Translate this page into:
Breast conservation surgery & oncoplasty in India – Current scenario
For correspondence: Dr Vani Parmar, Department of Surgical Oncology, Advanced Centre for Treatment Research & Education in Cancer, Tata Memorial Centre & Homi Bhabha National Institute, Kharghar, Navi Mumbai 410 210, Maharashtra, India e-mail: vaniparmar@gmail.com
-
Received: ,
This article was originally published by Wolters Kluwer - Medknow and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Breast cancer incidence is on the rise in India as in rest of the world. While the advances in overall cancer care are at par, the surgical interventions have not been changing at the same pace in India, as in the rest of the developed world. Partly, this is due to the relatively more advanced state of cancer at detection and partly due to lack of awareness resulting in apprehension and slow acceptance of de-escalation of surgical interventions by the treating surgeons, and the beneficiaries, the patients. The article looks at the current scenario, available evidence on the practices and pitfalls with possible solutions for advancing surgical care of breast cancer in India.
Keywords
Breast conservation
current scenario
India
mammoplasty
NACT
oncoplasty
reconstruction
Breast cancer in India
Breast cancer incidence is on the rise in India similar to the global phenomenon. Approximately 164,000 cases of breast cancer are diagnosed in India every year1. The disease has gained a predominantly urban profile with many new cases seen in middle-aged working-class women with urban lifestyles. The incidence-to-mortality ratio for breast cancer is high, possibly attributed to the late-stage disease at presentation, inadequate medical facilities, and also the lack of awareness about disease symptoms, breast self-examination (BSE) and no routine mammographic screening23. Late-stage breast cancer diagnosis with larger tumours results in higher mastectomy rates which aggravates the psychological trauma associated with the diagnosis resulting in depression and loss of self-esteem associated with losing an aesthetic organ and feminity45.
Breast conservation surgery and oncoplasty: The Indian scenario
Breast conservation surgery (BCS) has now become the evidence-based standard of care globally in early breast cancer and also is being offered in some select suitable cases in locally advanced and large operable breast cancer after down-sizing with neo-adjuvant systemic therapy4. Over the last two decades, BCS is being offered increasingly to women in India as well, in women presenting with very early breast cancer, especially in the large cities and metros. The level of public awareness has increased significantly with more and more women being keen on maintaining their body image and understand the importance of completion of relevant treatment protocols and regular follow up.
Breast cancer advocacy in India has evolved rapidly over the last couple of decades, and breast cancer is no longer considered a social stigma and is being discussed more openly in the public forums.
Evolution of breast conservation surgery in India
The interest and transition towards conservative breast surgery started in the 1980s in India and was shown to be safe and feasible in limited resource setting6. With the advent of technology and ease of access to mammography and linear accelerator, there was a concurrent increasing interest and confidence in surgical and radiation oncologists to address the issue. Therefore, BCS began to be offered cautiously, primarily to women with smaller tumours. Conservative breast surgery was carried out initially mostly in larger high volume centres with radiation facility78 and was not so popular among all treating surgeons, who were in majority general surgeons with very few focused breast surgeons. While the West had already started offering breast conservation in nearly 70 per cent women, the rate of breast conservations in most centres in India was variable and accounted for less than 25 per cent cases, with many centres continuing to offer mastectomy even for very early-stage breast cancer9.
With the start of the new millennium, popularity of breast cancer surgery in India showed an upward trend. Research in breast cancer also picked up especially in the larger high volume centres and some of the significant practice changing trials in India started towards the turn of last millennium1011. Breast conservation was evidenced to be safe1213 and offering this as a surgical option was accepted as a norm, albeit with an initial apprehension. This was also a time when the technique of breast conservation was considered oncologically appropriate only if the surgical incision was placed right over the tumour, with no tunnelling, and with cavity being left to heal with seroma accumulation to contour the breast, and no approximation of the walls of excision cavity14.
While multidisciplinary breast units were evolving at the close of the last millennium, vertical division to have focused area of interest in specified areas of oncology by organ-wise division was gaining in popularity. The need for holistic treatment of breast cancer was acknowledged and soon, the focus moved from not just conserving of breast but inclined towards breast reconstruction. Breast cosmesis took on a priority in the necessary end-points while keeping oncological safety as a prerequisite. Quality of life (QOL) had a new meaning in oncological surgery of breast with patient reported outcomes being the qualitative measure of proof of success.
Breast oncoplastic surgery
While the cancer surgeon focuses on radical extirpation of the cancerous tissue along with normal surrounding tissue to ensure negative margins, the plastic procedure helps at the same time to reconstitute the organ functionally and aesthetically. A new consensus definition of oncoplastic surgery was proposed by the American Society of Breast Surgeons as ‘Breast conservation surgery incorporating an oncologic partial mastectomy with ipsilateral defect repair using volume displacement or volume replacement techniques with contralateral symmetry surgery as appropriate15.
Training in oncoplastic breast surgery globally and in India
The term ‘oncoplastic surgery’ is credited to Prof Warner Audrestch from Dusseldorf, Germany16. He made pioneering contribution in refining and popularizing the techniques and training in oncoplastic surgery. He founded in 1990 a dedicated ‘Interdisciplinary Breast Centre – IBC’ in Dusseldorf, Germany, offering training in art of oncoplastic surgery. Since then there have been many surgeons in Europe, UK and US, who have further developed the skill of Oncoplasty and have taken this forward to a different level17.
Oncoplastic breast surgery (OBS) is now an integral part of breast cancer surgery, but only a few surgeons are formally trained in the various techniques. Increasing the availability of OBS necessitates much closer collaboration and cooperation between the breast and plastic surgeons, along with development of new training programmes, new curriculum and new guidelines suited to patient needs and available resources18.
Even though a two surgeon concept for OBS was deemed ideal in the initial phases of OBS uptake in Europe and UK, it became necessary to create a single oncoplastic surgeon to increase the OBS uptake for serving the needs of breast cancer patients. Since the adoption of the one surgeon concept, marked increase in OBS use was reported in the UK19. A similar effect on breast surgical practice influenced by the adoption of oncoplastic procedures by specialist breast surgeons was also reported from New Zealand20. This paradigm raised the quality of OBS being offered and resulted in cost-effectiveness. Similarly, in India, the concept of a single OBS surgeon has been taken up to increase its mainstream acceptance21.
In India, wherein mastectomy still remains the mainstay of cancer treatment in many centres, BCS is now being accepted as standard of care in selected patients by most clinicians. Breast oncoplasty training is now incorporated as an important component of training in advanced certified courses in surgical oncology recognized by regulatory educational bodies.
Nuances of oncoplastic breast surgery
The objectives of OBS are to provide: (i) oncologically safe surgery with complete tumour removal; (ii) surgical restoration of the breast shape and size; and (iii) enhancement of breast cosmesis. OBS can be broadly divided into breast cancer surgery using local parenchymal flaps, mammoplasty techniques or local/remote flaps, and breast reconstruction after mastectomy using internal implants/prosthesis or autologous tissue aided with surgical accessories.
Several studies from the UK, Europe and North America have indicated that OBS is oncologically safe, cost-effective, improves QOL, does not influence the outcomes of post-surgery chemotherapy or radiation and is well-accepted by patients22. Internationally, it is now an established practice to offer OBS to patients as standard surgical care in BC management23. Worldwide, trends in breast cancer management indicate the significant impact of this technique in improving surgical outcomes and improvement in QOL of patients24. However, most of these were based on small treated patients groups and underpowered studies, none of which randomized.
Types of oncoplasty
2. Level II: Especially useful for (i) larger tumours requiring post-excision volume replacement or whole breast reconstruction using perforator based or random flaps or pedicled flaps (Figs 4-6), with or without implants and (ii) larger breasts with reduction mammoplasty technique for volume reduction breast conservation for improved cosmesis and to facilitate radiation therapy postoperatively (Fig. 7).

- J-plasty for lower inner quadrant tumour.

- Grissoti flap for retroareolar tumour.

- Round block technique for excision of upper inner quadrant lump through circumareolar approach.

- Nipple-sacrificing areola-saving whole breast reconstruction (WBR) with extended LD flap; (A and B) preoperative; and (C and D) postoperative.

- Skin saving nipple preserving mastectomy with sentinel node biopsy with silicone implant reconstruction for a multicentric EBC with extensive microcalcification.
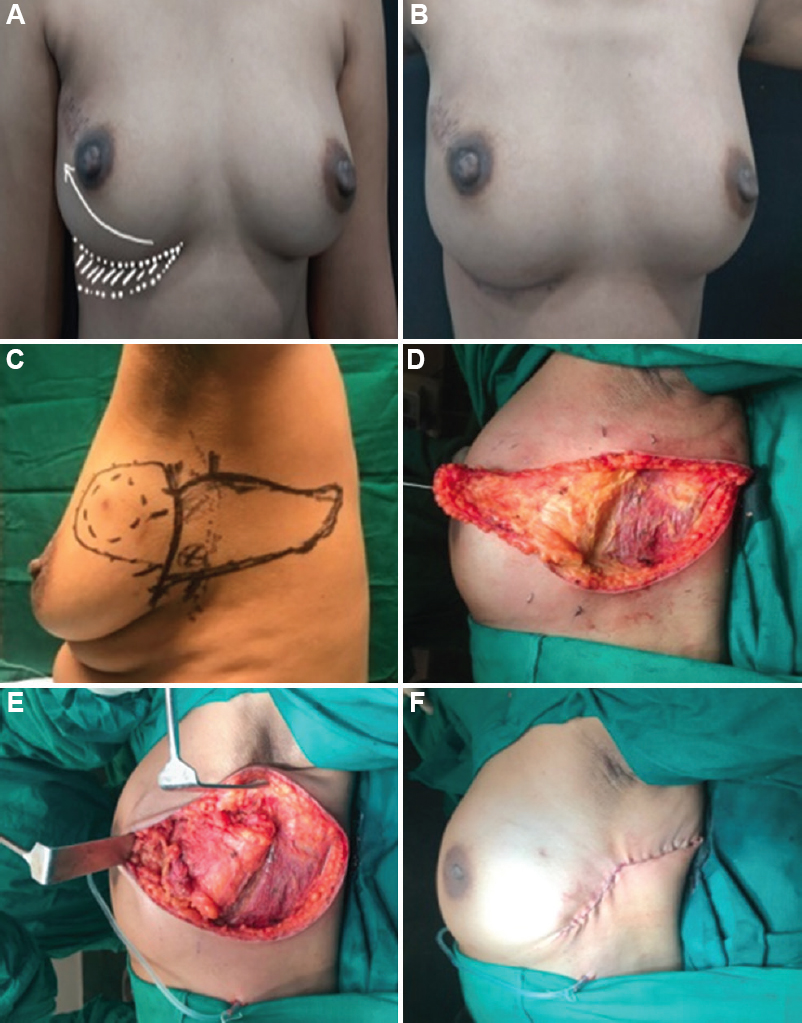
- (A and B) LICAP (anterior branch based) flap from inframammary fold for right breast UOQ volume replacement; and (C-F) LICAP (posterior branch based) flap for left breast UOQ volume replacement.
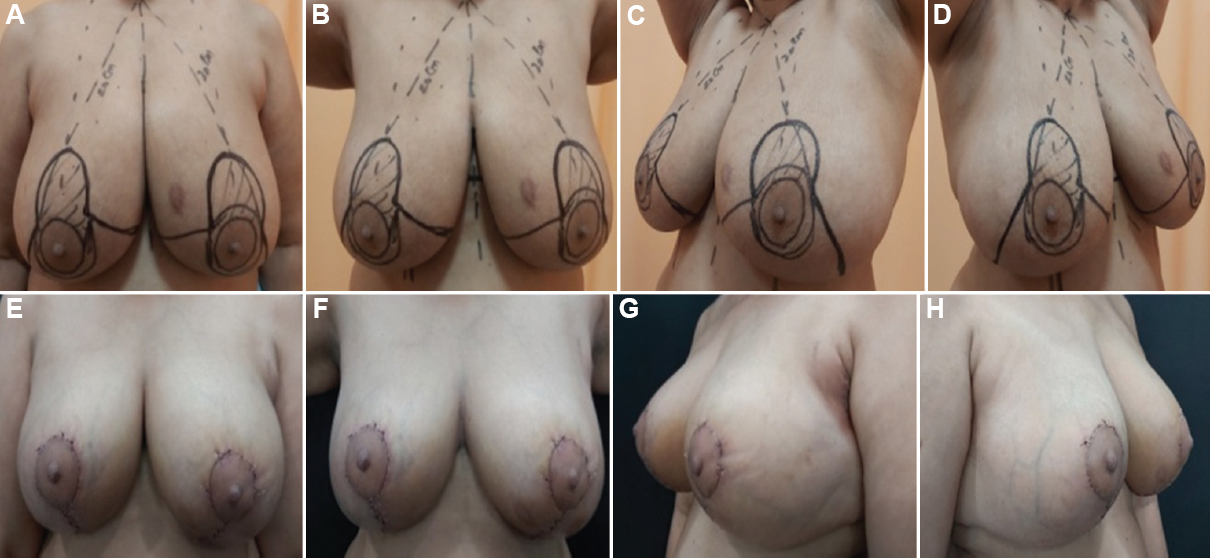
- Bilateral wise-pattern reduction mammoplasty in ptotic breast with superomedial pedicle (left breast lower central primary tumor); (A-D) preoperative; and (E-H) postoperative.
Oncoplastic surgery outcomes in Indian women
Lattissimus dorsi myocutaneous flap
Considering that OBS is still evolving in India, large body of evidence from India on use and application of oncoplastic procedures and their clinical outcomes is not available. Most data are retrospective or from prospectively maintained databases and case series reports. We had previously reported a series of 221 women with 148 early and 73 locally advanced breast cancer25, of whom 146 women were operated post-neo-adjuvant chemotherapy, a volume replacement lattisimus dorsi (LD) flap-based oncoplastic breast reconstruction, performed during 1998−2009. With relatively larger tumours (median 5 cm), these were extended indication for BCS. There was a five per cent positive margin status that was addressed by re-excision of positive margin, all treated by adjuvant radiation therapy. The donor site morbidity was low at 4.9 per cent and recipient morbidity at 1.3 per cent. At a median follow up of 36 months, locoregional recurrence was seen in 4.5 per cent with higher recurrence risk in lympho vascular emboli (LVE) positive and patients with higher axillary nodal burden.
Perforator flaps (PFs)
Perforator flaps (PFs) allow surgery in BC patients with small-to-moderate, non-ptotic breasts for tumours in virtually every quadrant with the use of various types of flaps selected according to the anatomical site of tumours as well as size and volume of the breasts26. Various types of PFs include (i) lateral intercostal artery PF (LICAP), (ii) lateral thoracic artery PF or LTAP, (iii) medial intercostal artery PF (MICAP), (iv) anterior intercostal artery PF (AICAP), (v) thoracoepigastric flap or TE flap.
The choice of these flaps was based on anatomical classifications such as (i) lower LICAP for lower outer quadrant (LOQ) tumours, (ii) LTAP and upper LICAPs for upper outer quadrant (UOQ) tumours, (iii) MICAPs for LOQ and AICAPs for lower inner quadrant (LIQ) tumours.
The breast cancer patients requiring PFs were further classified according to the surgery techniques namely: (i) simple parenchymal replacements (simple replacement of volume); (ii) parenchyma and skin replacements (tissue + skin replacement); and (iii) extreme resections in which reconstruction with PFs was possible (extreme oncoplasty).
Lateral intercostal artery perforator flap (LICAP) and Thoracoepigastric flap (TE): These flaps allow for larger volume replacement and can be either posterior branch based with skin donor area being lateral to posterior back and flap transposed after flipping or propelling into the breast defect, or anterior branch-based with skin donor area being inframammary (Fig. 6). In a series of 41 cases, operated during 2016-2020, with 26 women undergoing upfront oncoplastic surgery with posterior-based LICAP flap and 15 others after down-sizing with neo-adjuvant chemotherapy, with median tumour sizes of 2.9 and 1.5 cm, respectively, a positive cut margin was observed in 7.5 per cent cases with an equal 7.5 per cent incidence of morbidity27. At a median follow up of 14 months, fat necrosis post-RT was slightly high and noted in 10.5 per cent cases. The concern with post-radiation fat necrosis is the clinical suspicion, and at times, radiological features are very similar to a recurrence and it also gets worse as time progresses. This may lead to patient anxiety and clinician’s dilemma resulting in increased diagnostic biopsies. The data are still immature for clinical disease outcomes27.
Therapeutic mammoplasty
Therapeutic mammoplasty (TM) (Fig. 7A-H) has been shown to be a well-established BCS protocol for large ptotic breasts. This procedure applies to medium- to large-sized breasts with a small to relatively larger tumour, allowing for wider excision, combining a breast reduction technique along with mastopexy, thus allowing for BCS. Therapeutic mammoplasty procedures include wise pattern reductions, vertical scar mastopexy, Benelli mammoplasty techniques, Grissoti flap, etc. TM is a safe and acceptable technique for patients with medium to large ptotic breasts with satisfactory oncological outcomes. A retrospective study from the UK compared a cohort of women with unilateral BCS with another set of women who underwent bilateral reduction mammoplasty28. At a three years median follow up, in spite of large tumour size, rate of axillary dissection, adjuvant chemotherapy and tumour bed boost in mammoplasty group, the surgical complications were not significantly different, with lower re-excision rates in TM (P<0.05). Despite poorer prognostic factors, TM group reported better satisfaction and physical functioning and fewer adverse effects of radiotherapy. Extreme oncoplasty, as therapeutic mammoplasty is also referred to, can also be used in some multifocal tumours to avoid a mastectomy and allow for breast conservation without compromising oncological outcomes or cosmesis with high patient satisfaction29.
Oncoplasty post-neoadjuvant chemotherapy
With comparable survivals, BCS in the primary setting scores over mastectomy with better patient satisfaction and outcomes. Neo-adjuvant chemotherapy (NACT) for tumour downsizing followed by BCS is integral to clinical management of LABC/LOBCs although without level I evidence. Some level III evidence is available for post-NACT breast conservation and partial breast reconstruction with LD flap425. Post-NACT downsizing should increase BCS rates considerably30 but may not be feasible in all cases. The authors concluded that there was a need to standardize and establish appropriate protocols for tumour imaging during NACT, accurate pre-surgery tumor localization, good Radiology-Pathology (Rad/Path analyses of the excised specimens and effective RT techniques30. Internationally, concerns have been raised about the safety of post-NACT BCT in the Early Breast Cancer Trialists’ Group (EBCTCG) overview even though other reviews have suggested safety of this procedure31. In the EBCTCG overview, the overall conversion from mastectomy to breast conservation was only 40 per cent.
Regarding safety of OBS post-NACT, in our previous study the retrospective audit in 146 women who underwent a LD reconstruction post-NACT showed a two per cent locoregional recurrence rate at a single tertiary cancer centre25. It is known that traditional tumour localization at the time of biopsy may not always be accurate at the time of surgery for the large tumours that require NACT, with inherent risk of clip migration. This problem can be mitigated by considering clip insertion mid-NACT. Patients can be examined with an ultrasound examination USG every two to three cycles and tumours that responded well to NACT can be localized by clip insertion when tumour reduces to about 1 cm in size. Residual calcification extending across a large area may be wire-localized pre-operatively. Surgery plans are determined on the basis of residual tumour size, location, breast size and shape, axillary node status and patient choice.
The oncoplastic surgeries that can be offered post-NACT cover a wide variety of techniques, from traditional simple oncoplastic parenchymal mobilization and closure, Grissoti flap, therapeutic mammoplasty to extreme therapeutic mammoplasty and PFs. Oncoplastic surgeries have significantly bigger excisions and wider margins. Node clearance is managed as per the standard guidelines with axillary clearance. Of course, a longer follow up is required in these selective patients to completely understand the safety of offering oncoplasty for these residual tumours. Radiation protocols in such cases are still being streamlined. A 1:2 case-control study from Brazil32 reported that the outcomes between standard BCS after neo-adjuvant chemotherapy (controls) versus oncoplastic BCS (cases) at 67 months follow up had no difference in local and locoregional recurrences. The reported pathological complete response (pCR) was 26.9 per cent, 19.2 per cent patients died of progression and overall survival (OS) at 60 months was 81.7 per cent. These were T3 tumours, with average size of 5.25 cm and 85 per cent were larger than 3 cm.
Thus, increase in BCS rates can be achieved by carefully using various oncoplastic techniques post-NACT following a rigid effective protocol of imaging, accurate tumour localization and appropriate intra-operative assessment. Tumours must be excised with care ensuring negative margins with an intra-operative rad/path analyses and by employing appropriate RT techniques to prevent local recurrences. With these precautions, NACT-guided oncoplastic BCS can be oncologically safe and well accepted by patients.
Breast reconstruction
In OBS, total mastectomy followed by one- or two-stage breast reconstruction either with the help of a breast implant or autologous tissue (LD or DIEP flap) is the standard practice. Breast reconstruction improves QOL, overcomes mastectomy-associated depression and provided better self-esteem and femininity33. Implant-based immediate breast reconstruction (IBR) is more popular as it improves cosmesis, requires single-step surgery, shorter recovery time and is cost-effective since both oncosurgery and reconstruction are performed by a single oncoplastic breast surgeon34. The acceptance of implant-based IBR is poor (~15%) in India which can be improved by (i) wider acceptance of the ‘one oncoplastic surgeon–dual role’ model in which one surgeon performs oncosurgery as well as plastic surgery; (ii) surgical cost-reduction by innovative techniques to obviate need of acellular dermal matrix or ADMs, such as by dermal ‘sling surgery’; and (iii) creating affordable breast reconstruction packages which can absorb the implant cost.
Sling surgery for breast reconstruction
The lower dermal autologous sling is a natural accessory to breast implant reconstruction and is oncologically safe, has a low complication rate, produces good to excellent cosmetic results and improves patient satisfaction3536. Most importantly, it reduces RT-induced complications thus suggesting a protective effective covering for the breast implant in the lower outer aspect where pectoralis major muscle does not cover the implant in subpectoral placement. The use of sling tissue may possibly obviate the need for ADMs in implant-based reconstructions which are so commonly used in the West but are inaccessible and cost-prohibitive in India.
In small non-ptotic breast one-stage breast reconstruction with breast implants is feasible if aided by such novel surgical modification that employs autologous lower dermal skin (ALDS)-derived lower abdominal/thoracic skin. Surgically challenging non-ptotic/small breasts can be successfully reconstructed using implants with oncological safety, better cosmesis and protection from RT-related complications without the need of ADMs using this technique.
Conclusion
Oncoplastic surgery is slowly becoming the accepted standard of care in India with early breast cancer. The evolution has taken a little longer than the West but is slowly heading in the same direction and mastectomy would soon become the limited procedure being offered selectively where breast conservation or oncoplasty cannot be offered for technical reasons. Long term safety outcomes still need to be generated from Indian patients as the disease panorama here is different from the West and that is why proper selection of cases is important so as not to harm the patient for the sake of good cosmesis alone. Patients with locally advanced breast cancer may not be the right candidates for oncoplastic surgery unless the radicality of excision is well taken care of and oncological safety is not compromised in any way.
Acknowledgments:
Authors acknowledge Drs Devaki Kelkar and Nutan Gangurde from Prashanti Cancer Care Mission for contribution to the breast oncoplasty research work. Authors thank Drs Nita S. Nair and Shalaka Joshi for having shared some of their clinical data and images on patients where oncoplasty was offered.
Financial support & sponsorship: None.
Conflicts of Interest: None.






