Translate this page into:
Limb gangrene: The first sign of essential thrombocythemia
*For correspondence: zahitb@yahoo.com
-
Received: ,
This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
This article was originally published by Wolters Kluwer - Medknow and was migrated to Scientific Scholar after the change of Publisher.
Clinical ImageAn 84 yr old female patient†, previously asymptomatic until eight weeks ago, presented to the Emergency Medicine department, Adnan Menderes University Hospital, Aydın, Turkey, in April 2018 with pain in the right leg. The leg was discoloured black beginning from the middle of the tibia to the toes (Figure A and B), with lack of sensation of pain and absent popliteal artery and dorsalis pedis pulsations. Her leucocyte count was 24,500/μl, haemoglobin level was 8 g/dl and platelet count was 1500×106/l. In the peripheral blood smear, hypochromia, microcytosis and anisothrombocytosis were observed (Figure C). There was no arterial flow on popliteal and anterior and posterior tibial arteries, all of them totally occluded by a thrombus on Doppler ultrasonography. An allelic burden of 70 per cent heterozygous for the JAK 2 V617FA mutation was seen with fluorescence in situ hybridization, and Philadelphia chromosome was negative. Bone marrow revealed increased marrow cellularity and marked megakaryocytic hyperplasia, some of which showed hyperlobated nuclei without fibrosis (Figure D). There was no history of smoking, diabetes mellitus, atrial fibrillation or peripheral vascular disease, and the condition was diagnosed as limb gangrene due to essential thrombocythemia. Below-knee amputation was performed and hydroxyurea 2 g/day with aspirin 100 mg/day was initiated. The dose of hydroxyurea was decreased to 1 g/day when the patient's platelet count was <500,000/μl. On a follow up after six months, the overall condition was good. Her leucocyte count was 7,000/μl, haemoglobin level was 10 g/dl and platelet count was 385,000×106/l.
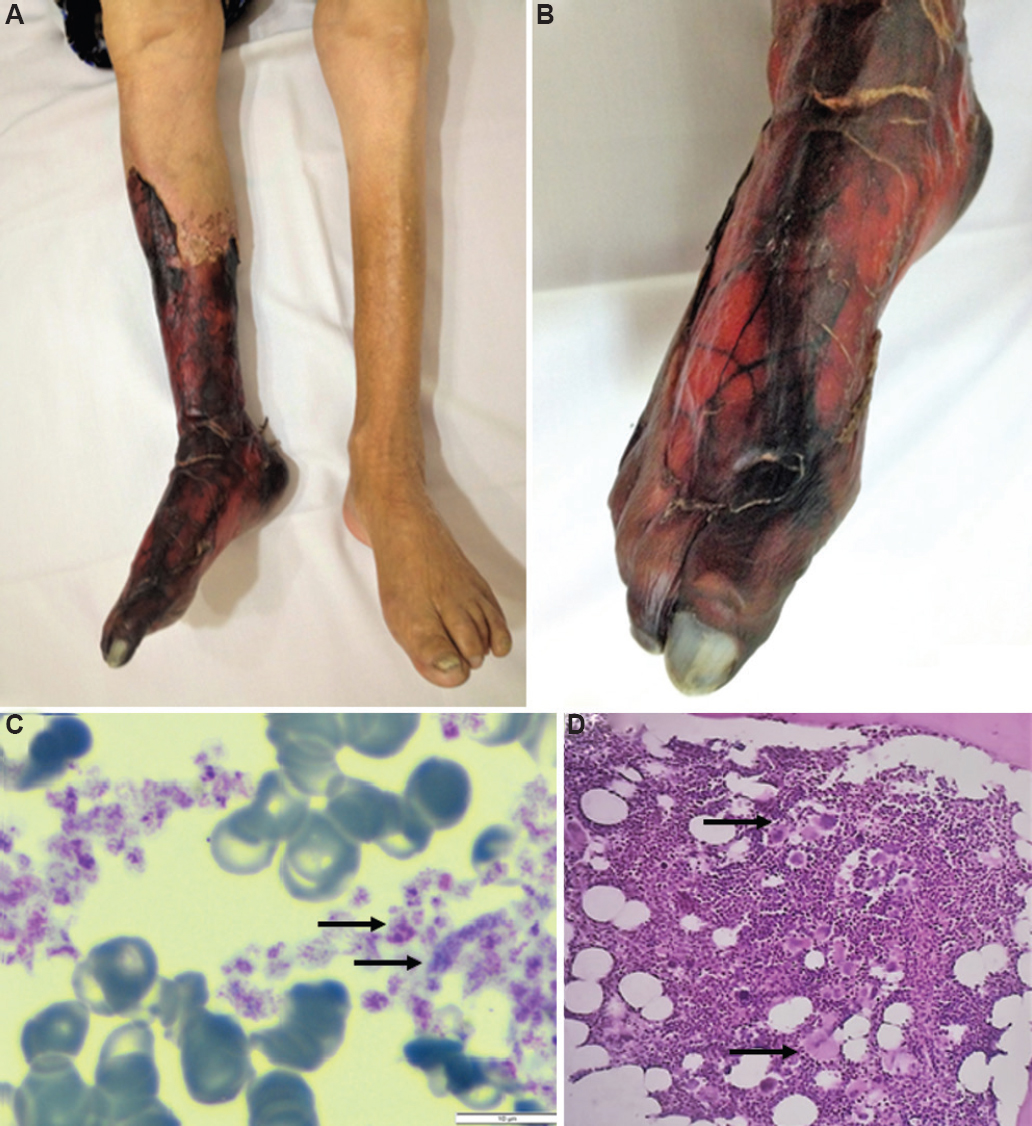
- (A and B) Appearance of the patient's right leg and ankle. (C) Thrombocytosis in the patient's peripheral smear with staining (May-Grunwald and Giemsa, ×1000; scale bar 10 μm). The differences in platelet size are remarkable (arrows). (D) Marrow trephine biopsy (Hematoxylin & Eosin X, ×20) showing megakaryocyte proliferation with hyperlobulated forms in the marrow specimen of the patient (arrows pointing to megakaryocytes).
Conflicts of Interest: None.





