Translate this page into:
Addressing challenge of zoonotic diseases through One Health approach
-
Received: ,
This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
This article was originally published by Wolters Kluwer - Medknow and was migrated to Scientific Scholar after the change of Publisher.
COVID-19 pandemic has reiterated the need for urgent, systematic, concrete and multisectoral actions to prevent, control and mitigate impact of infections that have been, and shall continue to arise from animals. Human-animal interaction is essential for survival and cannot be eliminated in foreseeable future thus facilitating zoonoses. In developing countries, especially the rural population has a greater, co-habitation of humans with the animals. Higher prevalence of zoonoses in these countries is a testimony to this inextricable relationship.
The ever-increasing proximity to wildlife due to land use changes, illegal trade in wildlife and other economic activities makes it conducive for pathogens circulating in wildlife to come closer to peri-domestic areas and infect animals and humans in these settings1. Such animal-human interface poses the potential to cause outbreaks due to novel pathogens. Unless detected and contained during early phase, a small outbreak can progress into an epidemic or even public health emergency of international concern (PHEIC), finally culminating into a pandemic2. Global impact of these PHEICs has been severely felt3 during the current millennium (Figure) thus not only halting but reversing the gains made in human development and alleviation of poverty.
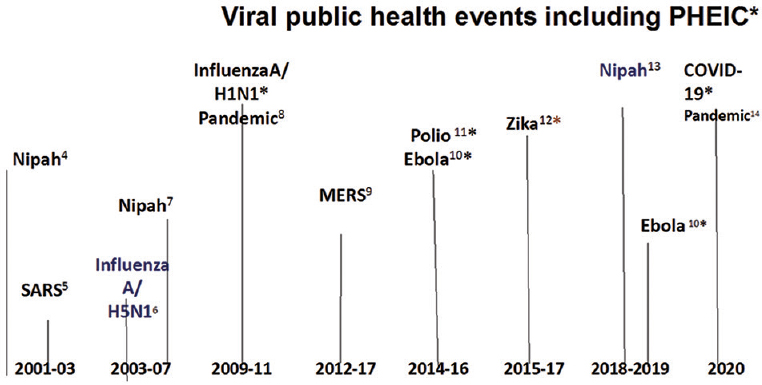
- Major public health events including PHEIC and pandemics during current millennium. Superscript numerals represent reference numbers. SARS: Severe Acute Respiratory Syndrome; MERS: Middle East Respiratory Syndrome, COVID-19: Coronavirus Disease of 2019. *Declared as Public Health emergencies of International Concern by WHO3.
The Figure shows that since 2001 almost every third year a major public health event has occurred, six of these were declared by the World Health Organization (WHO) as the PHEIC3 in accordance with the International Health Regulations (2005)1. Most of these events were caused by the pathogens that originated from animals. It is obvious that these events will continue to occur frequently in the future and the causative agents will arise from animals. Wildlife shall be a perpetual source of microorganisms for which humanity is immunologically naive. It is estimated that more than 850,000 viruses are lurking in the wildlife, of which 20,000 are coronaviruses15.
The diseases of animal origin are multidimensional. Zoonoses are endemic (leptospirosis, rabies, hydatidosis, taeniasis, KFD) and epidemic-prone (Japanese encephalitis, plague, Nipah, avian flu, MERS). Food-borne pathogens (Salmonella, Staphylococcus aureus, Campylobacter, E. coli), PHEIC and pandemics (influenza, SARS, COVID-19, Zika) and their causative agents can also be used to deliberately harm the human health (agents for bioterrorism or biowarfare e.g., Yersinia pestis, Bacillus anthracis, etc).
Pandemics and PHEIC are the visible faces of zoonoses. There are numerous other zoonotic diseases that are widely prevalent, constitute major chunk of human infectious diseases and have a wider canvas. The humans are known to be infected with 1407 pathogens16. Of these, 61 per cent have originated from animals and among these, more than 40 per cent are viruses. Seventy five per cent emerging infectious diseases have an animal origin; five new human diseases appear every year, of which three are of animal origin and 80 per cent of agents with potential bioterrorism use are zoonotic pathogens17. These numbers are bound to increase and pose associated risks because of more qualitative and quantitative contact of humans with animals. It is estimated that in India, number of animals match with the human population18 and any increase in human population results in a corresponding increase in the number of animals. High consumption of food of animal origin is associated with high incidence of food-borne illnesses. This group of zoonotic diseases is mainly caused by bacterial pathogens unlike the PHEIC which are mostly of viral aetiology. Unlike PHEIC, which are primarily caused by viruses, the food-borne zoonotic infections are mainly bacterial in aetiology. Thirty one bacterial genera have been incriminated as causing food-borne illnesses19. The food-borne zoonoses are responsible for substantial mortality, morbidity, and economic losses across the world every year20.
Animals contract numerous diseases because of poor sanitation around their habitation. In developing world, it is not uncommon to observe co-habitation of humans and animals in an infection-friendly rural environment deprived of appropriate cleanliness, hygiene and sanitation. Instead of addressing these challenges, antimicrobial agents are used as the quick alternative to prevent infections and promote growth of the animals. This has resulted into an enormous increase in use of antibiotics in the animal health sector. It is projected that between 2013 and 2030, use of these agents shall double in India, and in a few other countries21. It is also estimated that in most of the countries, about 70 per cent of all antibiotics are consumed in the animal health sector22. The excessive use of antibiotics is recognized as one of the greatest drivers of antimicrobial resistance (AMR). It facilitates selection of resistant strains which, through the food chain find their way to human beings and cause difficult-to-treat infections. But abuse of antibiotics is not limited to animals. There is an increase in the use of antibiotics in humans also which has dangerous consequences. AMR is now considered as the greatest challenge to mankind's efforts in containing infectious diseases. In spite of strong advocacy, there seems to be little action. The inaction is going to cost heavily. AMR has already assumed serious proportions23 to the extent that we are heading towards a “post-antibiotic era”.
In the absence of any concrete and swift actions, by 2050, resistant pathogens will cause death of more than 10 million people every year which shall be more than the number of people dying of cancers and road-side accidents put together, 7.5 per cent reduction in livestock production thus impacting food security, US $ 100 trillion loss with 3.5 per cent dip in the global Gross Domestic Product (GDP), pushing 28 million people into poverty apart from many other adverse impacts23. AMR will increase healthcare costs and push millions of people into poverty. It will also negate health benefits of modern technologies and complex surgeries2324. Because of changed land use, deforestation, and illegal trade in wildlife and products, new viruses shall continue to originate from wild animals through “spill over”. These spill overs may not remain localized to a defined geographical area or population. Rapid transport shall dramatically reduce the time for international spread of zoonotic viruses and drug resistant bacteria. With thousands of flights everyday carrying 3.5 billion passengers every year25 the world can be traversed in less than 24 hours.
The internecine nature of zoonoses calls for establishment of a collaborative and collective response. This response is recognized as a One Health approach which calls upon convergence of efforts of all stakeholders to protect human and animal health26. One Health recognizes inter-connectivity between people, animals, plants, and their shared environment. It calls for a collaborative, multisectoral, and transdisciplinary approach working at the local, regional, national, and global levels with the goal of achieving optimal health outcomes26. One Health in nutshell is working together.
In spite of advocacy by several leading agencies including the WHO, the Food and Agriculture Organization of the United Nations (FAO), the World Organization for Animal Health (OIE) and United Nations Programme for Environment (UNEP), there has been an inertia in implementing activities under the One Health approach. A tripartite agreement between FAO-OIE-WHO has been in operation for advocacy and as a replicable model at the local, regional and national levels27. This model calls for coordinated action by different stakeholders to contain, prevent, detect and respond to zoonoses including AMR and food-borne illnesses.
One Health should not be construed as a stand-alone or new programme that has to be built de novo. This endeavour utilizes existing expertise and infrastructure in various sectors with emphasis on inter-sectoral coordination, collaboration and communication. Essence of One Health is to provide a formal platform to people to plan and work together to achieve shared objectives of mitigating morbidity, mortality, economic loss and social chaos.
One Health does not imply creating a new or a vertical programme. It calls for enhancing capacity of each of the existing sectors to fight infectious diseases and more importantly breaking silos to ensure a collective fight to understand, predict, prevent, detect and respond to infectious diseases through collaboration, communication, cooperation, coordination and commitment between various sectors for efficient use of resources and collective expertise2829. One Health synergizes the strength of all major stakeholders and at the same time enhances the respective capacity of these sectors to address the present and future challenges by complex and hitherto unknown infectious diseases.
A large number of zoonoses that have till date not infected livestock and humans makes the whole world vulnerable to their invasion and consequent devastation. It has been exemplified by the ongoing pandemic of COVID-19 caused by SARS-CoV-2 virus. There is an urgent need to complement the activities being undertaken by the Global Virome Project15 by using sophisticated latest virological techniques, geospatial mapping processes, big data analytics and artificial intelligence for the identification of the hotspots for such viruses across the world, detecting, isolating and characterizing the novel viruses for prior development of diagnostic and therapeutic agents including development of the prototype vaccines. In addition, collective efforts by human health and animal health sectors can accelerate early diagnosis and joint containment activities.
Zoonoses continue to have endemic and epidemic-potential and every few years will strike as PHEIC or pandemic. Next pandemic due to the zoonotic virus is imminent. Zoonoses cause huge morbidity, mortality, economic loss and social chaos and the most efficient way forward to address this challenge is an urgent application of One Health approach that harnesses global and national resources to mount efficient and effective response to zoonoses including food-borne illnesses and AMR3031. One must not forget that economic losses due to pandemics and AMR shall not halt but reverse human development as has been shown by the COVID-19 pandemic. The need for launching a coordinated multisectoral global response with active engagement of human health, animal health and environment sectors in an One Health approach was never felt more till date3233.
Conflicts of Interest: None.
References
- Zoonotic host diversity increases in human-dominated ecosystems. Nature. 2020;584:398-402.
- [Google Scholar]
- IHR procedures concerning public health emergencies of international concern (PHEIC). Available from: https://www.who.int/ihr/procedures/pheic/en/
- An analysis of International Health Regulations Emergency Committees and Public Health Emergency of International Concern Designations. BMJ Glob Health. 2020;5:e002502.
- [Google Scholar]
- Nipah virus-associated encephalitis outbreak, Siliguri, India. Emerg Infect Dis. 2006;12:235-40.
- [Google Scholar]
- Epidemiology, transmission dynamics and control of SARS: the 2002-2003 epidemic. Philos Trans R Soc Lond B Biol Sci. 2004;359:1091-105.
- [Google Scholar]
- The spread of the H5N1 bird flu epidemic in Asia in 2004. Arch Virol Suppl. 2005;19:117-29.
- [Google Scholar]
- Transmission of Nipah virus - 14 years of investigations in Bangladesh. N Engl J Med. 2019;380:1804-14.
- [Google Scholar]
- Transmission parameters of the A/H1N1 (2009) influenza virus pandemic: a review. Influenza Other Respir Viruses. 2011;5:306-16.
- [Google Scholar]
- Middle East Respiratory Syndrome Coronavirus (MERS-CoV). Available from: https://www.who.int/health-topics/middle-east-respiratory-syndromecoronavirus-mers#tab=tab_1
- Public Health Emergency of International Concern (PHEIC) has Declared Twice in 2014; Polio and Ebola at the Top. AIMS Public Health. 2015;2:218-22.
- [Google Scholar]
- Zika virus and microcephaly: why is this situation a PHEIC? Lancet. 2016;387:719-72.
- [Google Scholar]
- Origin, transmission, diagnosis and management of coronavirus disease 2019 (COVID-19) Postgrad Med J. 2020;96:753-8.
- [Google Scholar]
- Host range and emerging and reemerging pathogens. Emerg Infect Dis. 2005;11:1842-7.
- [Google Scholar]
- Centers for Diseases Control and Prevention. Zoonotic diseases. Available from: https://www.cdc.gov/onehealth/basics/zoonotic-diseases.html
- Ministry of Fisheries, Animal Husbandry & Dairying. Department of animal husbandry & dairying releases 20th livestock cencus; total livestock population increases 4.6% over census-2012, increases to 535.78 million. Available from: https://pib.gov.in/PressReleasePage.aspx?PRID=1588304#:~:text=Total%20Bovine%20population%20(Cattle%2C%20Buffalo,of%200.8%20%25%20over%20previous%20Census
- WHO estimates of the global burden of foodborne. Available from: https://apps.who.int/iris/bitstream/handle/10665/199350/9789241565165_eng.pdf;jsessionid=726E59975724BEA5DFFC37CB4178DFA4?sequence=1
- Center for Infectious Diseases Research and Policy. FDA: Antibiotic use in food animals continues to rise. Available from: https://www.cidrap.umn.edu/newsperspective/2016/12/fda-antibiotic-use-food-animalscontinues-rise#:~:text=Approximately %2070%25%20of%20all%20medically,96%25%20 from%202009%20to% 202015
- Review on Antimicrobial Resistance. Tackling drug-resistant infections globally: Final report and recommendations. Available from: https://amr-review.org/sites/default/files/160525_Final%20paper_with%20cover.pdf
- Antimicrobial resistance in developing Asian countries: burgeoning challenge to global health security demanding local approaches. Global Biosecurity. 2019;1:50-4.
- [Google Scholar]
- International Civil Aviation Organization. Continuing traffic growth and record airline profits highlight 2015 air transport results. Available from: https://www.icao.int/Newsroom/Pages/Continuing-Traffic-Growth-and-Record-Airline-Profits-Highlight-2015-Air-Transport-Results.aspx
- From SARS to COVID-19: a previously unknown SARS-related coronavirus (SARS-CoV-2) of pandemic potential infecting humans – call for a One Health approach. One Health. 2020;9:100124.
- [Google Scholar]
- Zoonoses: FAO/OIE/WHO Collaboration (Tripartite). Available from: https://www.who.int/zoonoses/concept-note/en/
- Food and Agriculture Organization. One Health. Available from: http://www.fao.org/one-health/en/
- Implementation framework for One Health approach. Indian J Med Res,. 2019;149:329-31.
- [Google Scholar]
- Feasibility of combating antimicrobial resistance using One Health approach. Available from: file:///C:/Users/ICMR/Desktop/Downloads/241124-Article%20Text-828833-1-10-20200415.pdf
- Infectious disease threats in the twenty-first century: Strengthening the global response. Front Immunol. 2019;10:549.
- [Google Scholar]
- Control and prevention of infectious diseases from a One Health perspective. Genet Mol Biol. 2021;44(1 Suppl 1):e20200256.
- [Google Scholar]
- Make science evolve into a One Health approach to improve health and security: a white paper. One Health Outlook. 2020;2 doi:10.1186/s42522-019-0009-7
- [Google Scholar]





