Translate this page into:
Action-oriented colour-coded foot length calliper for primary healthcare workers as a proxy for birth weight & gestational period
Reprint requests: Dr. Asha K. Pratinidhi, Krishna Institute of Medical Sciences University, Karad 415 110, Maharashtra, India e-mail: ashapratinidhi@gmail.com
-
Received: ,
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Background & objectives:
Foot length of the newborn has a good correlation with the birth weight and is recommended to be used as a proxy measure. There can be variations in the measurement of foot length. A study was, therefore, carried out to develop a foot length calliper for accurate foot length measurement and to find cut-off values for birth weight and gestational age groups to be used by primary healthcare workers.
Methods:
This study was undertaken on 645 apparently healthy newborn infants with known gestational age. Nude birth weight was taken within 24 h of birth on a standard electronic weighing machine. A foot length calliper was developed. Correlation between foot length and birth weight as well as gestational age was calculated. Correctness of cut-off values was tested using another set of 133 observations on the apparently healthy newborns. Action-oriented colour coding was done to make it easy for primary healthcare workers to use it.
Results:
There was a significant correlation of foot length with birth weight (r=0.75) and gestational age (r=0.63). Cut-off values for birth weight groups were 6.1, 6.8 and 7.3 cm and for gestational age of 6.1, 6.8 and 7.0 cm. Correctness of these cut-off values ranged between 77.1 and 95.7 per cent for birth weight and 60-93.3 per cent for gestational age. Considering 2.5 kg as cut-off between normal birth weight and low birth weight (LBW), cut-off values of 6.1, 6.8 and 7.3 were chosen. Action-oriented colour coding was done by superimposing the colours on the scale of the calliper, green indicating home care, yellow indicating supervised home care, orange indicating care at newborn care units at primary health centres and red indicating Neonatal Intensive Care Unit care for infants.
Interpretation & conclusions:
A simple device was developed so that the primary health care workers and trained Accredited Social Health Activist workers can identify the risk of LBW in the absence of accurate weighing facilities and decide on the type of care needed by the newborn and take action accordingly.
Keywords
Birth weight
colour coding
foot length
foot length calliper
gestational age
neonatal anthropometry-receiver operating characteristic curve
Of the various anthropometric measurements used as a proxy for birth weight, foot length has a good correlation with the birth weight and the gestational age1234567. The birth weight is widely used and accepted measurement of growth of the infant with or without knowledge of gestational period. Utility of foot length is found to be simple and significant in the identification of low birth weight (LBW) as well as preterm infants who need special care8910. Accuracy of measurement of foot length is important because the differences in the foot length measurement are usually found in millimetres. Methods used such as taking impression of the foot with an ink or measuring it by an ordinary measuring tape, or a foot ruler is often associated with variations. Some researchers have suggested simple devices to measure accurate foot length1112. However, these devices are cumbersome and unsuiTable to be used in the field.
Foot length can be used as a proxy for birth weight for a newborn to determine ‘at risk’ LBW infant. The infants born in remote rural areas, at home or in a subcentre where the facilities are limited, are unlikely to be weighed at birth. A simple device to measure foot length to be used by the primary healthcare workers to detect the risk related to LBW and to take appropriate action is, therefore, needed.
The risk for the newborn is higher if the gestational age is <34 wk. In rural settings in India, very often the last menstrual period (LMP) is not accurately known, and the gestational period, therefore, is difficult to calculate. Under these circumstances, a proxy measure for gestational age would be useful to assess the underlying risk. This study was undertaken to develop a colour-coded foot length calliper to measure the foot length of the newborn accurately and also to find cut-off values for birth weight and the gestational age.
Material & Methods
This study was undertaken at Krishna Hospital and Medical Research Centre, Karad, Maharashtra, India, during 2013-2014. All consecutive singleton apparently healthy newborns born to apparently healthy mothers knowing their LMP were included in the study. The nude birth weight of each baby was measured on a standard electronic weighing machine (Vijay Digital System, 24B Technology). Gestational period was calculated from the LMP. Ethical clearance was obtained from the Institutional Ethics Committee, and an informed written consent of the mothers was taken before taking the anthropometric measurements.
A foot length calliper was prepared in such a way that it would be able to fix the two extreme ends of the foot and measure the distance between these two ends in centimetre (Fig. 1A). The foot length measurement was done on this calliper by taking the lower most point on convex curvature of the heel and the uppermost point of the convex curvature of the longest toe, usually greater toe but sometimes second toe (Fig. 1B) (Patent No. US 2013/ 0167391 A1).
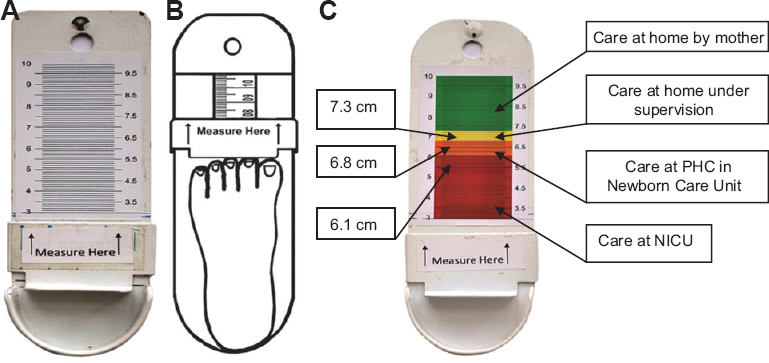
- (A) Foot length calliper with scale only, (B) foot length calliper showing accurate method of measurement of foot length. (C) Action-oriented colour-coded foot length calliper. NICU, Neonatal Intensive Care Unit.
The minimum numbers of infants required for determining correlation between foot length with birth weight, and gestational age were calculated513 to be 48 and 502, respectively. Care was also taken to fulfil minimum sample size for each of the gestational age strata (i.e., <32, 32 to <34, 34 to <37 and ≥37 wk) using observed mean and standard deviation (SD) of foot lengths13 for these strata. The minimum required sample sizes were 14, 20, 20 and 19, respectively, for gestational age <32, 32-<34, 34-<37 and ≥37 wk.
There were 703 infants born during the study period. Of these, 58 were excluded because of some abnormality, disease, multiple births or non-availability of LMP. The study was carried out on 645 consecutive infants fulfilling inclusion criteria. The foot length of all these infants was measured on the newly devised foot length calliper (Fig. 1A).
Colour coding of foot length calliper: Since the device was prepared for the grass root level workers, with limited literacy, it was decided to use four colours indicating the type of care to be given to the neonate; the red colour indicating the care at Neonatal Intensive Care Unit (NICU), orange colour indicating the care at neonatal care unit at the primary health centre (PHC), yellow colour indicating supervised care at home and green colour indicating routine home care of the newborn (Fig. 1C).
Statistical analysis: Correlation coefficients for foot length with birth weight and gestational period were calculated for these 645 infants. These infants were categorized according to birth weight: <1.5, 1.5-<2, 2.0-<2.5 and ≥2.5 kg and gestational period of <32, 32-<34, 34-<37 and ≥37 wk. Respective foot lengths were compared by applying ANOVA and further by Bonferroni multiple comparison test. Corresponding cut-off values for foot length were identified by receiver operating characteristic (ROC) curve analysis on the basis of maximum sensitivity and specificity for birth weight and gestational age groups. A separate set of 133 values of birth weight, gestational age and foot length was collected using the same inclusion and exclusion criteria. The correctness of the foot length cut-off values was assessed on this data set.
Results
The mean foot length increased as birth weight increased (P<0.001). Bonferroni multiple comparison test revealed a significant trend (P<0.01). Foot length also increased with gestational age (P<0.001). However, Bonferroni multiple comparison test revealed similar foot length for gestational age <32 and 32-<34 wk. In comparison to these two gestational age groups, foot length was significantly higher for other gestational age groups (Table I).
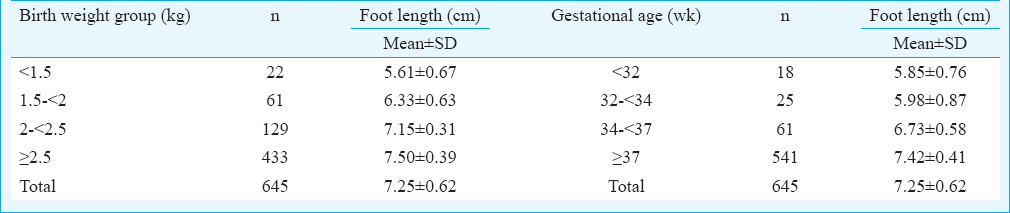
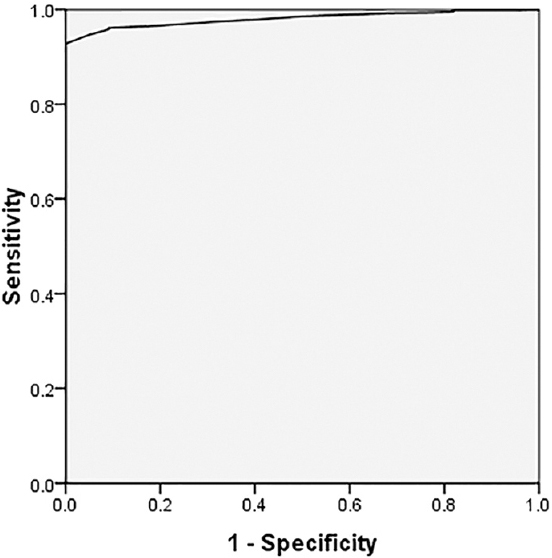
Correlation of foot length and birth weight: The overall correlation coefficient between foot length and birth weight was 0.75 [95% confidence interval (CI): 0.71-0.78] (P<0.001) with a partial correlation coefficient 0.57 (P<0.001) after controlling effect of gestational age. The correlation coefficient indicated the feasibility of accurate foot length being used for categorizing the neonates as <1.5, <2.0, <2.5 and ≥2.5 kg infants. To demarcate four birth weight groups, three cut-off values of foot length were computed by the use of ROC curve method. Birth weight category was taken as a dependent variable and foot length was taken as an independent variable to carry out ROC curve analysis. This analysis revealed 6.1, 6.8 and 7.3 cm as cut-off values of the foot lengths for identifying infants in different categories of birth weight as given in Table II.
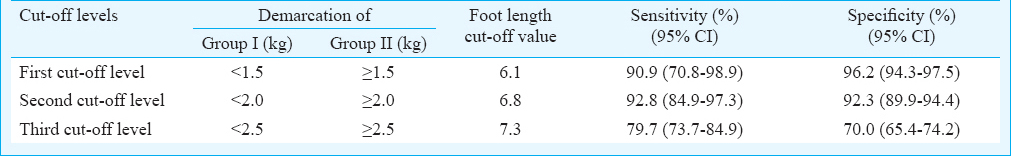
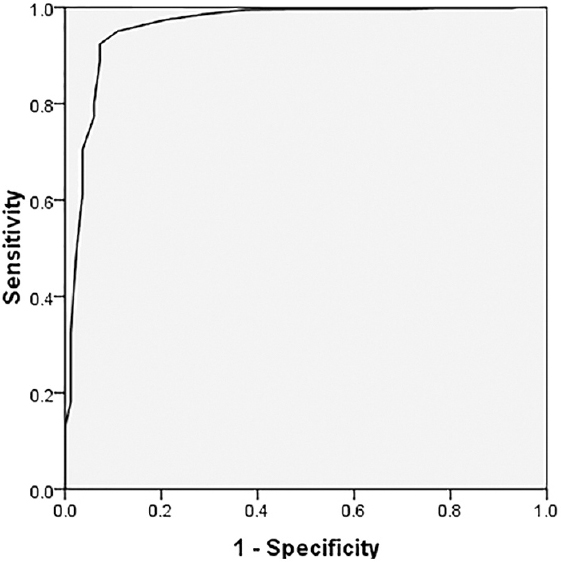
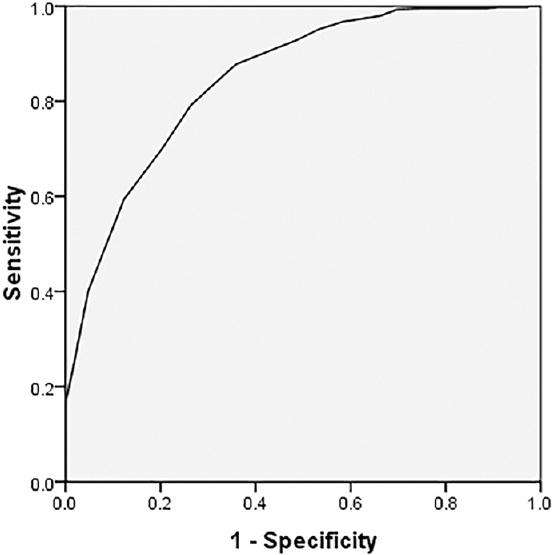
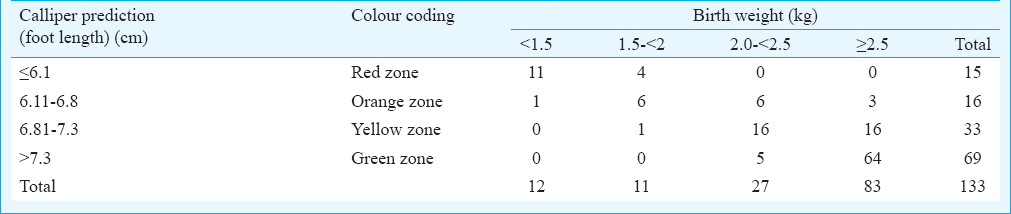
The area under the ROC curve for the first cut-off value was 0.980 (Fig. 2); for the second cut-off value, it was 0.959 (Fig. 3) and for the third cut-off value, it was 0.848 (Fig. 4). The accuracy of these cut-off values was tested using a different set of observations of 133 neonates. Foot length ≤6.1 cm identified 11 of the 12 i.e., 91.7 per cent infants having birth weights <1.5 kg, foot length ≤6.8 cm identified 22 out of 23 i.e., 95.7 per cent infants with birth weights <2.0 kg, foot length ≤7.3 cm identified 45 out of 50 i.e., 90 per cent infants with birth weights <2.5 kg and foot length >7.3 cm identified 64 out of 83 i.e., 77.1 per cent infants with birth weight ≥2.5 kg (Table III).
- Sensitivity and 1-specificity by receiver operating characteristic curve analysis for classification between <1.5 and ≥1.5 kg birth weight for various foot lengths.
- Sensitivity and 1-specificity by receiver operating characteristic curve analysis for classification between <2.0 and ≥2.0 kg birth weight for various foot lengths.
- Sensitivity and 1-specificity by receiver operating characteristic curve analysis for classification between <2.5 and ≥2.5 kg birth weight for various foot lengths.
Correlation of gestational period and foot length: The overall correlation coefficient between foot length and gestational age was 0.63 (95% CI: 0.58-0.68) (P<0.001) with a partial correlation coefficient 0.36 (P<0.001) after controlling effect of birth weight. A small but significant correlation coefficient indicated the feasibility of use of foot length for categorizing the neonates according to gestational age as <32, <34, <37 and ≥37 wk.
To demarcate four gestational age groups, three cut-off values of foot length were computed using ROC curve method. Gestational age category was taken as a dependent variable and foot length was taken as an independent variable to carry out ROC curve analysis. This analysis revealed 6.1, 6.8 and 7.0 cm as cut-off foot lengths for identifying infants of different gestational age categories (Table IV).
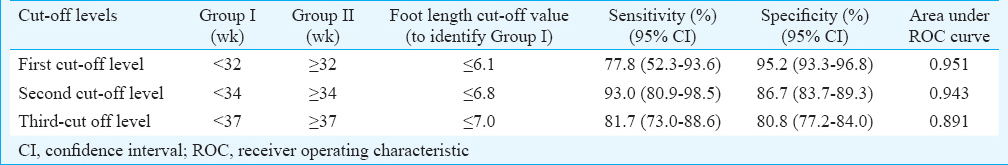
The accuracy of foot length cut-off values against gestational age (Table V) revealed that foot length ≤6.1 cm identified 3 out of 5 i.e., 60 per cent infants with gestational age <32 wk, foot length ≤6.8 cm identified 9 out of 10 i.e., 90 per cent infants with gestational age <34 wk, foot length of ≤7 cm identified 28 out of 30 i.e., 93.3 per cent infants with gestation age of <37 wk and foot length >7 cm identified 87 out of 103 i.e., 84.5 per cent infants with gestational age ≥37 wk.
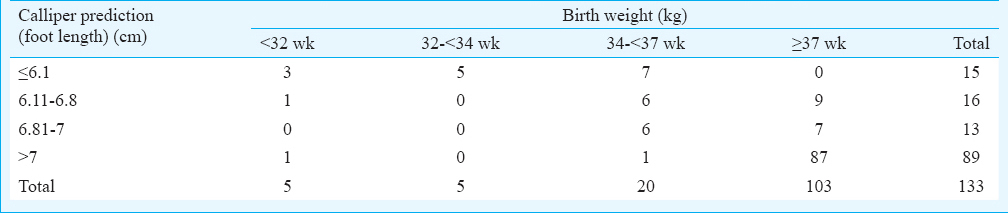
It was interesting to observe that first two cut-off values for birth weight i.e., 6.1 and 6.8 cm synchronized exactly with the first two cut-off values for the gestational age groups. Thus, the cut-off value of ≤6.1 cm foot length was indicative of <1.5 kg birth weight and/or gestational age of <32 wk. Similarly, a cut-off value of ≤6.8 cm was indicative of <2 kg birth weight and/or gestational age of <34 wk. There was a disparity at third cut-off value for birth weight and gestational age; ≤7.3 cm was the cut-off value for <2.5 kg birth weight whereas ≤7.0 cm was the cut-off value for <37 wk gestational age. Nearly 3.4 per cent infants would have been added by increasing the foot length by 0.3 cm i.e., 7.3 corresponding to the cut-off value demarcating LBW and normal birth weight (NBW) (Table III). Thus, for prematurity, use of 7 and 7.3 cm made a difference of only 3.4 per cent.
The calliper was, therefore, devised with three cut-off values: 6.1, 6.8 and 7.3 cm. The scale on the calliper was superimposed by four colour-coded zones according to birth weight categories (Fig. 1C). Area on the scale of the foot length above 7.3 cm was painted green, indicative of normal birth weight of 2.5 kg and above. Area between foot lengths of 6.8 to 7.3 cm was painted yellow and indicated birth weight group of ≥2 to <2.5 kg. Area between foot lengths of 6.1 to 6.8 cm was painted orange and indicated birth weight group of ≥1.5 to <2 kg and/or gestational period >32 wk but <34 wk. The area below 6.1 cm was painted red and indicated birth weight below 1.5 kg and/or gestational age <32 wk.
Discussion
The present study revealed significant correlation of foot length with birth weight (r=0.75) and gestational age (r=0.63). Correlation between foot length and birth weight in other studies2345 ranged from 0.42 to 0.9, whereas correlation between foot length and gestational age has ranged from 0.133 to 0.86825.
Some studies2311 have given cut-off values for gestational age. The foot length values for corresponding gestational age were greater2 or lesser311 by 2-3 mm. The cut-off value given by one study11 showed higher values than ours for 1.5 kg birth weight by 4 mm. Another study had values similar to ours7, whereas the third study4 had values one centimetre lesser than each of the cut-off values of our study. This could be due to variations in the foot length measurement techniques. Accuracy of our cut-off values was assessed by taking 133 observations not included in the group, from which the computation of foot length cut-off values has been done. Similar to our study, some other studies8910 have also shown utility of foot length measure in the identification of birth weight category specifically at home or in remote area.
Different researchers have used different techniques for foot length measurement such as foot length gauge18, foot print2511, Vernier calliper4, stiff plastic metric ruler69 and foot length calliper7. In none of these except foot length calliper used by Kakrani et al7, there was a curvilinear arrangement for resting of the heel. The present newly devised calliper has curvilinear provision to rest the heel and fix two extreme ends of foot for foot length measurement. It is a simple device where cut-off values for birth weight groups were designated using colour coding. The primary healthcare workers can identify the birth weight group without taking birth weight or without measuring the foot length. Accredited Social Health Activist (ASHA) workers working in rural areas could be very easily taught to use this colour-coded foot length calliper. It is very likely that the health worker may not be able to take accurate measurement up to 1 mm and memorize the cut-off values for different birth weight/gestation groups for taking appropriate action. Hence, colour coding was done.
We commonly observe that LBW infants <1.5 kg and/or preterm infants <34 wk of gestation have a difficulty in feeding if the sucking and swallowing reflexes have not well developed. Usually, these reflexes are developed by 32 wk of gestation or by 1.5 kg birth weight. Hence, foot length corresponding with >1.5 kg and ≥32 wk was considered as cut-off level to demarcate these LBW/preterm infants in need of NICU care. The second cut-off was taken to demarcate infants >2 kg and ≥34 wk of gestation. A birth weight of 2.5 kg and above is universally considered as NBW; hence, the third cut-off level was chosen at foot length corresponding to 2.5 kg birth weight although the third cut-off for birth weight was 7.3 cm and that of gestational age was 7.0 cm. Considering the problem of intrauterine growth restriction in the developing world including India14, where despite complete gestational period i.e., 37-40 wk the infants fail to gain adequate weight, it was decided to accept 7.3 as the third cut-off value so as to include all LBW infants with or without prematurity.
The applicability of the use of calliper and cut-off points for small for gestational age, appropriate for gestational age and large for gestational age combining birth weight and gestational age could not be worked out. This was the limitation of the study.
In conclusion, a simple colour coded and action oriented tool of foot length calliper was developed for the use of primary healthcare workers. This may help to grade the birth weight of the newborn and make a decision of appropriate level of care according to the birth weight group without a need to take birth weight or measure actual foot length.
Acknowledgment
Authors acknowledge financial assistance from Krishna Institute of Medical Sciences University, Karad, Maharashtra, India.
Conflicts of Interest: None.
References
- Foot length – A new and potentially useful measurement in the neonate. Arch Dis Child. 1979;54:226-30.
- [Google Scholar]
- Foot length measurement from foot print for identifying a newborn at risk. J Trop Pediatr. 1988;34:16-9.
- [Google Scholar]
- Prediction of weight of Indian children aged upto two years based on foot-length: Implications for emergency areas. Indian Pediatr. 2006;43:125-30.
- [Google Scholar]
- Assessment of growth from foot length in Taiwanese neonates. Pediatr Neonatol. 2009;50:287-90.
- [Google Scholar]
- Measuring newborn foot length to identify small babies in need of extra care: A cross sectional hospital based study with community follow-up in Tanzania. BMC Public Health. 2010;10:624.
- [Google Scholar]
- The reliability of a newborn foot length measurement tool used by community volunteers to identify low birth weight or premature babies born at home in Southern Tanzania. BMC Public Health. 2014;14:859.
- [Google Scholar]
- Measuring new born foot length to identify small babies in need of extra care: A cross-sectional hospital based study. Iran J Pediatr. 2013;23:508-12.
- [Google Scholar]
- Identifying high-risk babies born in the community using foot length measurement at birth in Uganda. Child Care Health Dev. 2013;39:20-6.
- [Google Scholar]
- A simple device for measurement of foot length in neonates. J Trop Pediatr. 1986;32:268-9.
- [Google Scholar]
- A simple tool for assessment of gestational age in newborns using foot length. J Evol Med Dent Sci. 2014;3:6424-9.
- [Google Scholar]
- Intrauterine growth retardation – Small events, big consequences. Ital J Pediatr. 2011;37:41.
- [Google Scholar]






