Translate this page into:
A systematic review on the prevalence of endometriosis in women
For correspondence: Dr Zahra Najmi, Department of Obstetrics and Gynecology, Fellowship of Minimally Invasive Gynecology Surgery, Zanjan University of Medical Sciences, Zanjan 451 395 6111, Iran e-mail: zahranaj@yahoo.com
-
Received: ,
This article was originally published by Wolters Kluwer - Medknow and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Background & objectives:
Endometriosis is one of the causes of female infertility, but the prevalence of endometriosis is not exactly known. We conducted a systematic review and meta-analysis to provide an estimate of the prevalence of endometriosis in women considering the stage of disease, diagnostic method, geographical distribution, clinical symptoms and sample size.
Methods:
MEDLINE, Web of Science, Google Scholar, Scopus and Cumulative Index of Nursing and Allied Health were searched to identify peer-reviewed studies published from January 1990 to December 2018 reporting the prevalence of endometriosis. Relevant additional articles were identified from the lists of the retrieved articles. Studies with cross-sectional design were included in the meta-analysis.
Results:
The overall prevalence of endometriosis was 18 per cent [95% confidence interval (CI): 16-20] and the prevalence of endometriosis by stage ranged from two per cent (95% CI: 1-4) for stage 4 to 20 per cent (95% CI: 11-28) for stage 1. The prevalence levels of endometriosis in women with infertility, chronic pelvic pain and asymptomatic were 31 (95% CI: 15-48), 42 (95% CI: 25-58) and 23 per cent (95% CI: 19-26), respectively.
Interpretation & conclusions:
The results of this study showed that the prevalence of endometriosis in developing countries was high. Future studies are needed to explore other factors affecting the prevalence of endometriosis worldwide, which may help develop future prevention programmes.
Keywords
Endometriosis
prevalence
quality assessment
women
Endometriosis affects about 6-10 per cent of women worldwide1. In Canada and the United States, the incidence of endometriosis ranges from 5 to 15 per cent in the women of reproductive age and from 2 to 5 per cent in postmenopausal women2345. The majority of patients with endometriosis are asymptomatic, and only 6-10 per cent of them suffer from pelvic pain6. This chronic gynaecological disease is accompanied with different symptoms such as chronic pelvic pain, dyschezia, lower back pain, dyspareunia, infertility and dysmenorrhoea7. Epidemiological indicators such as prevalence can be useful for healthcare managers and policymakers. Thus, a systematic review and meta-analysis was undertaken to provide an estimation of the prevalence of endometriosis in women.
Material & Methods
Search strategy: All international databases including MEDLINE, Web of Science, Google scholar, Scopus and Cumulative Index to Nursing and Allied Health Literature were searched for the original articles without language and time limitation, written from January 1990 to December 2018. Keywords were searched electronically by two independent Boolean operators using a specified search strategy. The protocol of this study was registered in the International Prospective Register of Systematic Reviews (PROSPERO) (CRD42017075275)8.
Inclusion/exclusion criteria: Two reviewers independently carried out the literature search and evaluation of the searched articles based on the inclusion and exclusion criteria. The structures of the searched articles were appraised by the reconstructed PRISMA checklist9. All the articles with full text in English conducted as a cross-sectional design reporting the prevalence of endometriosis in any stage of the disease in women aged 15-60 yr old, were include.
Data extraction: Using a uniform excel sheet, two reviewers independently extracted the required data from the data contained in the identified articles. Discrepancies in the extracted data were resolved through consensus, and if agreement could not be reached, they resolved it by referral to a third investigator. The STROBE checklist10 was used as a standard checklist for reporting the results of the included studies.
Quality assessment and risk of bias: The quality of each study was assessed according to the Quality Assessment Tool for Observational Cohort and Cross-Sectional Studies11 which included the quality of research question, study population, sampling strategy, groups recruited from the same population and uniform eligibility criteria, sample size justification, exposure assessed before outcome measurement, sufficient timeframe to observe an effect, different levels of the exposure of interest, exposure measurement and assessment, repeated exposure assessment, outcome measurement, blinding of outcome assessors, follow up rate and statistical analyses. This tool measures 14 different criteria which are used to give each study an overall quality rating of good, fair or poor.
Statistical analysis: Random effects models were used based on the presence of heterogeneity. Heterogeneity was assessed using Q Cochran’s test and I2 index12. The forest plot was implemented for showing the results of the individual and pooled effects of all the studies. The Egger’s test was also used to evaluate the presence of publication bias12. In addition, a subgroup analysis was done (by sample size, stages of endometriosis, diagnostic method, continent and clinical symptoms) to identify different sources of heterogeneity. A P<0.05 was considered significant for all statistical tests, except for Q Cochran’s, meta-regression and Egger’s test (<0.1). All statistical analyses were performed through STATA version 12.0 (STATA Corp., College Station, TX, USA).
Results
A total of 2433 articles were extracted for this study. Finally, 17 studies1314151617181920212223242526272829 with 127,476 women suffering from endometriosis were included for estimating the prevalence of endometriosis (Fig. 1). The characteristics of the included studies are described in Table I. The quality assessment details for the included studies are shown in Table II.
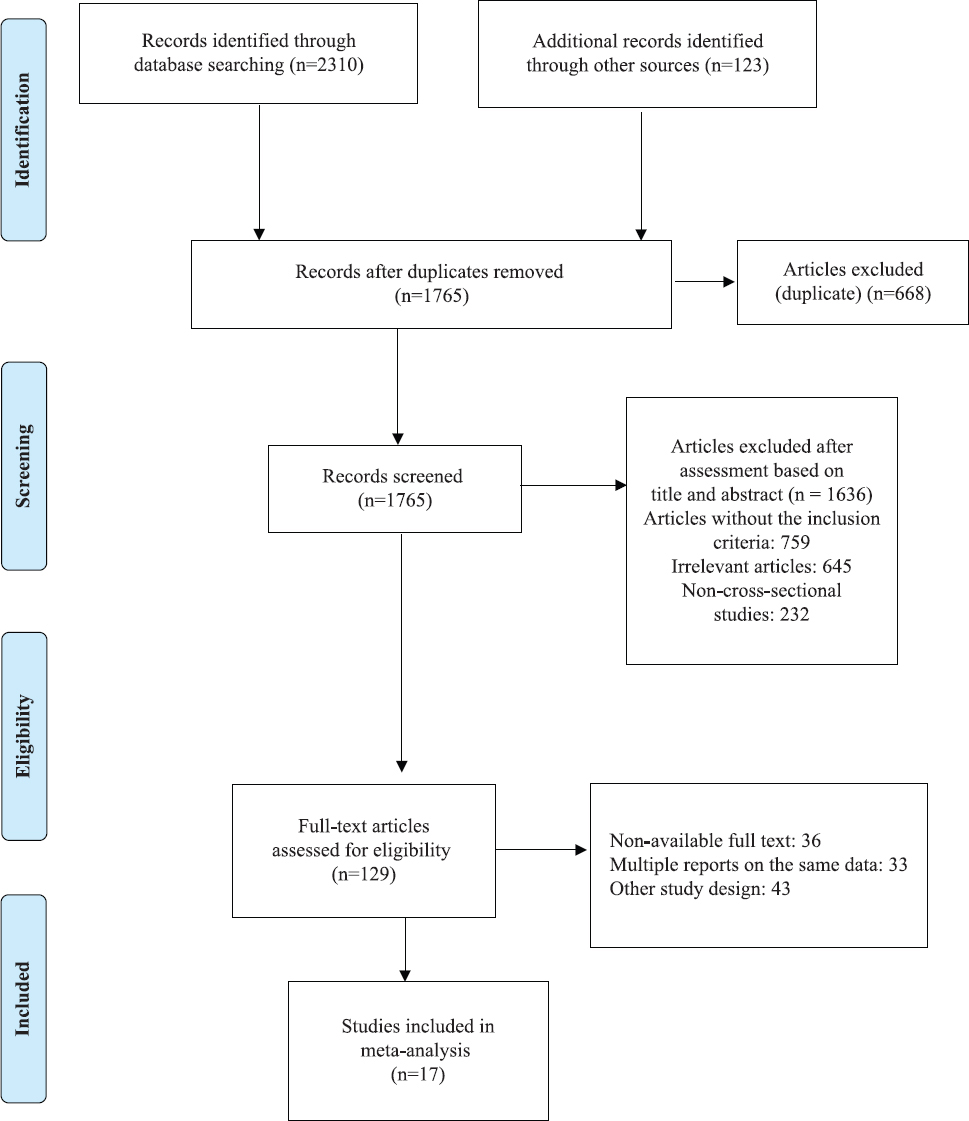
- Flow diagram showing literature search and study selection.
| Authors | Publication year | Data collection year | Country | Age (yr) | Sample size | Study population | Diagnostic method | Prevalence (%) | ||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| All stages | Stage 1 | Stage 2 | Stage 3 | Stage 4 | ||||||||
| Moen and Muus12 | 1991 | 1986-1989 | Norway | 20-50 | 208 | Asymptomatic women | Laparoscopic | 19.23 | 19.23 | 0.93 | - | 0.93 |
| Waller et al13 | 1993 | 1990-1992 | United Kingdom | 21-45 | 174 | Asymptomatic women | Laparoscopic | 32.2 | 22.98 | 7.47 | 1.72 | - |
| Melis et al14 | 1994 | 1991-1993 | Italy | 15-57 | 305 | Asymptomatic women | Laparoscopic | 24.9 | 9.15 | 26.2 | 7.86 | 5.24 |
| Chu et al15 | 1995 | 1993 | Taiwan | - | 752 | Asymptomatic women | Laparoscopic | 32.5 | - | - | - | - |
| Laufer et al16 | 1997 | 1990-1994 | USA | 13-21 | 46 | Women with chronic pelvic pain | Laparoscopic | 69.6 | 77.4 | 22.6 | - | - |
| Oral et al17 | 2003 | 1995-2001 | Turkey | 26-70 | 183 | Malignant epithelial ovarian tumours | Histopathological criteria | 7.65 | 4.37 | 4.37 | 3.27 | - |
| Darwish et al18 | 2006 | 1998-2005 | Egypt | - | 2493 | Women with chronic pelvic pain | Laparoscopic | 18.8 | 34.9 | 39.6 | 10.3 | 15.2 |
| Zacharia and O’Neill19 | 2006 | 2000-2003 | USA | 32-54 | 59 | Asymptomatic women | MRI | 34 | - | - | - | - |
| Ferrero et al20 | 2010 | 2007-2009 | Italy | <50 | 1291 | Infertile women | Ultrasound | 3.6 | - | - | - | - |
| Camilleri et al21 | 2011 | 2003-2008 | Malta | - | 437 | Infertile women | Laparoscopic | 16.9 | 8.69 | - | 1.37 | 0.91 |
| Abbas et al22 | 2012 | 2007 | Germany | 15-54 | 62323 | Infertile women | Laparoscopic | 0.81 | - | - | - | - |
| Fawole et al23 | 2015 | 2008-1010 | Nigeria | 18-45 | 245 | Asymptomatic women (in women with chronic pelvic pain=55.8%) | Laparoscopic | 48.1 | - | - | - | - |
| Ragab et al24 | 2015 | 2012-2014 | Egypt | - | 654 | Girls with severe dysmenorrhoea | Ultrasonography/laparoscopy/MRI | 12.3 | 5.45 | 3.18 | 3.63 | - |
| Umelo and Manchanda25 | 2015 | 2012-2014 | Indian | 15-49 | 440 | Asymptomatic women (infertile women=87.3% and in women with chronic pelvic pain=56.4%) | Laparoscopic | 25 | 7.3 | 35.5 | 31.8 | 25.1 |
| Fuldeore and Soliman26 | 2016 | 2012 | USA | 18-49 | 48020 | Asymptomatic women | Laparoscopic | 6.1 | - | - | - | - |
| Boujenah et al27 | 2017 | 2007-2015 | France | - | 52 | Infertile women | Ultrasonography/laparoscopy/MRI | 50 | - | - | - | - |
| Eisenberg et al28 | 2017 | 1998-2015 | Israel | 15-55 | 6146 | Asymptomatic women | Laparoscopic | 1.1 | - | - | - | - |
MRI, magnetic resonance imaging
| Authors | Q1 | Q2 | Q3 | Q4 | Q5 | Q6 | Q7 | Q8 | Q9 | Q10 | Q11 | Q12 | Q13 | Q14 | Quality rating | STROBE score |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Moen and Muus12 | Yes | Yes | Yes | NR | NR | NR | Yes | NA | Yes | No | Yes | No | No | No | Fair | 16 |
| Waller et al13 | Yes | Yes | NR | Yes | No | No | NA | NA | Yes | No | Yes | NR | NR | NA | Fair | 18 |
| Melis et al14 | Yes | Yes | Yes | NR | NA | NR | NR | NR | NA | NR | NA | NR | NR | NR | Poor | 4 |
| Chu et al15 | Yes | Yes | Yes | Yes | NR | NA | NR | NR | NR | NA | Yes | NR | NR | NR | Fair | 13 |
| Laufer et al16 | Yes | Yes | Yes | Yes | Yes | No | Yes | Yes | Yes | Yes | Yes | Yes | NR | NR | Good | 20 |
| Oral et al17 | Yes | Yes | Yes | Yes | NA | NR | NR | NA | NR | NR | Yes | NA | NR | NR | Fair | 2 |
| Darwish et al18 | Yes | Yes | Yes | NR | NR | No | NR | NR | No | No | Yes | NR | NR | No | Poor | 17 |
| Zacharia and O’Neill19 | Yes | No | NR | Yes | NR | NA | NA | NA | NA | NA | Yes | NR | NR | No | Poor | 22 |
| Ferrero et al20 | Yes | Yes | Yes | Yes | NR | NR | NR | NR | NR | NR | Yes | NR | NR | NR | Fair | 22 |
| Camilleri et al21 | Yes | Yes | NA | NR | No | NA | NR | NA | NA | NR | No | NA | NA | NA | Poor | 12 |
| Abbas et al22 | Yes | Yes | Yes | Yes | NA | NR | NR | NR | NR | NA | Yes | NA | NA | NA | Fair | 21 |
| Fawole et al23 | Yes | Yes | NR | Yes | No | NR | NR | NR | NR | NR | Yes | NA | NA | NA | Poor | 20 |
| Ragab et al24 | Yes | Yes | NA | NR | NA | NA | NR | NA | NA | NA | Yes | NA | NR | NA | Poor | 18 |
| Umelo and Manchanda25 | Yes | Yes | Yes | NR | NR | NR | NA | NR | NR | NA | Yes | NR | NR | NR | Poor | 16 |
| Fuldeore and Soliman26 | Yes | Yes | No | Yes | No | NR | NA | NR | NR | NA | No | NA | NA | NA | Poor | 25 |
| Boujenah et al27 | Yes | Yes | NA | Yes | No | No | NA | NA | Yes | No | Yes | NA | NA | NA | Fair | 18 |
| Eisenberg et al28 | Yes | Yes | No | NR | NA | NA | NA | NR | NR | NR | Yes | NA | NA | NR | Poor | 21 |
CD, cannot determine; NA, not applicable; NR, not reported
A meta-analysis was conducted regarding the stage of the disease, diagnostic method, continent and clinical symptoms to estimate the prevalence of endometriosis. The pooled prevalence estimate of endometriosis regardless of the stage of disease, diagnostic method, continent and clinical symptoms was 18 per cent [95% confidence interval (CI): 16-20; Fig. 2]. The prevalence of endometriosis based on the stage of the disease ranged from two per cent (95% CI: 1-4) for stage 4 to 20 per cent (95% CI: 11-28) for stage 1 (Table III).
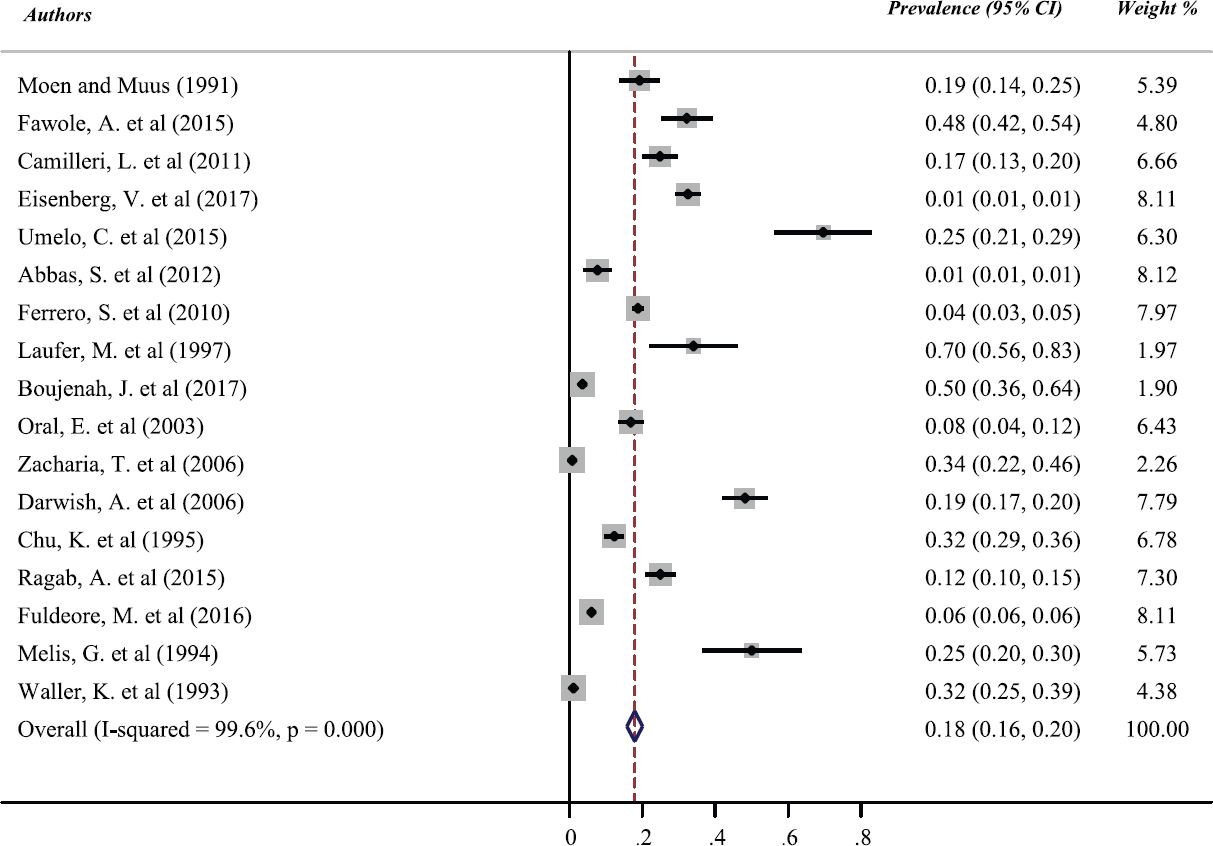
- Pooled prevalence estimate of endometriosis.
| Subgroups | Number of studies | Prevalence estimate (%) (95% CI) | Between subgroups | Between groups | ||
|---|---|---|---|---|---|---|
| I2 (%) | Pheterogeneity | Q | Pheterogeneity | |||
| Stages | ||||||
| 1 | 9 | 20 (11-28) | 99.10 | 0.001 | 16.44 | 0.001 |
| 2 | 8 | 13 (7-18) | 99.60 | 0.001 | ||
| 3 | 7 | 5 (2-8) | 97.00 | 0.001 | ||
| 4 | 5 | 2 (1-4) | 84.30 | 0.001 | ||
| Clinical symptoms | ||||||
| Infertility | 5 | 31 (15-48) | 99.10 | 0.001 | 20.21 | 0.001 |
| Chronic pelvic pain | 4 | 42 (25-58) | 99.20 | 0.001 | ||
| Asymptomatic women | 9 | 23 (19-26) | 99.00 | 0.001 | ||
| Ovarian malignancy | 1 | - | - | - | ||
| Diagnostic method | ||||||
| Laparoscopy | 12 | 20 (17-22) | 99.70 | 0.001 | 13.23 | 0.001 |
| Other (ultrasound or MRI or histopathology) | 3 | 12 (3-21) | 92.80 | 0.001 | ||
| Laparoscopy, ultrasound and MRI | 2 | 31 (25-37) | 96.50 | 0.001 | ||
| Total | 17 | 18 (16-20) | 99.60 | 0.001 | ||
| Continent | ||||||
| Europe | 8 | 17 (12-21) | 98.20 | 0.001 | 17.98 | 0.001 |
| Americas | 3 | 19 (3-36) | 99.60 | 0.001 | ||
| Asia | 3 | 36 (5-69) | 96.10 | 0.001 | ||
| Africa | 3 | 26 (14-38) | 98.20 | 0.001 | ||
| Total | 17 | 18 (16-20) | 99.60 | 0.001 | ||
| Sample size | ||||||
| <1000 | 13 | 28 (19-37) | 99.00 | 0.001 | 19.09 | 0.001 |
| >1000 | 4 | 7 (3-11) | 99.90 | 0.001 | ||
| Total | 17 | 18 (16-20) | 99.60 | 0.001 | ||
*P<0.05. MRI, magnetic resonance imaging; CI, confidence interval
The prevalence of endometriosis by the diagnostic method ranged from 12 per cent (95% CI: 3-21) for endometriosis diagnosed with other diagnostic methods to 20 per cent (95% CI: 17-22) for endometriosis diagnosed with laparoscopic method (Table III). The CI of Egger’s test did not include zero, showing significant publication bias (Fig. 3). Furthermore, high statistical heterogeneity (I2>99%, P<0.001) was identified in total analyses (Table III).
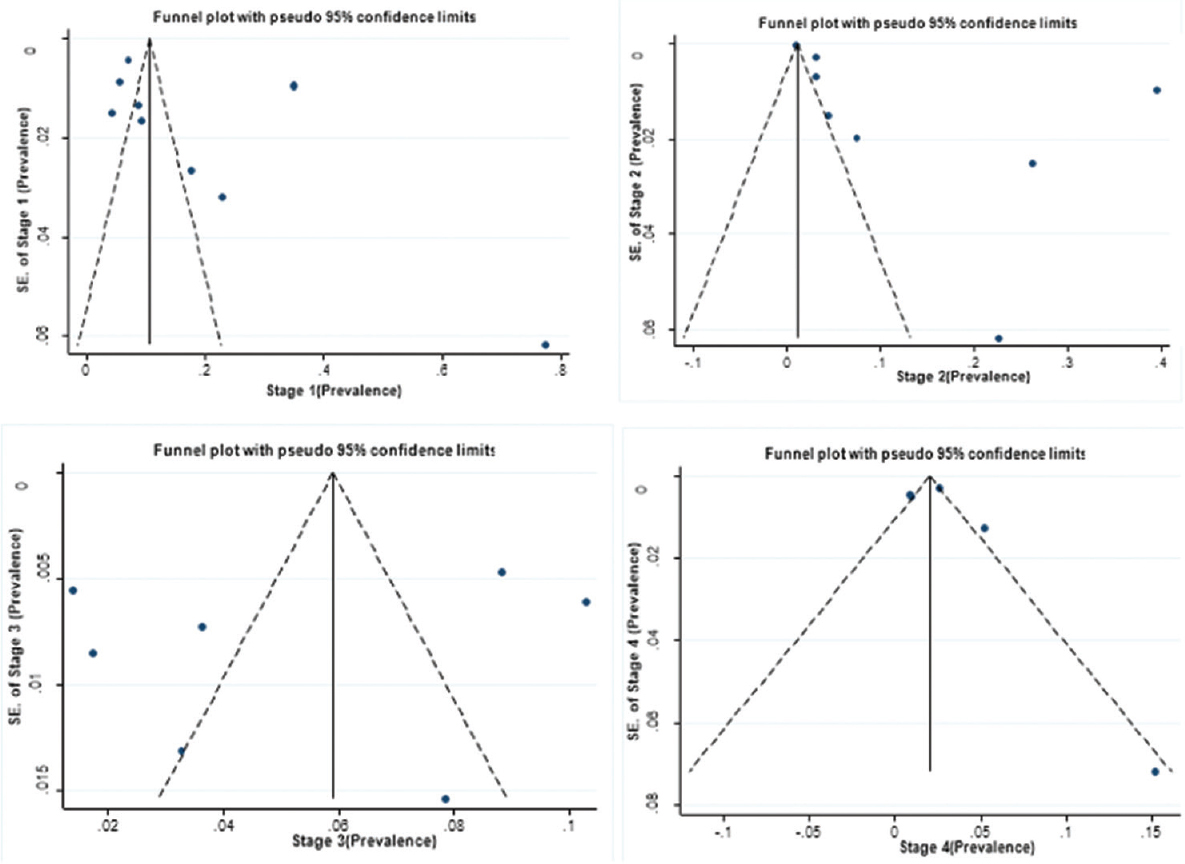
- Funnel plot for pooled prevalence estimate by different stages of endometriosis.
The prevalence of endometriosis by the continent ranged from 17 per cent (95% CI: 12-21) for Europe to 36 per cent (95% CI: 5-69) for Asia, and by the sample size ranged from 28 per cent (95% CI: 19-37) for studies with less than of 1000 individuals to seven per cent (95% CI: 3-11) for studies with more than of 1000 individuals (Table III). The results of subgroup analysis indicated that the prevalence rates of endometriosis in women with infertility, chronic pelvic pain and asymptomatic women were 31 (95% CI: 15-48), 42 (95% CI: 25-58) and 23 per cent (95% CI: 19-26), respectively (Table III).
Meta-regression was used to explore the sources of between-study heterogeneity including age and diagnostic method. According to the results, the prevalence of endometriosis did not show a relationship with age (P>0.10) and diagnostic method (P>0.10).
Discussion
Regarding the stage of endometriosis, the results of this study showed that the prevalence of minimal endometriosis (stage 1) was higher than other stages of endometriosis. Considering the diagnostic method, the prevalence of endometriosis diagnosed with laparoscopy, ultrasound and magnetic resonance imaging (MRI) methods was higher than endometriosis diagnosed with other diagnostic methods in the world. Another study showed the same results30.
The precise prevalence of endometriosis in female adult population is not known. The prevalence in fertile women undergoing sterilization is four per cent (1.5-5%), whereas it is 13.5 per cent (2-68%) in infertile women5. The reported prevalence of this disease in women undergoing laparoscopy for chronic pelvic pain ranged from 15 to 75 per cent6. A study conducted in north India in 2015 showed that the precise prevalence of endometriosis was not known; however, it was estimated to be 2-10 per cent in the general population, but up to 50 per cent in infertile women31.
Endometriosis affects approximately 70 per cent of women with dysmenorrhoea and dyspareunia32. Adolescents may have more severe symptoms. Reports from Germany showed that 0.05, 1.93 and 6.1 per cent of the patients were in the age groups of 10-14, 15-19 and 20-24 yr, respectively333435. A review of previous studies indicated that global estimates varied significantly and ranged from approximately 2-45 per cent based on the diagnostic criteria and the study population35. The world statistics suggest that 10-15 per cent of women in the world are affected by endometriosis, which is consistent with the results of our study, as the overall prevalence was estimated to be 18 per cent35. According to our analysis, the prevalence of endometriosis in developing countries was higher than in developed countries as also shown by another study36.
The present study had several limitations. First, the number of studies in some subgroups was small and did not provide sufficient statistical power to assess the source of heterogeneity. Second, there were some other factors (such as diagnostic accuracy, quality of detective equipment and physicians’ skills in detecting endometriosis) that might be important sources of heterogeneity, but we could not evaluate their role in heterogeneity due to the lack of information. Third, some of the included studies did not measure the variables such as age or prevalence of endometriosis by the stage of the disease.
Despite the high heterogeneity of the studies, this systematic review and meta-analysis showed a high prevalence of endometriosis in developing countries. The prevalence of endometriosis in women with chronic pelvic pain was higher than those with infertility. Future studies are needed to explore factors affecting endometriosis prevalence worldwide, which may help develop future prevention programmes.
Financial support & sponsorship: None.
Conflicts of Interest: None.






