Translate this page into:
Health system preparedness & community participation in Japanese encephalitis/acute encephalitis syndrome (JE/AES) prevention in a tribal district of Odisha, India
For correspondence: Dr Debdutta Bhattacharya, Department of Microbiology, ICMR-Regional Medical Research Centre, Chandrasekharpur, Bhubaneswar 751 023, Odisha, India e-mail: drdebduttab.rmrc-od@gov.in
-
Received: ,
This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
This article was originally published by Wolters Kluwer - Medknow and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Background & Objectives:
Japanese encephalitis/acute encephalitis syndrome (JE/AES) is one of the major zoonotic arbodiseases that has a significant effect on human and animal health. Though many studies have been published on the epidemiology and transmission mechanisms of JE/AES, but there is little evidence on health system preparedness, including community-based engagement. This study was undertaken to explore a multi-stakeholder perspective on health system preparedness for the prevention of JE/AES in a tribal district of Odisha, India.
Methods:
This study was conducted at Malkangiri district of Odisha. A total of nine focus group discussions (FGDs) among women having under-five children, community volunteers, and community health workers (CHWs), and 20 in-depth-interviews (IDIs) among community leaders, healthcare providers, and programme managers were conducted. The FGDs and IDIs were digitally recorded, transcribed, translated and analysed using content analysis approach.
Results:
Health system preparedness for the prevention of JE/AES was improved, including effective vector management, implementation of the surveillance system, and vaccination programme. The JE vaccine was introduced under Universal Immunization Programme in Odisha in 2016. Behavioural Change Communication activities were provided with the support of community volunteers on Village Health Nutrition and Sanitation Day (VHNSD) under Gaon Kalyan Samiti (GKS) platforms. The CHWs were actively involved in vector management and raising sanitation and hygiene awareness.
Interpretation & conclusions:
Community participation and coordination between different stakeholders have a significant impact on the successful implementation of the programme. It was suggested that there was a need for a sustainability approach to active participation, orientation and capacity building training among CHWs and community volunteers to successfully implement the programme.
Keywords
Acute encephalitis syndrome
health system
Japanese encephalitis
preparedness
vector management
zoonotic
The Japanese encephalitis/acute encephalitis syndrome (JE/AES) is one of the major zoonotic arboinfections1. It has a serious impact on human and/or animal health in endemic regions123. Globally, there are above two billion people living in endemic regions who are at risk with most having mild to moderate symptoms3;predominantly, children between 0 to 14 years develop encephalitis, with approximately 50 to 175 thousand cases per year in which almost one-third are fatal and the rest suffer from post-infectious neurological deficits3.
Globalization and extreme weather events have shown a significant effect on the spread of vector-borne diseases across the globe45. Human JE/AES infections have been documented primarily in temperate, subtropical and tropical regions of Asia and northern Australia123. The situation in India is aggravated by its diverse geographical and socio-behavioural environment, including rapid population growth6. Therefore, it is important to understand the transmission mechanisms and control strategies.
Many studies from India reported on epidemiology, molecular epidemiology, transmission mechanisms, pathways and other aspects of JE/AES78910. However, there is little information on the health system preparedness focusing on community-based participation for the prevention. Preparedness of the health system, including healthcare institutions, and collaborative preparedness between curative health institutions and public health services are crucial for outbreaks prevention11. This study was conducted to explore a multi-stakeholder perspective on the health system preparedness for the prevention of JE/AES in a tribal district of Odisha, India.
Material & Methods
A qualitative exploratory study was conducted in the Malkangiri district of Odisha, India in 2019. The district covers an area of 5,791 square kilometers with seven administrative blocks, and nearly 76 per cent of area is covered with dense forests and mountains. The district has a subtropical climate with monsoon lasting from the last week of May to October. The district is sparsely populated with a population density of 106 per square kilometer inhabited by primitive tribes – Bondas, Koyas, Porajas, and Didayis; half of the population are tribal with 48 per cent literacy rate. Agriculture and animal husbandry are the main sources of livelihood. The district was selected based on the frequency of outbreaks of JE12. The mapping of programmatic data available from the National Vector Borne Disease Control Programme (NVBDCP) showed the spread of JE/AES in the Malkangiri district (Figure).
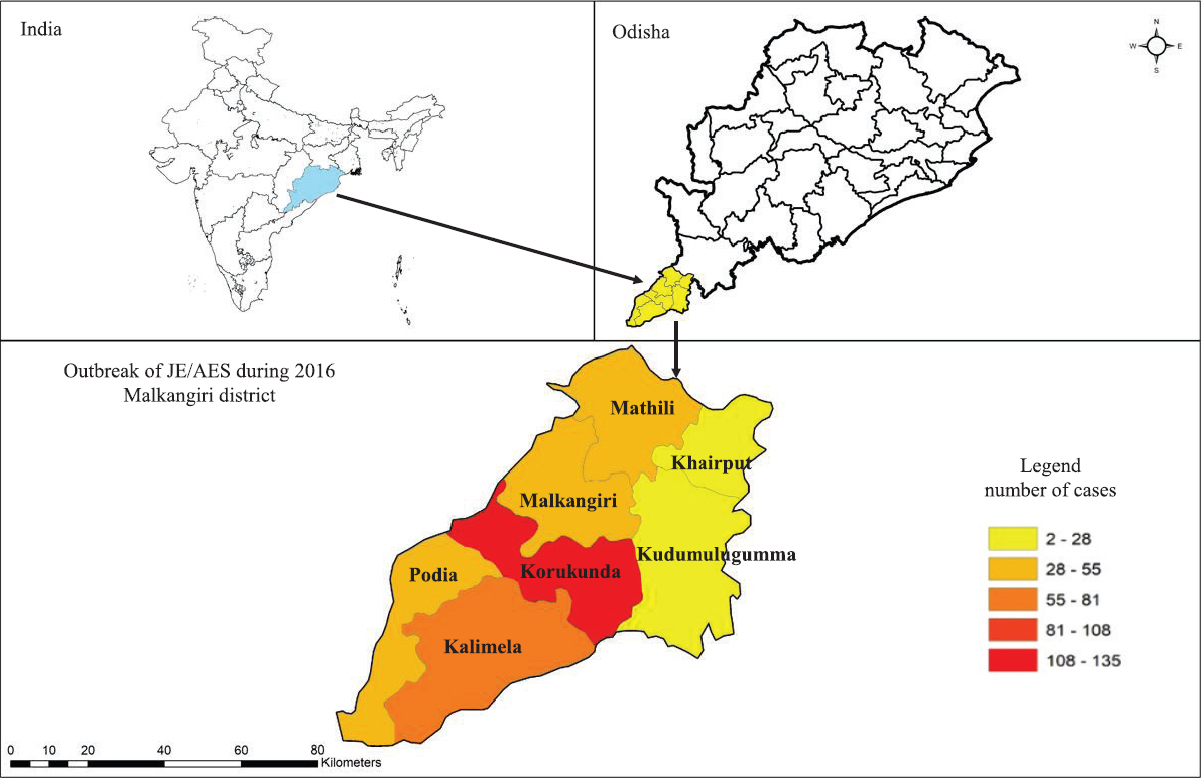
- Mapping of Japanese encephalitis/acute encephalitis syndrome outbreak in Malkangiri district during 2016. Source: National Vector Borne Disease Control Programme; State Task Force cum review meeting for Odisha. Map generated in QGIS version 3.8.
Study participants and data collection procedure: This study was carried out among women with children under five, community volunteers, community health workers, medical officers, and programme managers. The technique of stakeholder mapping was adopted for selecting study participants using purposive sampling method. In-depth interviews (IDIs) and focus group discussions (FGDs) were used to collect the data. A total of nine FGDs were carried out, three each among women with under-five age group children, community volunteers (i.e., members of women self-help groups), and frontline healthcare providers [i.e. Anganwadi workers (AWWs), accredited social health activists (ASHAs), and auxiliary nurse midwifery (ANMs)]. Twenty IDIs were conducted, eight among community leaders, i.e. ward members and village head, eight among healthcare providers from different levels of healthcare facilities: primary, secondary and tertiary, and four healthcare programme managers. FGDs and IDIs were conducted using a semi-structured guide in the local language. Ethical clearance was received from the ethical committee of ICMR-Regional Medical Research Center, Bhubaneswar. Written informed consent was taken from all participants before data collection.
Data management and analysis: FGDs and IDIs were digitally recorded, transcribed verbatim, and translated into the English language. The average duration of the FGDs was 40 (range 15-60) minutes and that of the IDIs was 25 (range 15-40) minutes. Content analysis was used for data analysis13. Major units were identified from the original transcripts relevant to the study objective. Then the units were condensed and coded. The related codes were divided into groups, collectively. Finally, the main theme was articulated based on categories.
Results
Three major themes emerged were: (i) epidemiology and outbreak investigation mechanisms (Suppl Table I); (ii) health system preparedness (Suppl Table II); and (iii) community participatory mechanisms (Suppl Table III). The content of each theme was represented with major categories and quotes from the participants.
| Categories | Epidemiological history, disease distribution, and perceived risk factor | Containments of outbreaks |
|---|---|---|
| Codes | Alternate years pattern | Perplexity between JE and AES |
| 184 hotspot villages | Standard treatment protocol | |
| Koya tribe | Nutritional support at the facility | |
| Half-baked Cassia occidentalis consumption | Primary case management by CHWs | |
| High mosquito density | 90% JE positive pigs | |
| Practice of pig rearing | Isolation of pigs |
JE, Japenese encephalitis; AES, acute encephalitis syndrome; CHWs, community health workers
| Categories | Surveillance system | Introduction of vaccination | Vector control mechanisms |
|---|---|---|---|
| Codes | Integrated Disease Surveillance Programme (IDSP) | 2017- National Immunization Programme | Long-lasting insecticide nets (LLNs) distribution |
| Weekly reporting | Endemic districts | Indoor residual spraying | |
| Standard format | Two doses | Fogging | |
| Treatment at District Headquarter Hospital | Mass vaccination campaign | BTI spraying | |
| Major symptoms- hypogylcaemia and malaria negative | Target: 0-15 years | Peri-domestic measures | |
| Household surveys | Integrated vector | ||
| Cerebrospinal fluid biomarker analysis | Supervision team | Management strategy | |
| ELISA | Community awareness campaigns | ||
| Reference laboratory | Tracking of left - outs | ||
| Reduction in cases | Departmental coordination |
| Categories | Community understanding on risk factors and perceived barriers for healthcare | Behavioral change communication strategies | Participation of community health workers and community volunteers |
|---|---|---|---|
| Codes | Common term: pig fever or Japenese fever | Integral part of prevention | Primary treatment |
| Poor hygiene | Community volunteers | Awareness activities | |
| Host- aquatic and domestic animals | VHSND and Gram Kalian Samiti meetings | Referral to DHH | |
| Sanitation as best measure | High workload in hospital and laboratories | ||
| Provision for pig shelters | Pamphlets distribution | ||
| Village health sanitation and nutrition day meetings | Debate in schools | Weekly reporting | |
| Behavior change monitoring by ASHA | Limited orientation on health issues | ||
| Lack of trust in public health facilities | No provision of Audio visuals aids | ||
| Out-of-pocket expenditure | Proper waste disposal | Self-help groups |
DHH, District Headquarter Hospital; VHSND, village health nutrition and sanitation day; ASHA, accredited social health activists
Theme 1: Epidemiology and outbreak investigation mechanisms
Epidemiological history, disease distribution, and perceived risk factors: In Malkangiri district in 2016, cases of JE/AES were found in 184 hot-spot villages. Cases were usually reported during monsoon and post-monsoon periods (September to November). The medical officers explained that the majority of cases involved were children between one and five years of age with common symptoms like fever, vomiting, sudden onset of convulsions and hypoglycaemia.
According to the medical officer, JE/AES outbreaks were first observed in the Korkunda block; however, there more number of cases were seen in the Kalimela block. Although it had spread to all communities, but the Koya tribe was mostly affected. The medical officers perceived that one of the risk factors for the outbreak of AES was the consumption of half-baked Cassia occidentalis seeds among tribal communities, while poor sanitation, high mosquito density and pig rearing were the other possible reasons for a greater risk of disease in the tribal population.
Containments of outbreaks: The interviewees noted that the difference between the cases of JE/AES was perplexed due to similarity in clinical presentation. A standard operating procedure for timely referral of cases and appropriate treatment was followed. At the peripheral level, community health workers were provided with all the essentials required for primary case management and the identified cases were referred to the district hospital for further treatment. All the pigs in the region were isolated during outbreaks with the help of the veterinary department.
Theme 2: Health system preparedness
Surveillance system: Respondents described that information about JE/AES under Integrated Disease Surveillance Programme (IDSP) was routinely collected over the last decade. The data were collected weekly in endemic districts using a predesigned standard format developed on the basis of suspected symptoms which were submitted by the CHWs. Simultaneously, patients were referred to the primary health care facilities for treatment; if primary health providers observed hyperthermia, hypoglycaemia and serum negative for malaria, immediately they were referred to higher facilities. Respondents reported that all cases were treated at the District Headquarters Hospital; samples were taken from suspected cases for serological tests. The samples were also sent for confirmation to the Regional Medical Research Center, Bhubaneswar or Manipal Center for Virus Research (MCVR), Karnataka, as a reference laboratory.
According to the healthcare providers, there was a shortage of staff in health facilities to manage the outbreak. Paediatricians and community medicine specialists from the nearest medical college, supported during the outbreak. Patients who reported to primary healthcare facilities were also counselled by physicians and referred to tertiary health care facilities for treatment. Many family caregivers perceived that there was a help-desk in the healthcare facility during the outbreak to assist them in their admission, diagnosis and prompt treatment.
Introduction of vaccination: The respondents stated that earlier, JE vaccine was not a part of the routine immunization schedule. However, following the outbreak of AES, JE vaccine was introduced as a part of the routine immunization programme in 2017 in the endemic districts of Odisha. To prevent outbreaks, a mass vaccination campaign along with community awareness campaign was conducted in endemic districts among children aged 1-15 years. ASHAs, AWWs, ANMs and school teachers were trained to conduct household surveys to count vaccine recipients under the supervision team.
One of the challenges described by the participants was the transport of vaccines to remote areas due to poor road connectivity. The other challenge was the lack of accommodation facilities for the staff during mass-vaccination.
Vector control mechanisms: The participants reported that various vector control measures were used at the community level to control outbreaks, such as the distribution of long-lasting insecticide mosquito nets (LLNs), indoor residual spraying, fogging, cutting of Cassia plant bushes, Bacillus thuringiensis serotype israelensis (BTI) spray in the rice field to control mosquito bites.
Theme 3: Community participatory mechanisms
Community understanding of risk factors and perceived barriers for healthcare: The most common term used for JE in the community was ‘pig fever or Japanese fever or foreign fever’. The majority of the community members pointed out that it was caused by mosquito bites or by pigs. A few community members also mentioned poor hygiene and consumption of Cassia occidentalis seeds as a risk factor for JE fever. Most participants were aware of JE symptoms viz., vomiting, diarrhoea and fever among children. Many participants were aware of the prevention strategies for JE infection. They referred to the use of mosquito nets, wearing of full sleeves clothing, and cleanliness as measures to prevent JE infection. They also proposed the provision of shelters for the rearing of pigs to maintain distances between community members and animals.
Medical officers pointed out that the lack of trust among community members in public health facilities was a challenge. Patients were identified by active case search and taken to the hospital for treatment. One of the barriers encountered by a community member was the lack of ambulance services, particularly in hilly regions. They also mentioned an increase in the out-of-pocket expenditure on treatment and referral, which was not borne by all the families of the villages. Poor road connectivity was another challenge raised by the respondents.
Behavioural change communication (BCC) strategies: Behavioural change communication activities were carried out in the affected JE districts with the support of community volunteers. The Village Health Nutrition and Sanitation Day (VHNSD) and Gram Kalian Samiti (GKS) meetings were the best platforms for raising awareness among villagers. In addition, CHWs were assigned the responsibility to monitor the use of impregnated nets in households and maintaining distance from pigs.
ASHAs and school-teachers were key players involved in ground-level awareness-raising activities. The ASHA workers pointed out that audio-visual aid was the most effective and sustainable means of information, education and communication; but they were not provided to them.
Participation of community health workers and community volunteers: Most CHWs and community volunteers had some knowledge of JE. They reported on various activities they were engaged in during the outbreak, such as active case search, referral of patients, and community awareness activities.
One of the major challenges expressed by the respondents was the lack of manpower; a few felt that peripheral health centers were not sufficiently equipped. Some of them, however, perceived that health workers at the peripheral level were not trained to deal with cases. They also mentioned three main barriers: one of these was poor information, education and communication (IEC) training activities, the other barriers were limited orientation on health issues, and field visits to hilly areas.
Self-help groups (SHGs) are a robust instrument for promoting effective community participation. They perceived that, as they were not from the medical field, their role during the outbreak was limited to raising awareness among villagers. They were also assigned the duty to close the potholes and to isolate the pigs at a distance of three kilometers from the village.
Discussion
The JE/AES is one of the important public health problems affecting the paediatric population in many parts of north and north-eastern India1415161718. Odisha State reported the first JE outbreak during 1989 followed by seasonal sporadic cases in different parts and major outbreaks in Malkangiri in 2012 and 2016714. Previous studies have shown that wading and water birds are natural hosts and carriers of JE; and Culex and Aedes mosquitoes transfer JE between birds and other species, including humans in temperate regions123.
The World Health Organization has recommended standards guidelines for the introduction or enhancement of surveillance systems19. The JE/AES surveillance has been developed since 2006-2007 by the Government of India2021. The JE vaccination was implemented in the Universal Immunization Programme (UIP) during 201122. In India JE vaccine was implemented in routine immunization under UPI in 181 endemic districts2223. Previous studies in India have shown that addressing community misconceptions about vaccination is essential to improve coverage2224.
The JE emergence involves a complex interplay of vectors, hosts, and the environment, including human behaviour, such as close contact with animals, particularly pigs, and poor hygiene and sanitation practices2456789. Considering to stay indoors during day time to avoid mosquitoes should be advised during outbreaks25. Research and policy in some Asian countries have encapsulated the ‘One Health’ principle of ensuring optimal protection for humans, animals and the environment2526. The previous studies emphasized the need for an integrated multi-pronged approach on vector control, hygiene and sanitation among tribal populations with inter-departmental cooperation to prevent outbreaks272829. Our findings suggest the need for periodic orientation and training among healthcare providers in endemic districts.
Although this study was conducted in Odisha, the findings might be useful for any similar context. The major limitation of this study was that only the mothers’ perceptions was explored, and the fathers and other male family members were not taken into account.
In conclusion, with the effective efforts from the health system towards prompt response and implementation of control measures including vaccination, surveillance, vector control, and public awareness programmes, JE/AES cases may be prevented. Community-participation and coordination between different stakeholders have a significant impact on the successful implementation of the programme.
Acknowledgment:
The authors acknowledge all State, district and block level officers for their technical support, and also thank all the study participants for their participation.
Financial support & sponsorship: The study was funded by the Indian Council of Medical Research, New Delhi, India [Special grant JE/AES (Project No. 228); (VIR/AES/2/2017/ECD-1)].
Conflicts of Interest: None.
References
- Review of emerging Japanese encephalitis virus: new aspects and concepts about entry into the brain and inter-cellular spreading. Pathogens. 2019;8:111.
- [Google Scholar]
- Estimated global incidence of Japanese encephalitis: a systematic review. Bull World Health Organ. 2011;89:766-74.
- [Google Scholar]
- Serological evidence of Japanese encephalitis virus circulation in Asian children from dengue-endemic countries. J Infect Dis. 2019;219:375-81.
- [Google Scholar]
- Climate change: an enduring challenge for vector-borne disease prevention and control. Nature Immunol. 2020;21:479-83.
- [Google Scholar]
- How complex travel, tourism, and transportation networks influence infectious disease movement in a borderless world. In: Handbook of Globalisation and Tourism. Cheltenham, UK, Northampton, MA, USA: Edward Elgar Publishing; 2019. p. :76-88.
- [Google Scholar]
- Emerging/re-emerging viral diseases & new viruses on the Indian horizon. Indian J Med Res. 2019;149:447-67.
- [Google Scholar]
- Japanese encephalitis: a review of the Indian perspective. Braz J Infect Dis. 2012;16:564-73.
- [Google Scholar]
- Epidemiology of acute encephalitis syndrome in India: Changing paradigm and implication for control. J Commun Dis. 2014;46:4-11.
- [Google Scholar]
- Role of integrated vector management for prevention and control of Japanese encephalitis/acute encephalitis syndrome (JE/AES)–a review. J Commun Dis. 2014;46:93-108.
- [Google Scholar]
- Responding to the challenge of acute encephalitis syndrome JE in India. J Commun Dis. 2014;46:1-3.
- [Google Scholar]
- Qualitative research: Institutional preparedness during threats of infectious disease outbreaks. Bio Med Res Int 2020 doi.org/10.1155/2020/5861894
- [Google Scholar]
- Entomological investigation of Japanese encephalitis outbreak in Malkangiri district of Odisha state, India. Mem Inst Oswaldo Cruz. 2018;113:e170499.
- [Google Scholar]
- How to plan and perform a qualitative study using content analysis. Nursing Plus Open. 2016;2:8-14.
- [Google Scholar]
- Japanese Encephalitis: A brief review on Indian perspectives. Open Virol J. 2018;12:121-30.
- [Google Scholar]
- Encephalitis outbreaks in India: A cluttered landscape. Pediatric Infect Dis. 2015;7:89.
- [Google Scholar]
- Japanese encephalitis epidemiology in Arunachal Pradesh, a hilly state in northeast India. Asian Pacific J Trop Dis. 2011;1:119-22.
- [Google Scholar]
- Japanese encephalitis in Assam, India: need to increase healthcare Workers’ understanding to improve health care. PLoS One. 2015;10:e0135767.
- [Google Scholar]
- Epidemiological report on acute encephalitis syndrome (AES)/Japanese Encephalitis (JE) outbreak in Bihar & planning perspectives for its control. American J Health Res. 2014;2:404-10.
- [Google Scholar]
- Evidence and rationale for the World Health Organization recommended standards for Japanese encephalitis surveillance. BMC Infect Dis. 2009;9:214.
- [Google Scholar]
- Directorate of National Vector Borne Diseases Control Programmeme. Guidelines for surveillance of acute encephalitis syndrome (with special reference to Japanese encephalitis). Available from: https://nvbdcp.gov.in/Doc/AES%20guidelines.pdf
- Acute encephalitis syndrome surveillance, Kushinagar District, Uttar Pradesh, India, 2011–2012. Emerg Infect Dis. 2013;19:1361.
- [Google Scholar]
- Coverage & missed opportunity for Japanese encephalitis vaccine, Gorakhpur division, Uttar Pradesh, India, 2015: implications for Japanese encephalitis control. Indian J Med Res. 2017;145:63-9.
- [Google Scholar]
- Vaccination policy for Japanese encephalitis in India: Tread caution! Indian. Pediatr. 2015;52:837-9.
- [Google Scholar]
- Changes in acute encephalitis syndrome incidence after introduction of Japanese encephalitis vaccine in a region of India. J Infect. 2014;69:200-2.
- [Google Scholar]
- Japanese encephalitis: on the One Health agenda. Curr Top Microbiol Immunol. 2013;365:205-47.
- [Google Scholar]
- Inter-ministerial convergence towards prevention and control of Japanese encephalitis and acute encephalitis syndrome (JE/AES)–an integrated multi-pronged public health approach. J Commun Dis. 2014;46:128-34.
- [Google Scholar]
- Understanding parental perspectives on outcomes following paediatric encephalitis: A qualitative study. PloS One. 2019;14:e0220042.
- [Google Scholar]
- Perceptions, practices and health seeking behaviour constrain JE/AES interventions in high endemic district of North India. BMC Public Health. 2017;17:1-2.
- [Google Scholar]
- Acute Encephalitis Syndrome Surveillance: Challenges and the way forward. J Commun Dis. 2014;46:73-85.
- [Google Scholar]






