Translate this page into:
Clinical profile & complications of neurotoxic snake bite & comparison of two regimens of polyvalent anti-snake venom in its treatment
Reprint requests: Dr Tarun Kumar Dutta, Department of General Medicine, Jawaharlal Institute of Postgraduate Medical Education & Research, Puducherry 605 006, India e-mail: tkduttajipmer@yahoo.co.uk
-
Received: ,
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Background & objectives:
The optimal anti-snake venom (ASV) dose required to treat neurotoxic snake envenomation is not known. Low-dose ASV (national protocol: maximum dose 200 ml) may be as efficacious as the conventional regimen (100 ml six hourly till all symptoms disappear), but a direct comparison of the regimens is not available. The aim of this study was to test the efficacy of low-dose ASV regimen against the conventional high-dose regimen.
Methods:
The clinical profile of 51 patients with neurotoxic snake envenomation was studied. Patients were treated with either the national protocol or the conventional protocol for ASV administration. The time to complete recovery of symptoms, duration of mechanical ventilation and total dose of ASV were compared.
Results:
More patients were females (28 vs. 23) bitten in the early morning hours (2400-0600 h). Thirty nine of 51 (76.4%) patients required mechanical ventilation. In terms of progression of neuroparalysis, time to complete resolution of ptosis and occurrence of VAP and ASV reactions, there was no difference. Duration of mechanical ventilation was less with the national protocol (24 vs. 43.5 h). Significantly less amount of ASV was used with the national protocol (224 vs. 982 ml) per patient. There were no mortality or permanent neurological sequelae with either regimen.
Interpretation & conclusions:
In this preliminary study, it was found that the national ASV protocol was as effective as the conventional regimen for neurotoxic snake bites. However, the findings need to be tested in a larger randomized controlled trial for definitive conclusions.
Keywords
Low-dose anti-snake venom
mechanical ventilation
national protocol
neurotoxic
snake bite
Snake envenomation is a major health problem, particularly in rural India. Approximately 35,000-50,000 people die of snakebite every year in India1. Snakes of family Elapidae are predominantly venomous causing neurotoxic features. This family includes cobra and krait, the most common neurotoxic envenomations encountered in clinical practice.
The dosage of anti-snake venom (ASV) required to treat neurotoxic envenomation has been a subject of debate for many years. The conventional regimen for neurotoxic snake bite is to administer ASV at a dose of 100 ml every six hours till all features of envenomation resolve2. The National Snake Bite Protocol has set 200 ml ASV as the maximum dose needed to treat neurotoxic snake bite. This dose was arrived at on the basis of the average amount of venom injected per bite and the amount of antivenom needed to neutralize that amount2.
ASV is a scarce, expensive drug and should be administered only when there are definite signs of envenomation. Unbound venom can be neutralized with ASV, but once bound, the reversibility is questionable. Low-dose ASV regimens were found to be as efficacious as high-dose regimens for haemotoxic envenomations3. Adoption of the proposed national protocol will lead to significant reduction in the total dose of ASV used. However, its efficacy needs to be verified before its adoption in clinical practice. This study was undertaken to compare the efficacy of national snake bite protocol (low dose) against the efficacy of conventional (high dose) regimen.
Material & Methods
This study was conducted in the department of General Medicine, Jawaharlal Institute of Postgraduate Medical Education and Research (JIPMER), Puducherry, India, during October 2010 to April 2012. All patients who were admitted in the Emergency Medical Services (EMS) department of JIPMER, with a history of snake bite and consequent neurological manifestations were included in the study. Patients with prolonged clotting time, either at admission or at six hours after admission were excluded. Patients with any bleeding manifestations were also excluded even if their clotting time was normal. Fifty one consecutive patients who satisfied the inclusion and exclusion criteria were included. The study was approved by the institutional ethics committee.
Intervention: Patients underwent a thorough clinical examination to assess the severity of envenomation. Written informed consent was obtained either from patients or from the first-degree relative/closest related attender. Patients were divided into two groups (Figure) to receive either the conventional ASV regimen (group A, n=25) or the national ASV regimen (group B, n=26). Patients in group A received 100 ml ASV every six hours till all neurotoxic manifestations subsided. Patients in group B received 100 ml ASV at admission, followed by 100 ml at two hours if there was no improvement in neuroparalysis. Thereafter, no further ASV was given, and patients were given supportive treatment alone. Neostigmine was not administered to any patient in the study.
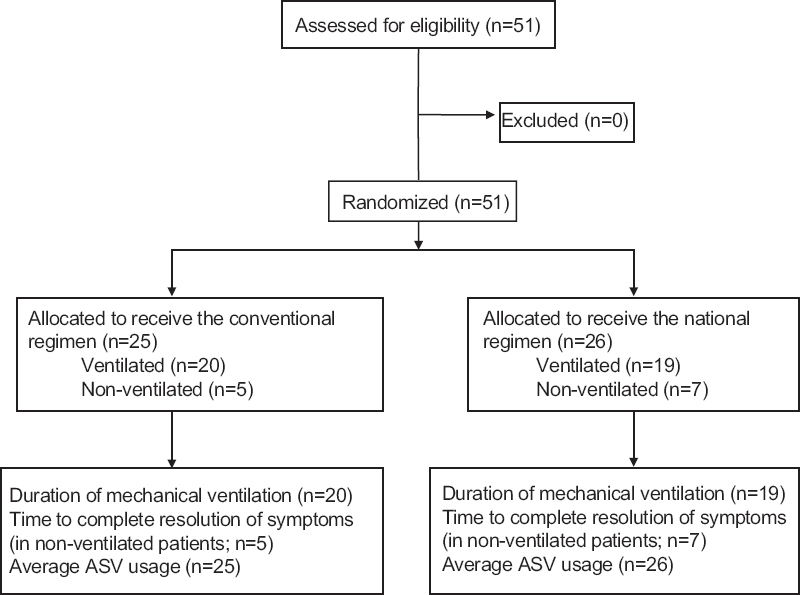
- CONSORT 2010 flow diagram showing the study design. ASV, anti-snake venom.
Outcomes: The primary outcome was the time to complete resolution of all neuroparalytic features. In case of intubated patients, the duration of ventilation was taken as the outcome measure. Secondary outcomes were the total dose of ASV used, and the complications related to envenomation (residual paralysis, hypoxic brain damage, etc.) or therapy [ventilator associated pneumonia (VAP), reactions to ASV, etc.].
Statistical analysis: Continuous data were given as means and standard deviations, and categorical data were expressed in percentages. The time to complete resolution of symptoms and the duration of mechanical ventilation were compared using Mann–Whitney test. The incidence of VAP and ASV reactions was compared using Chi-square test.
Results
There were 28 females among 51 patients (54.9%). About half the bites occurred in the early morning hours between 2400 h and 0600 h (26 patients; 50.9%). Ptosis was the most common symptom at admission occurring in 48 of 51 patients (94.1%). Twenty three patients had neuroparalysis severe enough to warrant mechanical ventilation at admission; overall, 39 patients were treated with mechanical ventilation (76.5%). Significant cellulitis at the site of bite was noted only in a minority of patients (8 of 51; 15.7%).
Twenty five patients received the conventional protocol and 26 received the national protocol. The mean age (37.96 vs. 35.42 yr) and sex distribution did not vary significantly between the groups. The mean bite-to-needle time was similar (3.46 h vs. 2.94 h). Twenty nine of 51 patients were bitten in the lower limbs. The biting species could not be identified in the majority (34/51 of patients); when identified, it was most commonly krait (10/17 patients).
Twelve patients were managed without mechanical ventilation. The average time required for complete resolution of symptoms was 1.4±1.1 days in the group B and 2.4±1.7 days in the group A. The difference was not significant (Table I).
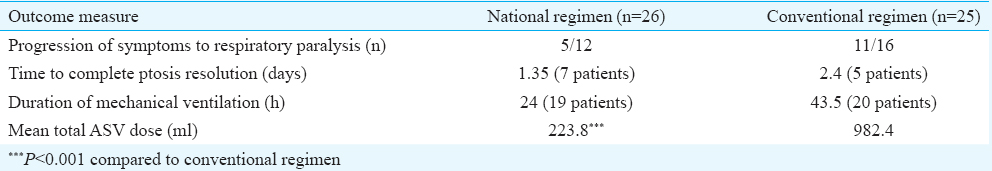
Thirty nine patients were mechanically ventilated; 19 received the national protocol and 20 received conventional protocol. There was a significant difference in the duration of mechanical ventilation between the two groups [national protocol: 24 h (6-180) vs. conventional protocol: 43.5 h (14-133); P=0.024].
An average of 223.8 ml ASV (22 vials) was used per person in the national regimen compared to 982.4 ml ASV (98 vials) in the conventional regimen. The difference in the average ASV usage between the two groups was significant (P<0.001) (Table I).
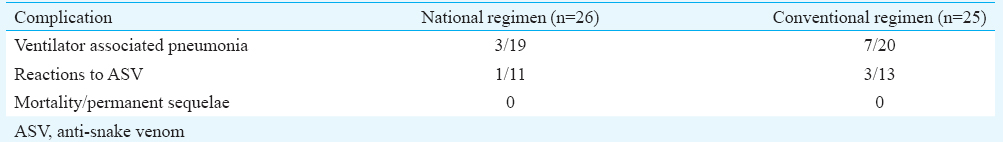
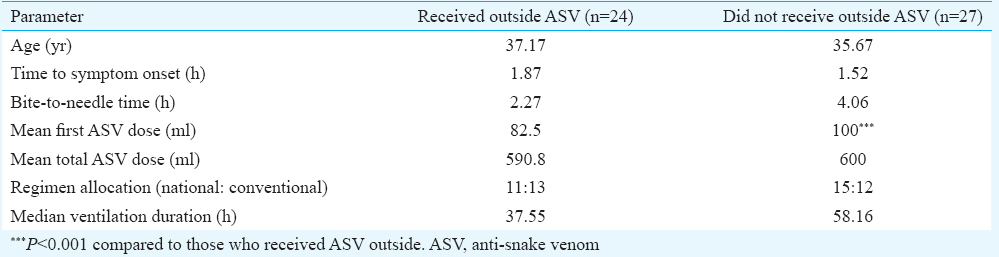
The difference in occurrence of VAP was not significant between the two groups (national regimen: 3/19 vs. conventional protocol: 7/20). There were no mortality and no permanent neurological sequelae observed with either regimen (Table II). Twenty four of 51 patients received ASV from elsewhere before referral. In a subgroup analysis comparing those patients who received ASV outside with those who did not, there was no significant difference in outcomes (Table III).
Discussion
The debate on the optimal dosage of ASV is not yet settled. A randomized controlled trial has been done to assess the optimal doses of ASV in haemotoxic envenomation4. A study by Paul et al5 concluded that while there was no additional benefit in following a high-dose regimen, there was a considerable financial gain in the low-dose regimen.
The mean bite to needle time was 3.2 h. This reflected a well-developed primary healthcare system in and around Puducherry, where ASV was administered (usually 8-10 vials) to patients with neuroparalysis at the first contact. Twenty four of 51 patients (47%) received ASV at smaller hospitals elsewhere before being referred to JIPMER. The early institution of ASV has been shown beneficial in preventing complications, whatever may be the severity of systemic envenomation67.
The proportion of patients who needed mechanical ventilation was high in this study, most likely due to referral bias, with three-fourths (76.4%) of them requiring intubation. This was comparable to another study conducted in similar urban tertiary care centres8. It was noted that those who received the national regimen progressed to require ventilation less often (5 vs. 11 patients) than those on conventional regimen. Patients who received the national regimen also had an earlier complete recovery of ptosis and significantly less duration of mechanical ventilation (24 vs. 43.5 h).
Mechanical ventilation in neurotoxic snake bite is usually short and uncomplicated, as the lungs have normal mechanics. The chances of VAP increase as the duration of ventilation increases, each having an amplifying effect on the other. Patients who received the national ASV protocol seemed to have less chances of VAP. This may represent an indirect benefit of shorter duration of ventilation achieved with national regimen. However, the numbers are too small to make any definite conclusion. ASV neutralizes the free venom in the plasma before it gets bound to tissues. Postsynaptic neurotoxicity is reversible only in the first few hours of envenomation. Thereafter, the binding becomes irreversible. Earlier administration of a higher ASV dose during this critical time period of reversible envenomation could have made the earlier recovery possible with a significantly less total ASV requirement in the national regimen group.
In a study from north India, 200 ml ASV was used as the initial bolus, which was then continued with maintenance doses of 100 ml six hourly till complete resolution of paralysis9. They concluded that the 200 ml bolus, instead of 100 ml, ‘resulted in an early recovery, a reduced total dose of ASV consumed, reduced the duration of mechanical ventilation, reduced the incidence of complications and thus was much more cost effective’. Another study from West Bengal10 compared the national protocol with a control group that received higher ASV doses. Protocol-guided treatment resulted in 66 per cent decline in the amount of ASV used, and an absolute mortality reduction of 24 per cent. In another study11, low-dose regimen (maximum 200 ml six hours apart) was compared with historical controls that received 100 ml six hourly and concluded that there was no difference in the duration of ventilation and that the low-dose regimen was equally efficacious.
Our study had some limitations. First, the total number of study participants was only 51. A sizeable proportion (47%) of patients received ASV from outside who could not be excluded from analysis. The dose of ASV received outside was variable and averaged eight vials (82.5 ml). This is less likely to have influenced the final result because the patients were almost equally distributed between the two groups with the difference being when they received the second dose of 10 vials - two hours later versus six hours later. Finally, ASV reactions were assessed only for 24 patients as this parameter was not included in the protocol initially.
In conclusion, our results show that the national ASV protocol may be as effective as the conventional regimen in treating neurotoxic snake bites. However, this being a preliminary study with a small sample size, this needs to be tested in a larger trial before definitive recommendations can be made.
Conflicts of Interest: None.
References
- World Health Organization. Rabies and envenomings: A neglected public health issue. Geneva: World Health Organization; 2007.
- Government of India. National snakebite protocol. New Delhi: Health & Family Welfare Department; 2007.
- Randomised trial of antivenom in snake envenomation with prolonged clotting time. Br Med J (Clin Res Ed). 1985;291:482.
- [Google Scholar]
- Rational use of anti-snake venom (ASV): Trial of various regimens in hemotoxic snake envenomation. J Assoc Physicians India. 2004;52:788-93.
- [Google Scholar]
- High-dose anti-snake venom versus low-dose anti-snake venom in the treatment of poisonous snake bites – A critical study. J Assoc Physicians India. 2004;52:14-7.
- [Google Scholar]
- Correlation between timing of ASV administration and complications in snake bites. J Assoc Physicians India. 2006;54:717-9.
- [Google Scholar]
- Snakebite envenoming in Kerala, South India: Clinical profile and factors involved in adverse outcomes. Emerg Med J. 2008;25:200-4.
- [Google Scholar]
- Impact of snake bites and determinants of fatal outcomes in Southeastern Nepal. Am J Trop Med Hyg. 2004;71:234-8.
- [Google Scholar]
- What dose of anti-snake venom should be given in severe neuroparalytic snake bite? Ann Thorac Med. 2011;6:47-8.
- [Google Scholar]
- A locally developed snakebite management protocol significantly reduces overall anti snake venom utilization in West Bengal, India. Wilderness Environ Med. 2008;19:267-74.
- [Google Scholar]
- Low dose of snake antivenom is as effective as high dose in patients with severe neurotoxic snake envenoming. Emerg Med J. 2005;22:397-9.
- [Google Scholar]






