization. The isolated DNA was used for amplification of the PPP3CA (calcineurin) gene. The reaction mixture for each sample with a total reaction volume as 20 µl was used for qPCR of the PPP3CA gene. The DNA sequencing for the amplified product was done using the ddNTPs Sanger’s sequencing method. BigDye® terminator (BigDye Terminator v3.1 Cycle Sequencing Kit, Thermo Fisher Scientific, USA) was used and the protocol was followed as per the manufacturer’s instructions. The PCR product was cleaned up using the QIAquick PCR purification kit (Qiagen, Hilden, Germany).
To synthesize the complementary DNA, isolated RNA was used and cDNA was synthesized using Agilent AccuScript High Fidelity 1st Strand cDNA Synthesis Kit (Agilent Technologies, Stratagene Products Division, CA, USA) as per the manufacturer’s protocol. After cDNA was synthesized, these were stored at −80°C and used for qPCR of coronin-1.
For coronin, qPCR was performed using the deltadelta Ct (ΔΔCt) method6. The threshold cycle (Ct) values for both patients and controls were subtracted from the Ct values of the reference gene (in this case β-actin) to give the delta Ct (ΔCt) values. The ΔΔ Ct values were obtained by using the formula: ΔΔCt = ΔCtcoronin − ΔCtβ-actin. For real-time PCR, Agilent Brilliant III Ultra-Fast SYBR Green qPCR master mix (Agilent Technologies, Stratagene Products Division, CA, USA) was used as per the manufacturer’s instructions.
Statistical analysis: The data were analyzed using Stata 14 software (StataCorp. 2011. College Station, TX, USA). To compare the baseline demographic and biochemical parameters between the two groups, Chi-square test was used for categorical variables and Student’s t test was used for continuous variables with normal distribution.
Results
One hundred patients with of TB and 100 healthy controls were assessed over one year. The TB patients comprised 58 cases of EPTB and 42 cases of PTB. The demographic characteristics of the patients are shown in Table I. Mean age and gender distribution in both groups were comparable. Family history of TB was present in 67 per cent TB patients. AFB were identified in 87 and 91 per cent showed positive Xpert MTB/RIF. In 47 per cent patients, corroborative histopathological evidence of TB was also available (Table I). Both groups of participants underwent renal and liver function tests. As compared to controls, patients with EPTB had significantly lower values of haemoglobin, uric acid, and serum calcium while erythrocyte sedimentation rate (ESR), platelets and urea levels were higher. Patients with PTB had significantly lower haemoglobin than controls and demonstrated significantly (P<0.05) higher levels of platelets, total leucocyte counts, ESR and serum urea. As compared to EPTB patients, those who had PTB had higher total leucocyte counts (Table II).
| Parameters | TB (n=100) | Controls (n=100) |
|---|---|---|
| Age (yr), mean±SD | 36±12 | 37±8 |
| Gender, n (%) | ||
| Male | 58 (58) | 55 (55) |
| Female | 42 (42) | 45 (45) |
| AFB positive, n (%) | 87 (87) | Not applicable |
| GeneXpert positive, n (%) | 91 (91) | Not applicable |
| Histopathology, n (%) | 47 (47) | Not applicable |
TB, tuberculosis; AFB, acid-fast bacilli
| Laboratory parameters | Control (n=100) | EPTB (n=58) | PTB (n=42) |
|---|---|---|---|
| Hemoglobin (gm/dl) | 14.1±1.7 | 12.3±1.9* | 12.3±1.8* |
| White blood cell count (×109/l) | 7.3±1.4 | 7.7±2.7 | 9.5±2.8*,# |
| Platelet count (×109/l) | 225±72.2 | 241±100.9 | 261±96.8 |
| ESR (mm/h) | 11.1±3.6 | 29.7±19.6* | 31.9±18.6* |
| Urea (mg/dl) | 21.9±5.4 | 26.5±9.6* | 25.1±7.2* |
| Creatinine (mg/dl) | 0.7±0.1 | 0.9±0.3 | 0.7±0.2 |
| Total bilirubin (mg/dl) | 0.6±0.6 | 0.6±0.3 | 0.5±0.2 |
| Total protein (g/dl) | 7.1±0.7 | 6.9±1.6 | 7.3±0.8 |
| AST (IU/l) | 30.9±9.2 | 33.3±14.8 | 28.4±19.8 |
| ALT (IU/l) | 25.6±16.5 | 30.2±20.7 | 30.1±19.7 |
| ALP (IU/l) | 178.4±29.6 | 190.6±71 | 200.1±77.4 |
| Uric acid (mg/dl) | 5.2±1.3 | 4.2±1.5* | 4.8±1.4 |
| Calcium (mg/dl) | 9.1±0.6 | 8.2±0.3* | 8.8±0.4 |
| Phosphorous (mg/dl) | 3.4±0.6 | 3.8±0.9 | 3.8±0.6 |
| Total cholesterol (mg/dl) | 178.4±29.7 | 73.3±93.5 | 83.5±86.1 |
Data are presented as mean±SD. P *<0.05 compared to control; P #<0.05 compared to EPTB. AST-Aspartate transaminase; ALT- Alanine transaminase; ESR- erythrocyte sedimentation rate; EPTB- extra-pulmonary tuberculosis; PTB-pulmonary tuberculosis
There was a significant difference between the ΔCt values of coronin-1a between patients and controls (19.94±2.61 vs. 16.09±1.91; P<0.001). To analyze the fold-change of coronin-1a among the patients, the 2−ΔΔCt formula was used. There was significant (P< 0.05) increase in the copy numbers of coronin-1a gene in TB patients as compared to healthy controls (Figure). The median value for ΔΔCt value was 8.3 (interquartile range 3.3-45.2).
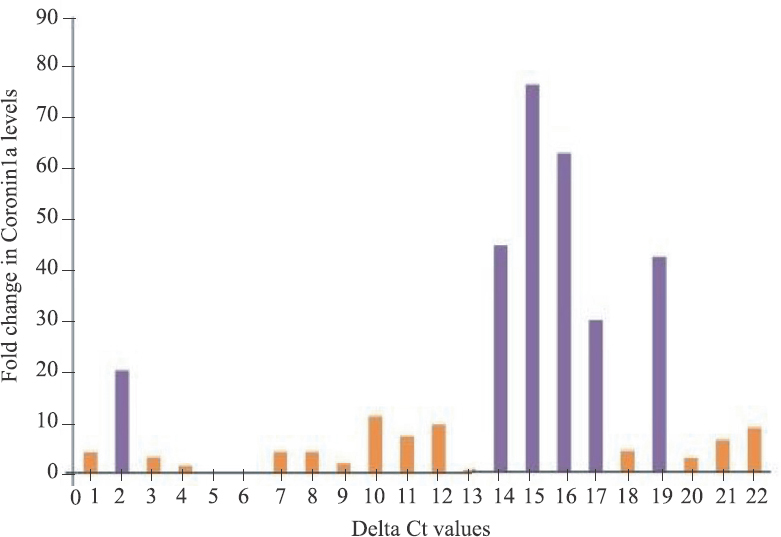
- Representative picture for fold change observed in TB cases with respect to healthy controls for coronin-1a.
Discussion
Coronins are proteins with broad expression in the eukaryotic world. These have amino-terminal tryptophan-aspartate residues that bind to carboxy-terminal spiral convoluted domains, which are necessary for their oligomerization. Seven coronin genes have been identified in mammals- coronins; 1 to 6 have the classic coronin structure, while coronin 7 is a tandem coronin particle without a spiral domain. The best-characterized coronin is the mammalian coronin 111. Coronins do not have trans-membrane domains and bind to the membrane through interaction with cholesterol. Coronin-1 is an actin-binding protein that activates calcineurin and prevents the formation of the phagolysosome in macrophages5. MTB avoids the destruction in human body by recruitment of tryptophan-aspartate-containing coating proteins which get localized in the cytoplasm of the Mycobacterium containing macrophage10. This protein was later identified as coronin. Coronin also has a role in leprosy and Helicobacter pylori infections and has also been found to be involved in the pathophysiology of viral infections11.
Previous studies have shown that coronin plays a role in activating calcium fluxes in macrophages1213. It is believed that the mycobacteria utilize the physiological calcium flux in macrophages to enhance their survival but at the same time, prevent those fluxes in calcium that trigger macrophage microbicidal effects that may be detrimental to their survival. In coronin-1 deficient macrophages where such physiological fluxes of calcium do not occur, mycobacteria are routed to lysosomes and killed13.
Significantly higher levels of coronin-1 were observed in patients suffering from TB as compared to normal controls. Genetic analysis of patients with TB may provide further insight as to the mechanism of the immune response of a person when challenged with a tubercular infection141516. These patients will also be expected to have a protracted course of illness and may have a poorer response to the traditional anti-tubercular therapy14.
The present study was a pilot study with certain limitations. The sample size was a sample of convenience and further did not highlight the significant difference of levels of coronin between EPTB and PTB patients.
The study highlights the importance of genetic screens analyzing pathways involved in survival of MTB to counteract these host immune defence mechanisms. This has a potential outcome as there have been a few new drugs in the treatment of TB and the newer agents have significant adverse effect profile and toxicity on long-term use. With the rise in the number of multidrug-resistant and extensively drug resistant TB cases, new drugs for the effective treatment of TB and new drug targets are the need of the hour17.
In conclusion, significantly higher levels of coronin 1a were found in TB patients as compared to healthy controls. Coronin appears to play an important role in the disease pathophysiology and agents developed against coronin may have a role in the treatment of TB. Further studies including genetic analysis of TB patients may shed more light on the role of coronin in humans as well as its potential applications in therapy.
Acknowledgment
Authors thank the staff members of the DOTS clinic and SRB Lab and project staff for their help during patient enrolment and follow up and acknowledge the support of Dr Mikashmi Kohli for doing the laboratory experiments.
Financial support & sponsorship: Department of Pharmaceuticals, Ministry of Chemical and Fertilizers, Government of India, New Delhi, provided financial support for this study.
Conflicts of Interest: None.
References
- World Tuberculosis Day 2021 Theme – ‘The Clock is Ticking’ – And the world is running out of time to deliver the United Nations General Assembly commitments to end TB due to the COVID-19 pandemic. Int J Infect Dis. 2021;113:Suppl 1-6.:S1-6.
- [Google Scholar]
- Latent tuberculosis infection and the EndTB Strategy: Ethical tensions and imperatives. Int J Tuberc Lung Dis. 2020;24:21-6.
- [Google Scholar]
- Autophagy adaptor protein p62/SQSTM1 and autophagy-related gene Atg5 mediate autophagosome formation in response to Mycobacterium tuberculosis infection in dendritic cells. PLoS One. 2013;8:e86017.
- [Google Scholar]
- A Rab20-dependent membrane trafficking pathway controls M. tuberculosis replication by regulating phagosome spaciousness and integrity. Cell Host Microbe. 2017;21:619-28.e5.
- [Google Scholar]
- Coronin-1 is a neurotrophin endosomal effector that is required for developmental competition for survival. Nat Neurosci. 2014;17:36-45.
- [Google Scholar]
- Official American Thoracic Society/Infectious Diseases Society of America/Centers for Disease Control and Prevention clinical practice guidelines: Diagnosis of tuberculosis in adults and children. Clin Infect Dis. 2017;64:e1-33.
- [Google Scholar]
- Tuberculosis diagnostics: State of the art and future directions. Microbiol Spectr. 2016;4:4-5.
- [Google Scholar]
- Diagnosis and treatment of extrapulmonary tuberculosis. Tuberc Respir Dis (Seoul). 2015;78:47-55.
- [Google Scholar]
- Coronins and their role in immunological phenomena. Cent Eur J Immunol. 2016;41:435-41.
- [Google Scholar]
- Endosomal actin remodeling by coronin-1A controls lipoprotein uptake and degradation in macrophages. Circ Res. 2012;110:450-5.
- [Google Scholar]
- Getting in and Staying Alive: Role for Coronin 1 in the Survival of Pathogenic Mycobacteria and Naïve T Cells. Front Immunol. 2018;9:1592.
- [Google Scholar]
- Coronin-1a inhibits autophagosome formation around Mycobacterium tuberculosis-containing phagosomes and assists mycobacterial survival in macrophages. Cell Microbiol. 2012;14:710-27.
- [Google Scholar]
- “It Takes Two to Tango”: Role of Neglected Macrophage Manipulators Coronin 1 and Protein Kinase G in Mycobacterial Pathogenesis. Front Cell Infect Microbiol. 2020;10:582563.
- [Google Scholar]
- Survival of mycobacteria in macrophages is mediated by coronin 1-dependent activation of calcineurin. Cell. 2007;130:37-50.
- [Google Scholar]
- Future target-based drug discovery for tuberculosis? Tuberculosis (Edinb). 2014;94:551-6.
- [Google Scholar]






