Translate this page into:
Upsurge of chikungunya cases in Uttar Pradesh, India
For correspondence: Dr Amita Jain, Department of Microbiology, King George's Medical University, Lucknow 226 003, Uttar Pradesh, India e-mail: amita602002@yahoo.com
-
Received: ,
This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
This article was originally published by Wolters Kluwer - Medknow and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Background & objectives:
Chikungunya (CHIK) re-emerged in India in 2006 after a gap of three decades. In Uttar Pradesh (UP), <100 confirmed cases per million were reported during this outbreak. Based on an upsurge of CHIK cases at UP, this retrospective study was conducted to investigate clinical and serological profile of CHIK cases in UP.
Methods:
A retrospective study was done on all clinically suspected CHIK cases that had been tested by ELISA for anti-CHIK virus IgM antibodies from September 2012 to December 2017. Based on clinical features, a subset of patients had earlier been tested serologically for dengue and Japanese encephalitis (JE).
Results:
Of the 3240 cases enrolled, 771 (23.8%) were seropositive. Patients had a range of clinical manifestations with seropositivity highest in those exhibiting arthralgia with fever (40%), followed by fever of unknown origin (FUO) (22%), encephalitis (13%) and fever with rash (12%). Cases (total, seropositive) increased over 20-fold in 2016 (1389, 412) and 2017 (1619, 341), compared to 2012-2015. Nearly a third of dengue serology-positive cases and a fifth of JE serology-positive cases were co-positive for CHIKV.
Interpretation & conclusions:
Archival data from 2006-2011 and data from this study (2012-2017) indicated that UP experienced first CHIK outbreak in the decade in 2016, as part of a large-scale upsurge across northern India. CHIK should be considered as a differential diagnosis in patients presenting with fever of unknown origin or fever with rash or acute encephalitis, in addition to classical arthralgia.
Keywords
Acute febrile illness
arbovirus
chikungunya
encephalitis
fever of unknown origin
Uttar Pradesh
Chikungunya (CHIK), an arboviral illness transmitted by Aedes mosquitoes, is globally considered as a re-emerging disease123. In India, after an epidemic in 1973, it had been silent till its re-emergence in 2005-200645. Since then, its epidemic has been ongoing in many States, with significant affliction of the populace4567. The National Vector Borne Disease Control Programme, Government of India, reported 12205 confirmed cases for 20198. Classically, it manifests as arthralgia, myalgia, high-grade fever, headache and/or rash5. Due to lack of vaccination and pharmacotherapy, prevention and supportive care are mainstays of management89. Knowledge of its epidemiology, the basis of primary prevention, is thus important in tackling outbreaks.
Uttar Pradesh (UP), being heavily infested by Aedes, has long been endemic for dengue10 but it had <100 confirmed cases of CHIK per million people during 2006-2011. The State was also unaffected by 2006 CHIK outbreak, despite its virus (CHIKV) being carried by the same vector as dengue, with <100/million confirmed cases11. The objective of this study was to determine the clinical, demographic and serological profile in CHIK cases tested at an apex public referral centre of UP.
Material & Methods
This retrospective study was conducted in June 2018 on data of all cases tested for anti-CHIKV IgM antibody from September 2012 to December 2017 at Viral Research and Diagnostic Laboratory, department of Microbiology, King George's Medical University, Lucknow, India. The Institutional Ethics Committee had approved the study (90th ECM II B-FS/P8).
Considering clinical features, a subset of samples had been tested for Dengue Virus (DENV) using NS1 antigen and/or IgM antibody based on duration of fever12. A subset of patients presenting with acute encephalitis syndrome (AES), had been tested for anti-CHIKV IgM antibody, along with anti-Japanese encephalitis virus (JEV) IgM antibody. All serology kits were ELISA-based (ICMR-National Institute of Virology, Pune, India). Based on clinical manifestations, patients had been categorized either as arthralgia with fever (classical of CHIK), fever with rash, fever of unknown origin (FUO) or acute encephalitis syndrome (AES), while all had been tested for anti-CHIKV IgM antibody. Their clinical history had been recorded and informed consent obtained during testing for future serological research.
Inter-group comparisons of categorical and continuous variables were done using Chi-square and Fischer's exact test, respectively. The correlation between continuous variables was assessed by Pearson's coefficient. Meteorological data were obtained from www.wunderground.com.
Results & Discussion
Three thousand two hundred and forty cases were included, with seropositivity of 23.8 per cent (n=771). While total and seropositive cases were <100 annually in 2012-2015, they increased over 20-fold in 2016 and 2017 (Figure A). Based on archival data of 2006-201111, and the present data from 2012-2017, it was found that there were <100 confirmed CHIK cases per million in UP annually during 2006-2015, despite multiple outbreaks in adjoining States of Delhi and Madhya Pradesh, having a significant inter-provincial population flux11. The upsurge suggested that UP had its first CHIK outbreak in the decade (2006-2016). Sequencing and phylogenetic analysis on E1 gene done at our institution demonstrated that the 2016 outbreak had the same causative viral strain in UP and Delhi13. All three States had dengue outbreaks in this period, with the same vector as CHIK10.
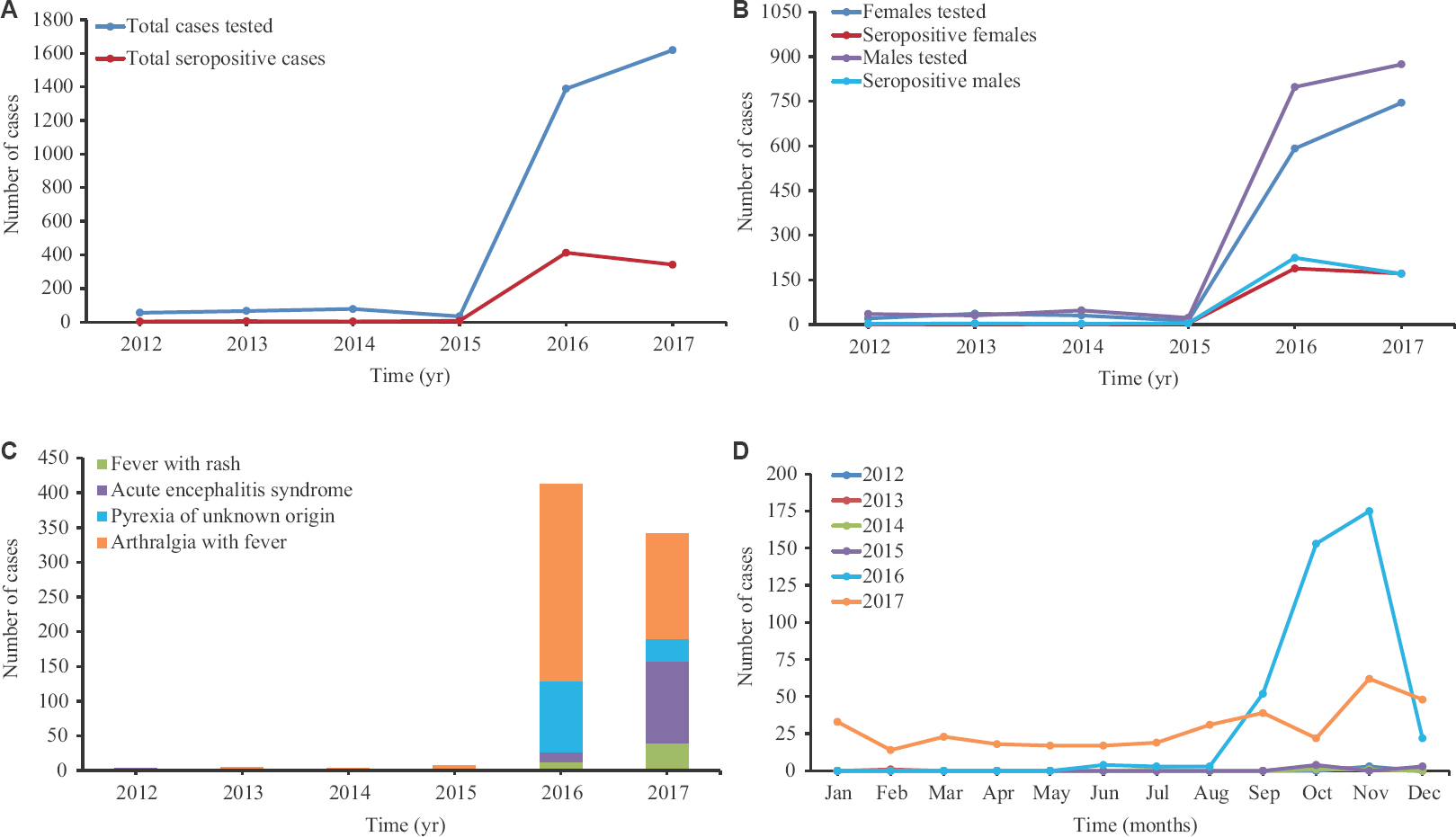
- (A) Year-wise distribution of chikungunya cases in Uttar Pradesh depicting total number of cases tested for anti-chikungunya IgM antibody and the number found seropositive. (B) Sex distribution of cases tested and seropositive cases per year. (C) Distribution of the four clinical presentations of seropositive cases per year. (D) Monthly distribution of seropositive cases per year.
The female-to-male case ratio (794:1000) was significantly different from sex ratio (912:1000) of UP (P<0.001)14. However, no significant difference was found in proportion of male and female cases (Figure B). The seropositive cases presented majorly as arthralgia with fever (57.2%), followed by FUO (18.3%), acute encephalitis (17.4%) and the least as fever with rash (7%). The seropositivity was highest in the age group of 45-60 yr (37.7%), followed by >60 yr (30.6%) and 15-45 yr (26.7%) (Table).
| Year | Age group (yr) | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| 0-5 | >5-15 | >15-45 | >45-60 | >60 | ||||||
| CT | SP (%) | CT | SP (%) | CT | SP (%) | CT | SP (%) | CT | SP (%) | |
| 2012 | 0 | 0.0 | 8 | 0.0 | 38 | 5.3 | 5 | 0.0 | 4 | 25.0 |
| 2013 | 1 | 0.0 | 12 | 8.3 | 42 | 4.8 | 7 | 0.0 | 2 | 0.0 |
| 2014 | 5 | 0.0 | 23 | 4.3 | 39 | 5.1 | 8 | 0.0 | 1 | 0.0 |
| 2015 | 0 | 0.0 | 4 | 0.0 | 25 | 24.0 | 4 | 25.0 | 1 | 0.0 |
| 2016 | 119 | 10.9 | 211 | 15.2 | 782 | 31.6 | 211 | 45.5 | 52 | 38.5 |
| 2017 | 268 | 15.7 | 320 | 14.1 | 644 | 24.4 | 174 | 32.8 | 74 | 27.0 |
| Total | 393 | 14.0 | 578 | 13.7 | 1560 | 26.7 | 409 | 37.7 | 134 | 30.6 |
CT, cases tested; SP, seropositivity
A significant difference was observed between 2016 and 2017 in the most common clinical presentation of cases (P<0.001), being arthralgia with fever (68.7%) and FUO (25%) in 2016 and arthralgia with fever (44.3%) and AES (34.3%) in 2017 (Figure C). A significant rise in proportion of encephalitis as a presentation among all seropositive cases was seen from 2016 (3.4%) to 2017 (34.3%) (95% CI=25.6-36.3, P<0.001) (Figure C). A significant difference was observed between age groups in clinical presentation (P<0.001). Most seropositive cases presented with arthralgia and fever in age groups 15-45 yr (64.9%), 45-60 yr (78.0%) and above 60 yr (70.7%). However, they mainly presented as encephalitis in ages 0-5 yr (76.4%) and 5-15 yr (41.8%).
No correlation was found between number of cases or seropositivity and either of average monthly temperature, precipitation or dew point, during 2012-2017. However, peak in cases was observed during August-to-December in 2016 and 2017 (Figure D).
Six hundred and fifty four and 2516 cases were tested additionally for JEV and DENV respectively. Of the 480 cases seropositive for DENV, 148 (31%) were co-positive for CHIKV. Of the 65 seropositive for JEV, 12 (18%) were co-positive for CHIKV, among whom over half were 0-5 yr old. It was found that 65 AES cases were JEV negative and CHIKV positive, whereas seven patients were co-positive for all three arboviruses. This co-positivity may be due to cross-reactivity, pre-existing immunity or co-infection, the latter being pertinent in high viral transmission areas. Furthermore, UP is a hyperendemic region for DENV and JEV10. More studies are needed in future to demonstrate these as a true co-infection. Many common aetiologies of AES in India have been reported, other than JEV, including scrub typhus and DENV151617. Demographic data of all these agents can be combined to better explain the epidemiology of AES.
Our study had several limitations. The exact aetiological agent(s) could not be determined due to logistic challenges to performing either the plaque reduction and neutralization test or demonstrating four-fold rise in antibody titres. Another drawback compromising case numbers was due to the patients not reaching the hospital because of mild manifestations and those expiring prior to hospitalization.
In conclusion, our findings indicate that UP experienced CHIK outbreak in 2016, with the illness having clinically overlapping picture with other arboviral diseases. Therefore, while CHIK as a possibility must not be ignored in classic cases of severe arthralgia with fever, it is important to consider it as a differential in patients presenting with FUO or fever with rash or acute encephalitis.
Financial support & sponsorship: The first author (AO) acknowledges the Indian Council of Medical Research, New Delhi, for providing Short Term Studentship (ICMR-STS 2018-02187).
Conflicts of Interest: None.
References
- Updates on chikungunya epidemiology, clinical disease, and diagnostics. Vector Borne Zoonotic Dis. 2015;15:223-30.
- [Google Scholar]
- Emergence of chikungunya virus in Indian subcontinent after 32 years: A review. J Vector Borne Dis. 2006;43:151-60.
- [Google Scholar]
- Guidelines for prevention and control of chikungunya fever. New Delhi: WHO SEARO; 2009.
- Chikungunya epidemic in India: A major public-health disaster. Lancet Infect Dis. 2007;7:306-7.
- [Google Scholar]
- Chikungunya in Southeast Asia: Understanding the emergence and finding solutions. Int J Infect Dis. 2011;15:e671-6.
- [Google Scholar]
- 2019. Chikungunya Situation in India. Ministry of Health & Family Welfare, Government of India. Available from: http://www.nvbdcp.gov.in
- Current perspectives on the spread of dengue in India. Infect Drug Resist. 2014;7:337-42.
- [Google Scholar]
- Fading chikungunya fever from India: Beginning of the end of another episode? Indian J Med Res. 2014;139:468-70.
- [Google Scholar]
- WHO informal consultation on fever management in peripheral health care settings: A global review of evidence and practice. Available from: https://apps.who.int/iris/bitstream/handle/10665/95116/9789241506489_eng.pdf;sequence=1
- Chikungunya outbreak in Delhi, India, 2016: Report on coinfection status and comorbid conditions in patients. New Microbes New Infect. 2017;20:39-42.
- [Google Scholar]
- 2011. Available from: http://censusindia.gov.in/2011-prov-results/prov_rep_tables.html
- Acute encephalitis syndrome in India: The changing scenario. Ann Neurosci. 2016;23:131-3.
- [Google Scholar]
- Emergence of orientia tsutsugamushi as an important cause of acute encephalitis syndrome in India. PLoS Negl Trop Dis. 2018;12:e0006346.
- [Google Scholar]
- Epidemiology and etiology of acute encephalitis syndrome in North India. Jpn J Infect Dis. 2014;67:197-203.
- [Google Scholar]






